Original article
Angiography-derived index versus fractional flow reserve for intermediate coronary lesions: a meta-analysis review
Índice derivado de la angiografía frente a reserva fraccional de flujo en lesiones coronarias intermedias. Revisión de metanálisis
aDepartamento de Cardiología, Hospital Clínico Universitario de Valladolid, Valladolid, Spain bCentro de Investigación Biomédica en Red de Enfermedades Cardiovasculares (CIBERCV), Instituto de Salud Carlos III, Madrid, Spain
ABSTRACT
Introduction and objectives: Transcatheter aortic valve implantation (TAVI) has revolutionised the treatment of severe symptomatic aortic stenosis, providing an alternative to surgical valve aortic replacement, especially in high-risk patients. Despite its benefits, significant interregional variability in TAVI access persists within Spain. This study aimed to analyse disparities in TAVI implementation across different autonomous communities, identifying the key factors underlying this variability.
Methods: We conducted a retrospective observational study using data from the Spanish National Registry of Specialized Care Activity Minimum Basic Data Set for 2016–2023, including all TAVI performed in Spain. Additionally, a survey was distributed among specialists from 123 centres to assess the factors influencing clinical decision-making, barriers to access, and resource availability.
Results: Although the number of TAVI increased across all regions, significant differences were observed in the implantation rates (between 0.63 and 2.28 per 10 000 inhabitants). Survey responses indicated that the primary determinants for TAVI indication were heart team judgment (40.0%) and patient risk stratification (36.5%). The main barriers to expanding TAVI access included rigid patient stratification (25.6%), insufficient early detection (17.8%), and resource limitations (13.3%). Participants emphasized the need for better coordination among health care levels and establishing uniform access criteria.
Conclusions: Although TAVI adoption has increased in Spain, significant regional disparities remain, suggesting factors beyond economics contribute to access variability. Addressing these inequalities requires enhanced coordination across different health care levels, optimized resource allocation, and refined patient selection strategies.
Keywords: Transcatheter aortic valve implantation. Aortic valve stenosis. Health inequities. Health services accessibility. Delivery of health care.
RESUMEN
Introducción y objetivos: El implante percutáneo de válvula aórtica (TAVI) ha revolucionado el tratamiento de la estenosis aórtica grave sintomática, ofreciendo una alternativa al reemplazo quirúrgico, en especial en pacientes de alto riesgo. A pesar de sus beneficios, persiste una significativa variabilidad interregional en el acceso al TAVI en España. Este estudio tuvo como objetivo analizar las disparidades en la implementación del TAVI entre las distintas comunidades autónomas, e identificar los factores determinantes de la variabilidad.
Métodos: Se realizó un estudio observacional retrospectivo con datos del Registro de Actividad de Atención Especializada Conjunto Mínimo Básico de Datos para el periodo 2016-2023, abarcando todos los procedimientos de TAVI realizados en España. Además, se distribuyó una encuesta entre especialistas de 123 centros para evaluar los factores que pueden influir en la toma de decisiones clínicas, las barreras de acceso y la disponibilidad de recursos.
Resultados: El número de procedimientos de TAVI aumentó en todas las regiones, pero se observaron diferencias significativas en las tasas de implantación, que se situaron entre 0,63 y 2,28 por 10.000 habitantes. Las respuestas de la encuesta indicaron que los principales determinantes para la indicación de TAVI fueron el criterio del equipo médico (40,0%) y la estratificación del riesgo del paciente (36,5%). Las principales barreras para incrementar el acceso al TAVI incluyeron la estratificación rígida de los pacientes (25,6%), la detección temprana insuficiente (17,8%) y las limitaciones de recursos (13,3%). Los participantes subrayaron la necesidad de mejorar la coordinación entre los niveles asistenciales y la estandarización de los criterios de acceso.
Conclusiones: Aunque la adopción del TAVI en España ha crecido, persisten importantes disparidades regionales que no pueden explicarse únicamente por factores económicos. Para abordar estas desigualdades es necesario mejorar la coordinación entre niveles asistenciales, optimizar la asignación de recursos y perfeccionar las estrategias de selección de pacientes.
Palabras clave: Implante percutáneo de válvula aórtica. Estenosis de válvula aórtica. Inequidades en salud. Accesibilidad de los servicios de salud. Atención a la salud.
Abbreviations
AC.: autonomous communities. AS: aortic stenosis. SNS: Spanish National Health Service. TAVI: transcatheter aortic valve implantation.
INTRODUCTION
Aortic stenosis (AS) is the most common valvular heart disease, with a prevalence of 3% in individuals older than 65 years and 7.4% in those older than 85 years. AS is more common in men.1,2 It is the leading cause of valve surgery in the adult population,3 and is associated with risk factors such as advanced age.4,5 Although aortic stenosis typically develops after age 60, symptoms usually present between ages 70 and 80; once symptoms occur, the mortality rate may reach 50% within the next few years.4,6
Transcatheter aortic valve implantation (TAVI), initially reserved for patients deemed ineligible for surgical aortic valve replacement,7-11 was subsequently expanded to include those at intermediate risk and, more recently, patients at low risk.5,12-14
In Spain, the use of TAVI has increased,5 reflecting its growing acceptance within the Spanish National Health System (SNS), largely attributable to improved clinical and economic outcomes.5,15 Multiple studies have demonstrated the benefits of TAVI, including significant improvements in quality of life,16,17 lower rates of major complications,18 and reduced mortality.5,19,20
Nationwide, improvements in TAVI outcomes, shorter lengths of stay, and lower mortality rates have been reported. Furthermore, autonomous communities (AC) with higher implant volumes have a better safety and efficacy profile, lower risks of infection, reduced need for permanent pacemaker implantation, and shorter lengths of stay.5 However, the distribution of TAVI reveals notable interregional disparities, with procedural rates varying considerably according to hospital resources and volumes.21
Despite these advances, in Spain, TAVI use remains significantly lower compared with other European countries.22 Furthermore, Spain exhibits one of the highest variations in access and utilization rates among its AC (42%), which cannot be explained solely by economic differences, hospital utilization, or observed mortality.21 An analysis by de la Torre Hernández et al.21 described the need for strategies to promote equity in TAVI access across Spain.
This study analyzed heterogeneity in the use of TAVI across AC (2016–2023) and identified the factors associated with this inequality.
METHODS
TAVI data in Spain from 2016 through 2023
Data on TAVI performed from 2016 to 2023 were obtained from the Specialized Care Activity Minimum Basic Data Set23-25 using the International Classification of Diseases, 10th revision for Spain (ICD-10-ES) (supplementary data 1). This mandatory registry, which includes all specialized care centers, is managed by the Spanish Ministry of Health and ensures strict compliance with privacy and data protection standards. The analysis included all TAVI performed in public and private hospitals across AC.
Survey
Simultaneously, we designed a survey to gather information on therapeutic decision-making in patients with AS to identify possible factors influencing TAVI implementation and interregional variability previously observed. This survey was distributed to department heads of the 123 medical centers affiliated with the Interventional Cardiology Association of the Spanish Society of Cardiology. Respondents were asked to extend the invitation to other department members to ensure representative and diverse responses.
The survey (supplementary data 2) covered clinical, structural, organizational, and patient-related aspects relevant to clinical practice during the study period, and was structured into 3 thematic blocks:
- – Center and participant characteristics (questions A1–C3): evaluation of institutional context and department composition, including variables such as the respondent’s specialty and annual budget allocation.
- – Patient selection and decision-making (questions C4–E2): identification of key clinical and demographic factors influencing therapeutic choice, as well as barriers and determinants shaping clinical team decisions.
- – Center evaluation and TAVI use (questions E3–F9): assessment of clinician perception and satisfaction regarding TAVI, and exploration of adoption, implementation, and geographic distribution of this strategy.
Responses were analyzed descriptive and qualitatively, allowing a comprehensive interpretation of factors influencing TAVI implementation and interregional heterogeneity.
RESULTS
TAVI in 2016–2023
The results of TAVI interventions, expressed as the number of cases and intervention rates per 10 000 inhabitants, are shown in figure 1. All AC experienced an increase in procedures during the study period (figure 1A), with the greatest growth observed in the Canary Islands (33 cases in 2016 and 368 in 2023) and La Rioja (2 cases in 2016 and 28 in 2023), corresponding to increases of 1.115% and 1.400%, respectively. The AC with the highest number of TAVI performed in 2023 were Andalusia (n = 1392), Catalonia (n = 1245), and the Community of Madrid (n = 1257). La Rioja had the fewest (2 cases in 2016, 28 in 2023).
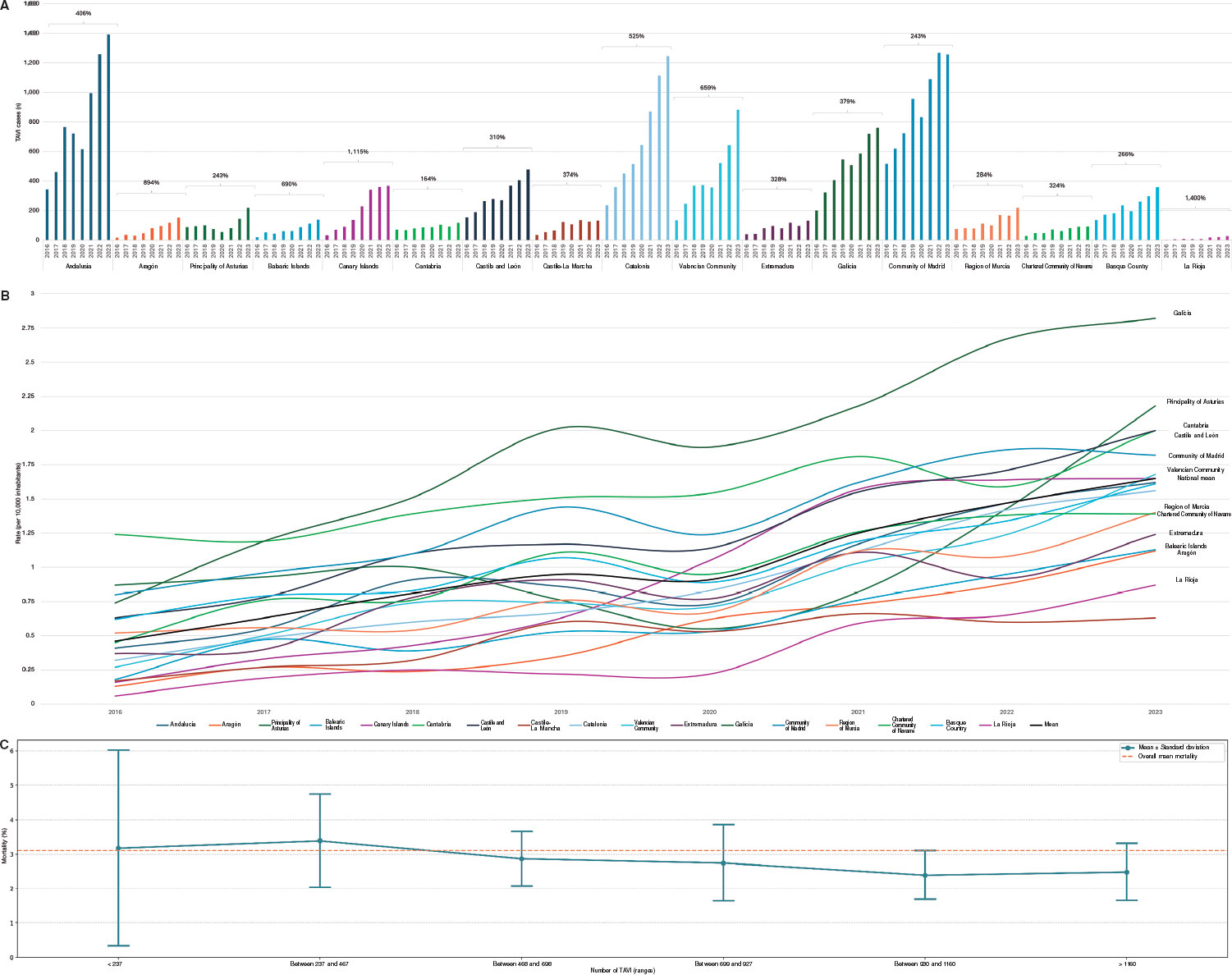
Figure 1. A: total number of transcatheter aortic valve implantation (TAVI) cases by autonomous community and year (2016–2023). B: population-adjusted procedural rates adjusted (per 10 000 inhabitants) by autonomous community and year (2016–2023). C: mean and dispersion of mortality based on the number of TAVI.
Procedure rates (figure 1B) indicated that, in 2023, the AC with the highest per capita TAVI volumes were Galicia (2.82 per 10 000 inhabitants), Asturias (2.18 per 10 000), Cantabria (2.00 per 10 000), Castile and León (2.00 per 10 000), and Madrid (1.82 per 10 000), all above the national average (1.65 per 10 000). The lowest per capita TAVI volumes were found in Extremadura (1.24 per 10 000), the Balearic Islands (1.13 per 10 000), Aragón (1.12 per 10 000), La Rioja (0.87 per 10 000), and Castile-La Mancha (0.63 per 10 000).
The mean in-hospital mortality rate during the study period was 3.07% (figure 1C).
Survey
Center and participant characteristics
The survey was completed by 26 specialists with different TAVI-related profiles: 18 in interventional cardiology, 7 in clinical cardiology, and 1 in cardiac imaging, including 4 heads of cardiac surgery departments and 18 cath lab directors. The respondents’ mean professional experience was 26.5 years (range, 9–41 years) and worked in hospitals with a mean TAVI experience of 10.6 years (range, 1–16 years). Responses were obtained from hospitals in 11 of the 17 AC (64.7% of the national territory). Team composition by professional profile is provided in supplementary data 3.
Teams performed a mean of 76 TAVI (range, 0–148) in 2021 and 95 (range, 0–254) in 2022, with marked variation across hospitals. Annual budgets allocated to units ranged from €474 765 to €25 111 709, reflecting wide disparities in resource availability. Despite these differences, most respondents reported being satisfied with the extent to which purchasing committees allocated budgets to meet their teams’ clinical needs (19.2%, very satisfied; 42.3%, quite satisfied; 34.6%, moderately satisfied; 3.9%, unsatisfied).
Most participants rated continuity of care across different settings as good or improvable (54.9% and 38.5%, respectively) and gave examples of best practices as well as areas for improvement. Best practices included teleconsultation, specialized programs such as TAVI Nurse,26 periodic cross-level meetings, and shared protocols between primary and hospital care. Suggested improvements included insufficient coordination between primary and specialized care, overloaded schedules, and the need to improve clinical information systems such as integrating joint activities.
Patient selection and decision-making
The clinical indication for TAVI was determined primarily by heart team judgment (40.0%) and patient stratification (36.5%), followed by patient preference (12.5%) and resource availability (10.4%). Barriers to expanding TAVI included rigid patient stratification (25.6%), insufficient early detection (17.8%), intra-team discrepancies (14.2%), insufficient budget (13.3%) and technology (11.8%), and obstacles to multidisciplinary team integration (7.4%).
Most centers had decision-support tools for TAVI (76.9%) and specific training programs (65.4%). Tools included decision algorithms, clinical practice guidelines, consensus protocols, and software for anatomical, feasibility, and comorbidity assessment. Specific training and periodic multidisciplinary meetings were also in place.
Most centers (76.9%) conducted periodic evaluations of outcomes—described as continuous process evaluation—to optimize procedures, including registries, internal audits, analysis of complications, in-hospital mortality, and readmissions. Annual and monthly clinical meetings allowed protocol adjustments and improved care processes, with high adherence to international clinical practice guidelines.
On the other hand, respondents indicated limited satisfaction with information exchange among departments and specialists involved in TAVI decision-making (figure 2A).
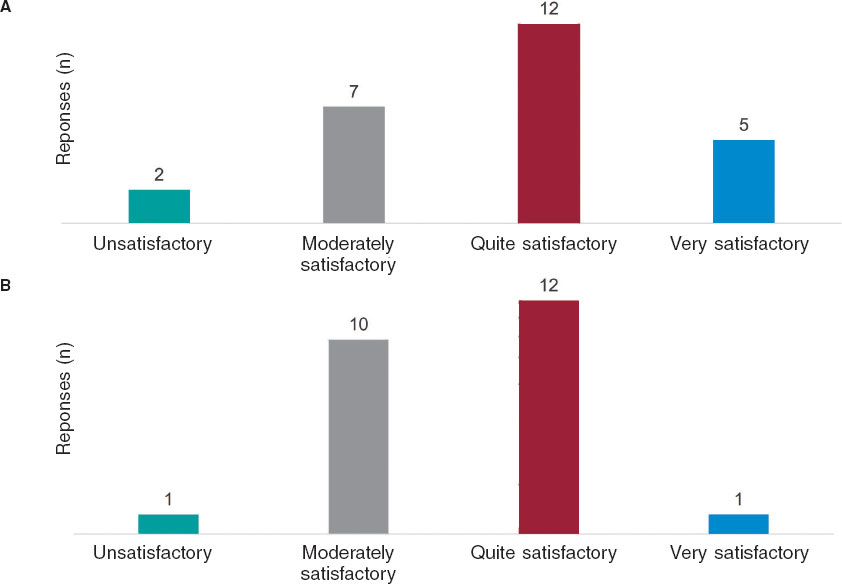
Figure 2. A: respondents’ evaluation of information exchange across departments, committees, and professionals involved in decision-making for aortic valve replacement. B: respondents’ evaluation of information exchange and best practices across centers performing transcatheter aortic valve implantation in Spain.
The survey on patient profiles treated with TAVI, which is performed primarily in intermediate- and high-risk patients, showed that 96.2% of centers treat high-risk patients; 76.9%, intermediate-risk patients; and only 30.8%, low-risk patients. In general, although no major barriers to treatment based on risk profile were reported (69.3% responded negatively), some resistance from cardiac surgery (n = 5), disagreement with institutional protocols (n = 4), and infrastructure limitations expressed as restricted availability of cath labs (n = 3) were noted.
Similarly, respondents perceived that the professional background of team members influences clinical decision-making for TAVI (63.6% strongly agreed and 27.3% moderately agreed; n = 11), highlighting the importance of training, experience, and individual performance. Multidisciplinary, consensus-based decisions among specialists in clinical cardiology, imaging, interventional cardiology, and cardiac surgery allow for the consideration of specific anatomic and clinical factors. Although such multidisciplinary teams promote more objective decision-making, participation from cardiac surgery may affect the indication in low-risk patients.
Therefore, participants considered the heart team’s judgment on additional factors in the indication for TAVI to be relevant, rating it as fairly (50%) or very relevant (50%). Similarly, respondents reported overall satisfaction with the process by which clinical decisions were made within the team: 53.8% found it fairly satisfactory; 38.5%, very satisfactory; 7.7%, moderately satisfactory.
There was near-unanimous agreement (96%) on the importance of incorporating the patient’s opinion into the decision-making process for TAVI indication. When ranking the key factors guiding clinical decision-making, comorbidity and age stratification were rated as the most relevant (figure 3).
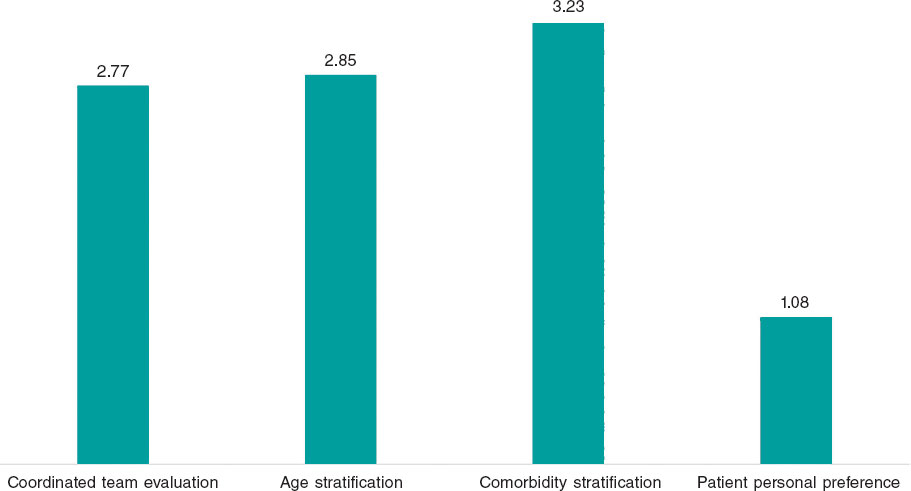
Figure 3. Weighted average of responses ranking factors by relevance in the clinical decision to indicate transcatheter aortic valve implantation.
The leading criteria for inclusion on the TAVI waiting list were the presence of comorbidities (n = 22), clinical status or overall risk (n = 20), followed by the minimum (n = 17) and maximum age threshold (n = 2).
The mean waiting time for the procedure was approximately 2 months (mean, 1.92 months; range, 0–4 months). Compared with surgical aortic valve replacement, the waiting list was generally perceived as shorter (50.0%) or equivalent (26.9%).
The primary factors influencing waiting time for TAVI were the need for computed tomography (n = 7) and cath lab availability (n = 5). Other factors included computed tomography availability (n = 3), anesthesia availability (n = 3), and waiting list length (n = 2). In line with this, respondents indicated that most patients (88.5%) undergo TAVI as scheduled procedures
Center evaluation and TAVI use
Most respondents considered the number of centers performing TAVI in Spain sufficient (n = 18, 24 respondents) and highlighted the importance of ensuring adequate procedural volume per center to optimize outcomes and minimize complications. Strengthening infrastructure, human resources, and networking was considered essential, prioritizing quality and safety over opening new centers.
Likewise, participants were generally satisfied with the exchange of information and best practices among TAVI centers in Spain (figure 2B).
There was consensus that improving the early detection of AS would, in turn, improve outcomes and patient experience (91.7%; n = 24). Conversely, most considered that regulatory thresholds for accrediting centers would not substantially affect total TAVI volume (62.5%; n = 24).
Finally, participants shared additional considerations. They emphasized prioritizing safety and clinical outcomes in TAVI programs beyond simply increasing the number of available centers. Although concentration of procedures in high-volume centers was suggested to improve health outcomes, it could also reduce the total number of procedures. The need for audits and dissemination of risk-adjusted results was highlighted to ensure transparency and care quality. Lastly, concern was expressed about the impact of health system fragmentation on equity of access.
DISCUSSION
The present study confirms the upward trend in TAVI implantation in Spain, which is consistent with previous research.5,22 From 2016 through 2023, the number of procedures increased in all AC, reflecting broader acceptance of this technique within the SNS. This trend is attributed to the consolidation of TAVI as a reference therapeutic alternative for the treatment of severe symptomatic AS, progressively expanding from high-risk to intermediate- and low-risk patients.12-14
Despite this generalized increase, results show notable interregional variability in TAVI rates. In 2023, some AC reported procedural rates well above the national average, while others were considerably lower. This inequality has been documented previously and suggests a key role for organizational factors in determining access to the procedure.21 Of note, in regions such as La Rioja, the absence of local cardiac surgery centers may partly explain the low number of TAVI. However, this does not mean that patients are not treated; rather procedures are performed in neighboring AC.
From a clinical perspective, multiple studies have shown that TAVI reduces in-hospital mortality, improves quality of life, and decreases the rate of major complications.16-20 Although these outcomes were not directly assessed in the present study, former studies have identified a relationship between higher procedural volume and improved outcomes, including reduced infection risk, decreased pacemaker need, and a shorter length of stay.5 Our analysis does not allow a direct correlation to be established between procedural volume and quality of care in Spain. This suggests that, although cumulative experience is a determinant of improved outcomes, other organizational and resource-management factors may also contribute to the observed discrepancies. Nonetheless, our findings indicate that as TAVI volume increases, the variability in mortality outcomes tends to diminish, suggesting greater standardization of practice and reduced variability across more experienced centers.
The survey analysis revealed that TAVI indication in Spain continues to depend primarily on physician judgment and patient risk stratification, with less influence from patient preference or resource availability. These findings are consistent with former studies underscoring the importance of multidisciplinary clinical judgment in decision-making, which results in patient selection aligned with clinical practice guidelines and safety criteria.27 However, organizational barriers hindering the expansion of TAVI were identified, including rigid patient stratification, insufficient identification of candidates, and difficulties integrating heart teams. Such limitations have previously been recognized as determinants of inequality in TAVI access in Spain,21 reinforcing the need for strategies to optimize care.
From a financial perspective, TAVI has been shown to be cost-effective compared with conventional surgical aortic valve replacement across various clinical scenarios.15,28 In our study, however, participants did not identify financing as a major barrier to expansion. This finding is consistent with prior Spanish investigations, which found no clear correlation between regional health spending and TAVI rates,5,21 suggesting that variability is more strongly influenced by organizational rather than economic factors.
The perception of infrastructure is relevant too, as most respondents considered the number of centers performing TAVI in Spain sufficient, while emphasizing the importance of guaranteeing a minimum procedural volume per center to optimize outcomes and minimize complications. Former studies have highlighted that cumulative team experience can improve clinical outcomes.27 However, no consensus was reached in this study on whether concentrating procedures in a smaller number of centers would favor equity of access or, conversely, limit availability in regions with restricted supply.
With respect to continuity of care, both advances and opportunities for improvement were identified. While > 90% of specialists positively evaluated the implementation of teleconsultation, specialized nursing programs (TAVI Nurse26), and shared protocols across levels of care, participants also emphasized the need to strengthen coordination between primary and specialized care, improve clinical information systems, and optimize scheduling management. These aspects have previously been highlighted as important for improving the efficiency of TAVI care processes5 and identified as cross-cutting priorities in the 2022 report of the SNS, Estrategia en Salud Cardiovascular.29
Limitations
This study has certain limitations. First, although the analysis of the Specialized Care Activity Minimum Basic Data provides information on overall TAVI trends, the Spanish Ministry of Health’s statistical portal does not include detailed patient-level clinical data, thus preventing assessment of outcomes such as complications.
Second, although the survey was designed to achieve representation from all AC, responses were obtained from only 11 of them (26 of 123 [21%] affiliated centers of the Interventional Cardiology Association), meaning that the perceptions and experiences reflected are drawn from a subset of regions, which may influence interpretation of certain findings. Nevertheless, this limitation is inherent to survey-based research, as participation greatly depends on availability and willingness of respondents. Despite this, the sample offers a representative perspective on organizational and clinical factors influencing variability in TAVI access within the SNS.
Finally, sex and gender variables were not considered in accordance with the SAGER guidelines, as the focus was on regional differences across AC. Future studies should explore sex- and gender-related influences on TAVI implementation.
CONCLUSIONS
Our findings reflect sustained growth in TAVI implementation in Spain, alongside marked interregional variability in procedural rates. Patient selection is driven primarily by physician judgment and clinical risk, while barriers to expansion are more organizational than financial. Key strategies are suggested to reduce regional variability and ensure equitable TAVI access within the SNS, including improved coordination across different levels of care, standardization of selection criteria, and strengthened resource management.
FUNDING
This work was funded by Edwards Lifesciences.
ETHICAL CONSIDERATIONS
Approval from the study ethics committee was deemed unnecessary, as it used administrative data from the Spanish Ministry of Health without accessing patient-level data. Similarly, informed consent was deemed unnecessary. Sex and gender variables were not analyzed in accordance with the SAGER guidelines, as the study focused on regional differences across AC.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCE
Artificial intelligence was not used in this study.
AUTHORS’ CONTRIBUTIONS
All authors were involved in the study design. A. Morán-Aja, O. Martínez-Pérez, M. Cerezales, and J. Cuervo requested the data and implemented the web-based survey. O. Martínez-Pérez conducted data analysis. All authors reviewed and validated the results. A. Morán-Aja, O. Martínez-Pérez, M. Cerezales, and J. Cuervo drafted the manuscript. All authors reviewed and approved the final version.
CONFLICTS OF INTEREST
J.M. de la Torre-Hernández is editor-in-chief of REC: Interventional Cardiology; the journal’s editorial procedure to ensure impartial handling of the manuscript. A. Morán-Aja, O. Martínez-Pérez, M. Cerezales, and J. Cuervo work for Axentiva Solutions S.L., a consultancy providing services to various pharmaceutical and medical device companies.
ACKNOWLEDGMENTS
The authors thank the Research Agency and Scientific Department of the Spanish Society of Cardiology for their support in project management and securing funding. Their collaboration was essential to the planning and execution of this study, enabling data analysis and evaluation of regional variability in TAVI implementation in Spain.
WHAT IS KNOWN ABOUT THE TOPIC?
- TAVI has revolutionized the treatment of severe AS, becoming a first-line option in high- and intermediate-risk patients. It has demonstrated advantages over conventional surgery, including reduced mortality, a shorter length of stay, and improved quality of life. In Spain, TAVI use has grown unevenly across AC, influenced not only by economic factors but also by organizational and structural differences in patient selection criteria and resource availability. However, the impact of this variability on clinical outcomes and equity of access remains unclear.
WHAT DOES THIS STUDY ADD?
- This study provides a comprehensive analysis of interregional variability in TAVI implementation in Spain, combining the Specialized Care Activity Minimum Basic Data Set with a specialist survey. Compared with former studies, it not only identifies differences in implementation rates across AC but also organizational, structural, and care-related barriers influencing access. Furthermore, it evaluates professional perceptions of team composition in clinical decision-making and challenges in continuity of care. These findings improve understanding of the determinants of heterogeneity in TAVI access and offer recommendations to enhance equity of implementation within the SNS. Results may be key for health policy planning and the design of strategies to optimize resource allocation and ensure more uniform access to this technology.
REFERENCES
1. Ferreira-González I, Pinar-Sopena J, Ribera A, et al. Prevalence of calcific aortic valve disease in the elderly and associated risk factors:a popula- tion-based study in a Mediterranean area.
2. Stewart BF, Siscovick D, Lind BK, et al. Clinical Factors Associated With Calcific Aortic Valve Disease.
3. Salinas P, Moreno R, Calvo L, et al. Long-term Follow-up After Transcath- eter Aortic Valve Implantation for Severe Aortic Stenosis.
4. Otto CM, Lind BK, Kitzman DW, Gersh BJ, Siscovick DS. Association of Aortic-Valve Sclerosis with Cardiovascular Mortality and Morbidity in the Elderly.
5. Íñiguez-Romo A, Zueco-Gil JJ, Álvarez-BartoloméM, et al. Outcomes of transcatheter aortic valve implantation in Spain through the Activity Registry of Specialized Health Care.
6. Ramaraj R, Sorrell VL. Degenerative aortic stenosis.
7. Van Hemelrijck M, Taramasso M, De Carlo C, et al. Recent advances in understanding and managing aortic stenosis.
8. Maldonado Y, Baisden J, Villablanca PA, Weiner MM, Ramakrishna H. General Anesthesia Versus Conscious Sedation for Transcatheter Aortic Valve Replacement —An Analysis of Current Outcome Data.
9. Perrin N, Frei A, Noble S. Transcatheter aortic valve implantation:Update in 2018.
10. Leon MB, Smith CR, Mack M, et al. Transcatheter Aortic-Valve Implanta- tion for Aortic Stenosis in Patients Who Cannot Undergo Surgery.
11. Duncan A, Ludman P, Banya W, et al. Long-Term Outcomes After Tran- scatheter Aortic Valve Replacement in High-Risk Patients With Severe Aortic Stenosis.
12. Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease.
13. Mack MJ, Leon MB, Thourani VH, et al. Transcatheter Aortic-Valve Replacement with a Balloon-Expandable Valve in Low-Risk Patients.
14. Popma JJ, Deeb GM, Yakubov SJ, et al. Transcatheter Aortic-Valve Replace- ment with a Self-Expanding Valve in Low-Risk Patients.
15. Pinar E, de Lara JG, Hurtado J, et al. Cost-effectiveness analysis of the SAPIEN 3 transcatheter aortic valve implant in patients with symptomatic severe aortic stenosis.
16. Tamm AR, Jobst ML, Geyer M, et al. Quality of life in patients with transcatheter aortic valve implantation:an analysis from the INTERVENT project.
17. Nuland PJA, van Ginkel DJ, Overduin DC, et al. The impact of stroke and bleeding on mortality and quality of life during the first year after TAVI:A POPular TAVI subanalysis.
18. Zhang S, Kolominsky-Rabas PL. How TAVI registries report clinical outcomes —A systematic review of endpoints based on VARC-2 definitions.
19. Gargiulo G, Sannino A, Capodanno D, et al. Transcatheter Aortic Valve Implantation Versus Surgical Aortic Valve Replacement.
20. Sehatzadeh S, Doble B, Xie F, et al. Transcatheter aortic valve implantation (TAVI) for treatment of aortic valve stenosis:an evidence update.
21. la Torre Hernández JM, Lozano González M, García Camarero T, et al. Interregional variability in the use of cardiovascular technologies (2011- 2019). Correlation with economic indicators, admissions, and in-hospital mortality.
22. Biagioni C, Tirado-Conte G, Nombela-Franco L, et al. Situación actual del implante transcatéter de válvula aórtica en España.
23. Ministerio de Sanidad. Registro de Actividad de Atención Especializada, Conjunto Mínimo Básico de Datos. Available at:https://www.sanidad. gob.es/estadEstudios/estadisticas/cmbdhome.htm. Accessed 8 Apr 2024.
24. Ministerio de Sanidad. Registro de Actividad de Atención Sanitaria Espe- cializada (RAE-CMBD). Actividad y resultados de la hospitalización en el SNS. Año 2022. Madrid:Ministerio de Sanidad;2024. Available at:https://www.sanidad.gob.es/estadEstudios/estadisticas/docs/RAE-CMBD_Informe_Hospitalizacion_2022.pdf. Accessed 29 May 2025.
25. Ministerio de Sanidad. Registro de Atención Sanitaria Especializada RAE-CMBD. Manual de Usuario y Glosario de Términos. Portal Estadístico;2023. Available at:https://pestadistico.inteligenciadegestion.sanidad.gob. es/publicoSNS/D/rae-cmbd/rae-cmbd/manual-de-usuario/manual-de-usuario- rae. Accessed 29 May 2025.
26. González Cebrián M, Valverde Bernal J, Bajo Arambarri E, et al. Docu- mento de consenso de la figura TAVI Nurse del Grupo de Trabajo de Hemodinámica de la Asociación Española de Enfermería en Cardiología.
27. Carnero-Alcázar M, Maroto-Castellanos LC, Hernández-Vaquero D, et al. Isolated aortic valve replacement in Spain:national trends in risks, valve types, and mortality from 1998 2017.
28. Baron SJ, Magnuson EA, Lu M, et al. Health Status After Transcatheter Versus Surgical Aortic Valve Replacement in Low-Risk Patients With Aortic Stenosis.
29. Ministerio de Sanidad. Estrategia en Salud Cardiovascular del Sistema Nacional de Salud (ESCAV). 2022. Available at:https://www.sanidad.gob. es/areas/calidadAsistencial/estrategias/saludCardiovascular/docs/Estrategia_de_salud_cardiovascular_SNS.pdf. Accessed 29 May 2025.
ABSTRACT
Introduction and objectives: Thrombus removal in patients with ST-segment elevation myocardial infarction (STEMI) undergoing percutaneous coronary intervention (PCI) can be challenging in the presence of a large thrombus burden. Excimer laser coronary angioplasty (ELCA) is an adjuvant device capable of vaporizing thrombus. This study aimed to evaluate the safety and efficacy profile of ELCA in PCI.
Methods: Patients with STEMI undergoing PCI with concomitant use of ELCA for thrombus removal were retrospectively identified at our center. Data were collected on the device efficacy and its contribution to overall procedural success. Additionally, ELCA-related complications and major adverse cardiovascular events were recorded at a 2-year follow-up.
Results: ELCA was used in 130 STEMI patients, 124 (95.4%) of whom had a large thrombus burden. TIMI grade flow improved significantly after ELCA: before laser application, TIMI grade-0 flow was reported in 79 (60.8%) cases and TIMI grade-1 flow in 32 (24.6%) cases. After ELCA, TIMI grade-2 and 3 flows were achieved in 45 (34.6%) and 66 (50.8%) cases, respectively (P < .001). Technical and procedural success were achieved in 128 (98.5%) and 124 (95.4%) cases, respectively. The complications included 1 death at the cath lab (0.8%), 1 coronary perforation (0.8%), and 3 distal embolizations (2.3%). At the 2-years follow-up, major adverse cardiovascular events occurred in 18.3% of the population.
Conclusions: In the context of STEMI, ELCA seems to be an effective device for thrombus dissolution, with adequate technical and procedural success rates. In the present cohort, ELCA use was associated with a low complication rate and favorable long-term outcomes.
Keywords: Acute coronary syndrome. Thrombectomy. Excimer laser coronary angioplasty.
RESUMEN
Introducción y objetivos: La eliminación de trombos durante la intervención coronaria percutánea primaria (ICPp) en el infarto agudo de miocardio con elevación del segmento ST (IAMCEST) es un desafío en presencia de una carga trombótica elevada. La angioplastia coronaria con láser de excímeros (ELCA) es una técnica complementaria que permite vaporizar el trombo. Este estudio evaluó la eficacia y la seguridad de la ELCA en el contexto de la ICPp.
Métodos: Análisis retrospectivo unicéntrico de pacientes con IAMCEST sometidos a ICPp con ELCA. Se evaluaron la eficacia en la disolución del trombo, la mejoría del flujo, el éxito del procedimiento, las complicaciones asociadas y los acontecimientos cardiovasculares adversos mayores durante un seguimiento de 2 años.
Resultados: Se realizó ELCA en 130 pacientes con IAMCEST, de los cuales 124 (95,4%) tenían carga trombótica elevada. El flujo TIMI mejoró significativamente tras la ELCA: previamente era 0 en 79 casos (60,8%) y 1 en 32 casos (24,6%), y se lograron flujos TIMI 2 y 3 en 45 casos (34,6%) y 66 casos (50,8%), respectivamente (p < 0,001). Las tasas de éxito técnico y del procedimiento fueron del 98,5% y el 95,4%, respectivamente. Las complicaciones incluyeron 1 muerte intraprocedimiento (0,8%), 1 perforación coronaria (0,8%) y 3 embolizaciones distales (2,3%). A los 2 años, la tasa de acontecimientos cardiovasculares adversos mayores fue del 18,3%.
Conclusiones: La ELCA parece ser una técnica eficaz y segura en el IAMCEST para la disolución del trombo, con altas tasas de éxito técnico y procedimental, baja incidencia de complicaciones y resultados favorables a largo plazo.
Palabras clave: Síndrome coronario agudo. Trombectomía. Angioplastia coronaria con láser de excímeros.
Abbreviations
ELCA: excimer laser coronary angioplasty. LTB: large thrombus burden. MACE: major adverse cardiovascular events. PCI: percutaneous coronary intervention. STEMI: ST-segment elevation myocardial infarction. TIMI: Thrombolysis in Myocardial Infarction.
INTRODUCTION
In patients with ST-segment elevation myocardial infarction (STEMI), percutaneous coronary intervention (PCI) is the preferred reperfusion strategy, as long as it can be performed within 120 minutes of the electrocardiogram-based diagnosis.1 Many patients with STEMI present with thrombotic occlusion of the infarct-related artery. Therefore, the use of devices aimed at reducing thrombus burden is a reasonable consideration to minimize distal embolization and no-reflow. Persistent no-reflow in patients with STEMI undergoing PCI is associated with the worst in-hospital outcomes and increased long-term mortality.2
While early studies on manual thrombus aspiration suggested benefits in terms of improved myocardial blush grades and ST-segment elevation resolution,3 larger trials comparing manual thrombus aspiration with PCI alone showed no significant reduction in cardiovascular death, recurrent myocardial infarction, cardiogenic shock, or a New York Heart Association FC IV heart failure within 180 days.4 Consequently, routine aspiration thrombectomy is no longer recommended in patients with STEMI.5
Thrombus removal, particularly when dealing with a large thrombus burden (LTB) in the context of STEMI, remains a critical and sometimes challenging aspect of PCI. Excimer laser coronary angioplasty (ELCA Coronary Laser Atherectomy Catheter, Koninklijke Philips N.V., The Netherlands) is a well-established adjuvant therapy for coronary interventions. ELCA uses xenon-chloride gas as the lasing medium to produce UV light energy, which is delivered to the target site through an optical fiber. This energy has the ability to ablate inorganic material through photochemical, photothermal, and photomechanical mechanisms.6,7 The microparticles released during laser ablation measure < 10 µm and are absorbed by the reticuloendothelial system, theoretically reducing the risk of microvasculature obstruction.8 These unique characteristics of ELCA have facilitated its use as an adjuvant therapy in patients with STEMI to ablate and remove thrombus.
Although ELCA is part of the therapeutic armamentarium in some PCI-capable centers, literature data is limited on its safety and efficacy profile in this specific scenario. The aim of this study was to evaluate the contribution of ELCA, focusing on its safety and efficacy profile as an adjuvant therapy in patients with STEMI undergoing PCI in our center.
METHODS
Data from all patients undergoing PCI with the simultaneous use of ELCA as an adjuvant technique were retrospectively recorded in a dedicated database after each procedure, starting from the introduction of the device in our center. ELCA procedures were performed by 5 interventional cardiologists with dedicated training in the use of the device.
This study was approved by Parque Sanitario Pere Virgili ethics committee (Barcelona, Spain) (reference No.: CEIM 003/2025). For the purposes of this study, we selected the subgroup of patients with STEMI who underwent PCI in which ELCA was used to facilitate thrombus removal.
Thrombus burden was assessed using the thrombus grading classification9 as defined by the Thrombolysis in Myocardial Infarction (TIMI) study group, ranging from 0 to 5. A LTB was defined as a thrombus score ≥ 3. According to our internal protocol, ELCA was considered in STEMI patients in the presence of angiographic evidence of LTB, defined as TIMI thrombus grade ≥ 3, particularly if TIMI grade-0–1 flow or, poor visualization of the distal vessel, or as a bailout strategy after unsuccessful manual thrombectomy. Clinical variables were meticulously refined, and follow-up details were obtained through a thorough review of the patients’ health records. Following coronary angiography and successful guidewire crossing of the culprit lesion, ELCA was left at the operator’s discretion. It was used either as a primary device for thrombus removal or as a bailout strategy when manual thrombus aspiration did not improve TIMI grade flow. The selection of catheter size was mainly based on the target vessel diameter and on the characteristics of the vessel and the lesion; a 0.9 mm ELCA catheter is usually used in tortuous anatomies due to its better navigability and in small-caliber vessels, whereas a 1.4 mm catheter is used in selected cases involving larger proximal vessels with straight segments. Catheter size (0.9 mm or 1.4 mm) was selected based on vessel diameter and lesion characteristics. Laser fluence (45-60 mJ/mm²) and pulse repetition rate (25-40 Hz) were chosen as per manufacturer’s recommendations.
Before laser application, the target vessel was flushed with saline solution to prevent interaction between the laser and blood or contrast medium. In all cases, continuous saline infusion was administered during laser delivery to avoid coronary artery wall heating. Laser energy was delivered using an ‘on-off’ technique, consisting of 10-s laser activation cycles interspersed with 5-s pauses. The laser catheter was advanced at a rate of approximately 1 mm/s over a 0.014-in coronary guidewire through the target lesion, following the manufacturer’s recommendations.7,10 After 2–3 laser catheter passes, a follow-up coronary angiography was performed to evaluate the efficacy of laser application and assess the feasibility of stent implantation. TIMI grade flow was recorded after the ELCA procedure (Post-ELCA TIMI grade flow) and once the PCI would have been completed (final TIMI grade flow). Technical success was defined as the ability to advance the laser catheter through the entire target lesion and deliver laser energy successfully. Procedural success was defined as achieving a final TIMI grade ≥ 2 flow without any major cath lab-related complications, such as death, coronary perforation, or emergency bypass surgery after PCI completion. All procedural complications, including death, coronary perforation,11 emergency bypass surgery, distal embolization, ventricular arrhythmia, and no-reflow were carefully documented and reported. Follow-up was conducted via retrospective review of health records, and major adverse cardiovascular events (MACE) defined as a composite endpoint of all-cause mortality, new myocardial infarction, and target lesion revascularization were recorded at the follow-up.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation for normally distributed data or as the median (interquartile range) for non-normally distributed data. Inter-group comparisons were performed using an unpaired Student’s t-test for normally distributed variables and the Mann–Whitney U test for non-normally distributed variables. Categorical variables are expressed as counts and percentages and were analyzed using the chi-square test or Fisher’s exact test, as appropriate.
The composite endpoint of MACE was analyzed as time-to-event data at the follow-up. Kaplan–Meier survival analysis was performed to estimate the event-free survival rates. All statistical analyses were conducted using SPSS Statistics (version 23.0, IBM Corp., United States). A 2-tailed P value < .05 was considered statistically significant.
RESULTS
Between July 2015 and August 2024, a total of 130 PCI s were performed in patients with STEMI using ELCA as an adjuvant therapy for thrombus removal. The patients’ mean age was 61.8 ± 11.7 years, with 18 (13.8%) being women and 18 (13.8%) diagnosed with diabetes mellitus. ELCA was employed as the primary device for thrombus dissolution in 66 cases (50.8%) and as a bailout strategy in 64 cases (49.2%). Within the bailout group, manual thrombus aspiration was performed in 47 cases (36.2%), balloon dilation in 6 cases (4.6%), and thrombus debulking using the dotter effect in 11 cases (8.5%).
In the overall cohort, 124 patients (95.4%) presented with culprit lesions with a LTB. Before laser energy application, TIMI grade-0 flow was reported in 79 (60.8%) cases TIMI grade-1 flow in 32 (24.6%). After ELCA, TIMI grade-2 and 3 flows were achieved in 45 (34.6%) and 66 (50.8%) cases, respectively; P < .001 (figure 1).

Figure 1. TIMI grade flow distribution before and after ELCA application. Stacked bar graph showing the distribution of TIMI grade 0-3 flows at 3 different time points: initial angiography, post-ELCA, and final angiographic result after PCI. A marked improvement in coronary flow is observed following ELCA, with a progressive increase in TIMI grade-3 flow from 6.2% to 74.6%. ELCA, excimer laser coronary angioplasty; TIMI, Thrombolysis in Myocardial Infarction.
Technical success was achieved in 128 (98.5%) cases, and procedural success in 124 (95.4%) (table 1). Procedural success was significantly higher when ELCA was used as the initial strategy vs when it was used as the bailout strategy (100% vs 90.6%; P = .013). However, procedural time was significantly longer in the bailout vs the initial strategy group (69.81 vs 48.50 min, respectively) (table 2).
Table 1. Baseline characteristics of patients
| Variable (n = 130) | Value |
|---|---|
| Age, yr | 61.8 ± 11.7 |
| Female | 18 (13.8) |
| Hypertension | 59 (45,4%) |
| Hypercholesterolemia | 57 (43,8%) |
| Tobacco use | 78 (60%) |
| Diabetes mellitus | 18 (13.8) |
| Killip classification | |
| I | 98 (75.4) |
| II | 18 (13.8) |
| III | 3 (2.3) |
| IV | 11 (8.5) |
| Radial access | 118 (90,7%) |
| Femoral access | 12 (9,3%) |
| Lesion localization | |
| LMCA | 3 (2,3%) |
| LAD | 55 (42,3%) |
| LCX | 8 (6,2%) |
| RCA | 64 (49,2 %) |
| Primary device | 66 (50.8) |
| Bailout strategy | 64 (49.2) |
| Large thrombus burden | 124 (95.4) |
| Laser catheter size, Fr | |
| 0.9 | 114 (87.7) |
| 1.4 | 16 (12.3%) |
| Procedural time, min | 60 (43–86) |
| Fluoroscopy time, min | 22.2 ±12.2 |
| Laser frequency, Hz | 31 ± 10.4 |
| Laser fluency, mJ/mm2 | 46.5 ± 9.17 |
| Laser delivery time, s | 125.9 ± 83.4 |
| Technical success | 128 (98.5) |
| Procedural success | 124 (95.4) |
|
LAD: left anterior descending coronary artery; LCX: left circumflex artery; LMCA: left main coronary artery; RCA: right coronary artery. Categorical data are presented as absolute value and percentage, n (%); and continuous variables as mean ± standard deviation or first and third quartiles. |
|
Table 2. Difference in variables between the initial and bailout strategy groups
| Variable | ELCA as the initial strategy (n = 66) | ELCA as the bailout strategy (n = 64) | P-value |
|---|---|---|---|
| Complications | 8 (12.1%) | 3 (4.7%) | .100 |
| Large thrombus burden | 64 (97%) | 60 (93.8%) | .440 |
| Technical success | 65 (98.5%) | 63 (98.4%) | 1.000 |
| Procedural success | 66 (100%) | 58 (90.6%) | .013 |
| Procedural time, median | 48.50 (38.83–66.61) | 69.81 (55.36–101) | < .001 |
|
ELCA, excimer laser coronary angioplasty. Categorical data are presented as absolute value and percentage, n (%); and continuous variables as mean ± standard deviation or first and third quartiles. |
|||
One case of type IV coronary perforation, according to the modified Ellis classification, occurred in an octogenarian patient with an ecstatic and tortuous right coronary artery. Perforation sealing was achieved with the implantation of a covered stent. One cath lab-related death occurred in a patient with an uncrossable mid-segment of a left anterior descending coronary artery lesion and initial TIMI grade-3 flow. Following balloon dilation and partial advancement of the laser probe, complete vessel occlusion and suspected left main coronary artery dissection resulted in cardiac arrest and cath lab-related death.
Other procedural complications included distal embolization in 3 (2.3%) cases and slow flow or no-reflow in 4 (3.1%). Among the slow/no-reflow cases, 1 occurred after laser application, and 3 following stent implantation and/or post-dilation. All were successfully managed with optimal medical therapy, achieving final TIMI grade-2 flow. One episode of ventricular arrhythmia occurred during saline washout of the target vessel, requiring electrical cardioversion. Additionally, 1 case of stent thrombosis (0.8%) occurred intraoperatively (figure 2).
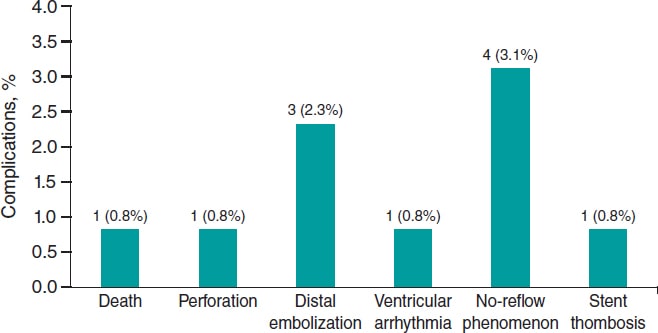
Figure 2. ELCA-related procedural complications. Bar chart showing the frequency and percentage of major complications during or immediately after ELCA. The most common was no-reflow (3.1%), followed by distal embolization (2.3%). Other events (death, perforation, ventricular arrhythmia, and stent thrombosis) were rare (0.8% each). ELCA, excimer laser coronary angioplasty.
Long-term follow-up data were missing for 6 patients (4.6%). At the 2-year follow-up, the event-free rate for combined MACE was 0.80 (95%CI, 0.73–0.88) as determined by the Kaplan–Meier estimator (table 3 and figure 3).
Table 3. List of adverse clinical events
| Patient No. | Event | Date |
|---|---|---|
| 6 | Death | 1 |
| 13 | Death | 493 |
| 15 | Death | 148 |
| 23 | Death | 11 |
| 33 | Death | 170 |
| 36 | Death | 4 |
| 43 | New myocardial infarction associated with TLR | 39 |
| 50 | New myocardial infarction | 213 |
| 61 | Death | 16 |
| 77 | Death | 1 |
| 83 | New myocardial infarction associated with TLR | 119 |
| 84 | Death | 4 |
| 92 | Death | 1 |
| 98 | Death | 0 |
| 101 | Death | 37 |
| 110 | Death | 0 |
| 113 | Death | 12 |
| 118 | Death | 253 |
| 121 | Death | 139 |
| 124 | New myocardial infarction associated with TLR | 291 |
| 128 | Death | 10 |
|
TLR, target lesion revascularization. Lost to follow-up: 6 patients (4.6%). |
||
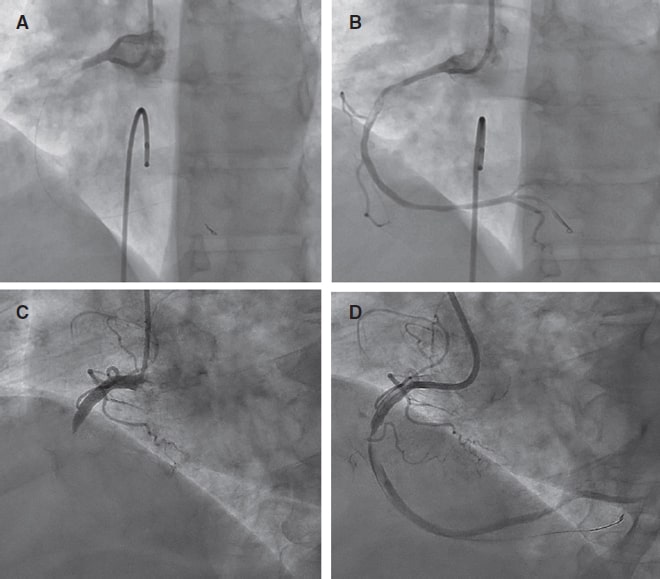
Figure 3. Pre- and post-ELCA findings in 2 typical cases of right coronary artery with large thrombus burden. ELCA, excimer laser coronary angioplasty.
DISCUSSION
The main finding of this single-center study is that coronary laser angioplasty is a feasible, safe, and effective adjuvant therapy in the context of PCI (videos 1-4 of the supplementary data), demonstrating a low rate of complications and an acceptable long-term rate of MACE.
Data on the use of ELCA in acute myocardial infarction remain limited, with most evidence coming from non-randomized clinical trials. The CARMEL trial,12 the largest multicenter study to date, evaluated the safety, feasibility, and acute outcomes of ELCA in patients with acute myocardial infarction within 24 h of symptom onset requiring urgent PCI. TIMI grade flow significantly improved after laser application, increasing from 1.2 to 2.8, with an overall procedural success rate of 91% and a low distal embolization rate of 2%, even though 65% of cases had a LTB. In our study, 95.4% of the patients had culprit lesions with a LTB, and laser delivery significantly improved the mean TIMI grade flow from 0.6 to 2.29, with a comparable distal embolization rate of 2.3%.
Arai et al.13 retrospectively analyzed 113 consecutive acute coronary syndrome cases undergoing PCI comparing an ELCA group (n = 48) with a thrombus aspiration group (n = 50). They found that ELCA was associated with a significantly shorter door-to-reperfusion time, a better myocardial blush grade, and fewer MACE vs thrombus aspiration. These favorable outcomes are likely attributable to ELCA’s ability to vaporize thrombi through acoustic shockwave propagation and dissolution mechanisms,12 as well as its capacity to suppress platelet aggregation kinetics (a phenomenon known as the ‘stunned platelet’ effect).14
Reperfusion injury to the coronary microcirculation is a critical concern during PCI in STEMI patients. While manual thrombus aspiration can reduce the rate of no-reflow in patients with a LTB, residual thrombi and decreased coronary flow following thrombectomy have been associated with a higher risk of no-reflow.15 In a study of 812 patients with STEMI and a LTB undergoing PCI, Jeon et al.16 reported that 34.4% experienced failed thrombus aspiration, defined as no thrombus retrieval, remnant thrombus grade ≥ 2, or distal embolization. This failure was associated with an increased risk of impaired myocardial perfusion and microvascular obstruction.
ELCA’s ability to vaporize thrombi (with a low rate of distal embolization) and mitigate platelet activation, key cofactors in myocardial reperfusion damage,17 can potentially reduce this undesirable effect. Although the direct impact of ELCA on coronary microcirculation in PCI has not been well documented, evidence from smaller studies suggests potential benefits. For example, Ambrosini et al.18 investigated ELCA in 66 patients with acute myocardial infarction and complete thrombotic occlusion of the infarcted related artery, demonstrating excellent acute coronary and myocardial reperfusion outcomes (as assessed by the myocardial blush score and the corrected TIMI frame count), as well as a low rate of long-term left ventricular remodeling (8%). The significant improvement in mean TIMI grade flow observed immediately after ELCA application in our cohort may indirectly suggest a protective effect of this technique on coronary microcirculation. However, the lack of large studies comparing ELCA with conventional STEMI treatment limits the ability to definitively confirm the benefits of coronary laser therapy in this setting. Shibata et al.19 explored the impact of ELCA on myocardial salvage using nuclear scintigraphy in 72 STEMI patients and an onset-to-balloon time < 6 h, comparing ELCA (n = 32) and non-ELCA (n = 40) groups. Their findings indicated a trend towards a higher myocardial salvage index in the ELCA vs the non-ELCA group (57.6% vs 45.6%).
Limitations
This study has several limitations. It is a retrospective analysis, which inherently introduces biases related to data collection, interpretation and application of inclusion and exclusion criteria. Besides, the absence of a comparative group limits the ability to establish the definitive clinical benefit of ELCA and its potential superiority over other strategies in the context of STEMI patients undergoing PCI. Furthermore, while the significant improvement of TIMI grade flow observed after laser application suggests potential benefits for coronary microcirculation, we did not directly assess this effect or thrombus burden reduction since post-ELCA thrombus grading was not systematically recorded. Unfortunately, in our retrospective database, PCI details (segmental analysis of coronary arteries and classification), the use of intravascular imaging modalities, dual antiplatelet therapy regimens (aspirin in addition to a potent P2Y12 inhibitor, or clopidogrel when prasugrel or ticagrelor were contraindicated, was routinely prescribed following current guidelines recommendations) or post-PCI echocardiography or cardiac magnetic resonance parameters were not systematically collected (unavailable in the health reports we revised) and follow-up data were missing for 4.6% of patients, all of which limited our ability to assess their potential impact on clinical outcomes. Last, our findings represent the experience of a single center, the percentage of women and patients with diabetes is relatively low, and procedures were performed by 5 trained operators, which may limit the external validity of the results.
CONCLUSIONS
ELCA seems to be an effective device for thrombus dissolution in the STEMI scenario, with excellent technical and procedural success rates. Besides, a low complication rate and favorable long-term outcomes with an acceptable event-free survival rate was observed in the present cohort.
DATA AVAILABILITY
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
FUNDING
None declared.
ETHICAL CONSIDERATIONS
This study was approved by the center Ethics Committee (waiving the need for informed consent due to the retrospective nature of the investigation) in full compliance with national legislation and the principles set forth in the Declaration of Helsinki. Sex was reported as per biological attributes (SAGER guidelines).
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCE
The authors state that no generative artificial intelligence technologies were used in the preparation or revision of this article.
AUTHORS’ CONTRIBUTIONS
A. Pernigotti and M. Mohandes were responsible for the conceptualization and study design and contributed equally as co-first authors. M. Mohandes, A. Pernigotti, R. Bejarano, H. Coimbra, F. Fernández, C. Moreno, M. Torres, J. Guarinos were involved in data collection and statistical analysis. M. Mohandes, A. Pernigotti, and J.L. Ferreiro were involved in manuscript drafting and critical revision and were responsible for the supervision and final approval. All authors have accepted responsibility for the entire content of this manuscript and consented to its submission to the journal. Each author reviewed all results and approved the final version of the manuscript.
CONFLICTS OF INTEREST
The authors declared no conflicts of interest related to this manuscript. J.L. Ferreiro declared having received speaker’s fees from Eli Lilly Co, Daiichi Sankyo, Inc., AstraZeneca, Pfizer, Abbott, Boehringer Ingelheim, Bristol-Myers Squibb, Rovi, Terumo and Ferrer; consulting fees from AstraZeneca, Eli Lilly Co., Ferrer, Boston Scientific, Pfizer, Boehringer Ingelheim, Daiichi Sankyo, Inc., Bristol-Myers Squibb and Biotronik; and research grants from AstraZeneca, not related to this manuscript.
WHAT IS KNOWN ABOUT THE TOPIC?
- ELCA is a specialized technique used as adjuvant therapy during PCI for STEMI, particularly in patients with LTB.
- Although former studies have shown that ELCA can improve coronary flow and potentially reduce thrombotic material, data in the setting of acute myocardial infarction remain limited.
- ELCA is mostly used in high-volume centers by experienced operators, and standardized criteria for use in STEMI patients are not consistently reported in the literature.
WHAT DOES THIS STUDY ADD?
- This is one of the largest retrospective single-center series (130 patients) ever reported on the use of ELCA in STEMI patients with angiographically defined LTB.
- The study shows a high rate of technical and procedural success, significant improvement in TIMI flow, low rate of complication, and acceptable long-term outcomes.
- It provides detailed information on operator training, device selection, and laser settings, contributing to transparency and reproducibility.
- It also identifies current limitations in data reporting (eg, lack of systematic thrombus grading or dual antiplatelet therapy regimen documentation), underscoring the need for standardization in future studies.
SUPPLEMENTARY DATA
Vídeo 1. Mohandes M. DOI: 10.24875/RECICE.M25000537
Vídeo 2. Mohandes M. DOI: 10.24875/RECICE.M25000537
Vídeo 3. Mohandes M. DOI: 10.24875/RECICE.M25000537
Vídeo 4. Mohandes M. DOI: 10.24875/RECICE.M25000537
REFERENCES
1. Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC guidelines for the management of acute coronary syndromes. Eur Heart J. 2023;44:3720-3826.
2. Kim MC, Cho JY, Jeong HC, et al. Long-term clinical outcomes of transient and persistent no reflow phenomena following percutaneous coronary intervention in patients with acute myocardial infarction. Korean Circ J. 2016;46:490-498.
3. Sardella G, Mancone M, Bucciarelli-Ducci C, et al. Thrombus aspiration during primary percutaneous coronary intervention improves myocardial reperfusion and reduces infarct size:the EXPIRA prospective, randomized trial. J Am Coll Cardiol. 2009;53:309-315.
4. Jolly SS, Cairns JA, Yusuf S, et al. Randomized trial of primary PCI with or without routine manual thrombectomy. N Engl J Med. 2015;372:1389-1398.
5. Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization:Executive summary. Circulation. 2022;145:e4-e17.
6. Grundfest WS, Litvack F, Forrester JS, et al. Laser ablation of human atherosclerotic plaque without adjacent tissue injury. J Am Coll Cardiol. 1985;5:929-933.
7. Mohandes M, Fernández L, Rojas S, et al. Safety and efficacy of coronary laser ablation as an adjuvant therapy in percutaneous coronary intervention:a single-centre experience. Coron Artery Dis. 2021;32:241-246.
8. Rawlins J, Din JN, Talwar S, O'Kane P. Coronary intervention with the excimer laser:review of the technology and outcome data. Interv Cardiol Rev. 2016;11:27-32.
9. Gibson CM, de Lemos JA, Murphy SA, et al. Combination therapy with abciximab reduces angiographically evident thrombus in acute myocardial infarction:a TIMI 14 substudy. Circulation. 2001;103:2550-2554.
10. Topaz O, Das T, Dahm J, et al. Excimer laser revascularisation:current indications, applications and techniques. Lasers Med Sci. 2001;16:72-77.
11. Ellis SG, Ajluni S, Arnold AZ, et al. Increased coronary perforation in the new device era. Incidence, classification, management, and outcome. Circulation. 1994;90:2725-2730.
12. Topaz O, Ebersole D, Das T, et al. Excimer laser angioplasty in acute myocardial infarction (the CARMEL multicenter trial). Am J Cardiol. 2004;93:694-701.
13. Arai T, Tsuchiyama T, Inagaki D, et al. Benefits of excimer laser coronary angioplasty over thrombus aspiration therapy for patients with acute coronary syndrome and thrombolysis in myocardial infarction flow grade 0. Lasers Med Sci. 2022;38:13.
14. Topaz O, Minisi AJ, Bernardo NL, et al. Alterations of platelet aggregation kinetics with ultraviolet laser emission:the “stunned platelet“phenomenon. Thromb Haemost. 2001;86:1087-1093.
15. Ahn SG, Choi HH, Lee JH, et al. The impact of initial and residual thrombus burden on the no-reflow phenomenon in patients with ST-segment elevation myocardial infarction. Coron Artery Dis. 2015;26:245-253.
16. Jeon HS, Kim YI, Lee JH, et al. Failed thrombus aspiration and reduced myocardial perfusion in patients with STEMI and large thrombus burden. JACC Cardiovasc Interv. 2024;17:2216-2225.
17. Rezkalla SH, Kloner RA. No-reflow phenomenon. Circulation. 2002;105:656-662.
18. Ambrosini V, Cioppa A, Salemme L, et al. Excimer laser in acute myocardial infarction:single centre experience on 66 patients. Int J Cardiol. 2008;127:98-102.
19. Shibata N, Takagi K, Morishima I, et al. The impact of the excimer laser on myocardial salvage in ST-elevation acute myocardial infarction via nuclear scintigraphy. Int J Cardiovasc Imaging. 2020;36:161-170.
ABSTRACT
Introduction and objectives: To compare the effects of drug-coated balloon (DCB) vs drug-eluting stent (DES) in patients presenting with de novo large vessel coronary artery disease (CAD).
Methods: We conducted a systematic research of randomized controlled trials comparing DCB vs DES in patients with de novo large vessel CAD. Data were pooled by meta-analysis using a random-effects model. The prespecified primary endpoint was target lesion revascularization (TLR).
Results: A total of 7 trials enrolling 2961 patients were included. The use of DCB vs DES was associated with a similar risk of TLR (OR, 1.21; 95%CI, 0.44-3.30; I2 = 48%), all-cause mortality (OR, 1.56; 95%CI, 0.94- 2.57; I2 = 0%), cardiac death (OR, 1.65; 95%CI, 0.90-3.05; I2=0%), myocardial infarction (OR, 0.97; 95%CI, 0.58-1.61; I2 = 0%), major adverse cardiovascular adverse (OR, 1.19; 95%CI, 0.74-1.90; I2 = 13.5%) and late lumen loss (standardized mean difference [SMD], −0.35; 95%CI, −0.74 to 0.04; I2 = 81.4%). However, the DCB was associated with a higher risk of target vessel revascularization (OR, 2.47; 95%CI, 1.52-4.03; I2 = 0%) and smaller minimal lumen diameter during late follow-up (SMD, −0.36; 95%CI, −0.56 to −0.15; I2 = 34.5%). Nevertheless, prediction intervals included the value of no difference for both outcomes.
Conclusions: In patients with de novo large vessel CAD the use of DCB vs DES is associated with a similar risk of TLR. However, the DES achieves better late angiographic results.
Keywords: Drug-coated balloon. Drug-eluting stent. Coronary artery disease.
RESUMEN
Introducción y objetivos: Comparar los efectos del balón farmacoactivo (BFA) frente al stent farmacoactivo (SFA) en pacientes con enfermedad arterial coronaria (EAC) de gran vaso de novo.
Métodos: Se realizó una búsqueda sistemática de ensayos clínicos aleatorizados comparando BFA frente a SFA en pacientes con EAC de gran vaso de novo. Los datos se agruparon mediante un metanálisis de efectos aleatorios. El objetivo primario fue la necesidad de revascularización de la lesión diana (RLD).
Resultados: Se incluyeron 7 ensayos con 2.961 pacientes. El uso de BFA, en comparación con SFA, se asoció con un riesgo similar de RLD (OR = 1,21; IC95%, 0,44-3,30; I2 = 48%), muerte por todas las causas (OR = 1,56; IC95%, 0,94-2,57; I2 = 0%), muerte de causa cardiovascular (OR = 1,65; IC95%, 0,90-3,05; I2 = 0%), infarto de miocardio (OR = 0,97; IC95%, 0,58-1,61; I2 = 0%), acontecimientos adversos cardiacos mayores (OR = 1,19; IC95%, 0,74-1,90; I2 = 13,5%) y pérdida luminal tardía (DME = −0,35; IC95%, −0,74 a 0.04; I2 = 81,4%). Sin embargo, el BFA se asoció a un mayor riesgo de revascularización del vaso diana (OR = 2,47; IC95%, 1,52-4,03; I2 = 0%) y a un menor diámetro luminal mínimo en el seguimiento (DME: −0,36; IC95%, −0,56 a −0,15; I2 = 34,5%), aunque los intervalos de predicción incluyeron el valor nulo para ambos resultados.
Conclusiones: En los pacientes con EAC de gran vaso de novo, el BFA comparado con el SFA se asoció a un riesgo similar de RLD, obteniendo el SFA mejores resultados angiográficos.
Palabras clave: Balón farmacoactivo. Stent farmacoactivo. Enfermedad arterial coronaria.
Abbreviations
CAD: coronary artery disease. DCB: drug-coated balloon. DES: drug-eluting stent. MI: myocardial infarction. MLD: minimum lumen diameter. TLR: target lesion revascularization.
INTRODUCTION
Drug-eluting stents (DES) remain the standard of treatment for patients undergoing percutaneous coronary intervention (PCI).1,2 However, DES are associated with a gradually and permanent increased risk of adverse events, particularly due to late stent thrombosis and in-stent restenosis, with a 2% incidence rate per year with no plateau observed.1 This risk is even higher when complex and long lesions are treated.3 In recent years, drug-coated balloons (DCB) have emerged as a potential alternative treatment option to DES. Following adequate lesion preparation, unlike traditional stents, DCBs can release an antiproliferative drug into the vessel wall without leaving behind a permanent metal scaffold. Notably, permanent scaffolding can distort and constrain the coronary vessel, thus impairing vasomotion and adaptive remodelling, while also promoting chronic inflammation.4 DCB-PCI is a well-established treatment for in-stent restenosis and small-vessel coronary artery disease (CAD).5,6 However, its role in de novo large vessel CAD remains controversial. In a recent randomized clinical trial (RCT) with patients undergoing de novo CAD revascularization, a strategy of DCB-PCI did not achieve non-inferiority vs DES in terms of device-oriented composite endpoint driven by higher rates of target lesion revascularization (TLR).7 Contrary to prior published research, our findings did not support similar clinical outcomes for DCB vs DES in patients with de novo large vessel CAD.8,9 A recent meta-analysis of 15 studies compared DCB-PCI or hybrid angioplasty vs DES-PCI in patients with vessels > 2.75 mm in diameter showing no significant differences in the clinical endpoints of TLR, cardiac death, and MI.10 However, 14 of the 15 included studies were non-RCT, and the recent previously reported RCT was not included. Nevertheless, individual non-inferiority studies often lack the statistical power needed to definitively compare these technologies, underscoring the need for a systematic appraisal of treatment effects and evidence quality. Therefore, we conducted a systematic review and meta-analysis of available RCT to provide a comprehensive and quantitative assessment of evidence on the efficacy of DCB vs the current-generation DES in de novo large vessel CAD in terms of adverse events at longest available follow-up.
METHODS
Search strategy and selection criteria
We conducted a meta-analysis of RCT according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2009 guidelines.11 Two reviewers independently identified the relevant studies through an electronic search across the MEDLINE and Embase databases (from inception to October 2024). In addition, we employed backward snowballing (eg, reference review from identified articles and pertinent reviews). No language, publication date or publication status restrictions were imposed. This study is registered with PROSPERO and the search strategy is available in the supplementary data.
Study selection
Two reviewers independently assessed trial eligibility based on titles, abstracts, and full-text reports. Discrepancies in study selection were discussed and resolved with a third investigator. Eligible studies needed to meet the following pre-specified criteria: a) RCT comparing PCI with DCB and PCI with DES; b) study population including patients with de novo large vessel CAD (eg, defined as vessel diameter ≥ 2.5 mm);12 c) availability of clinical outcome data (without restriction as to follow-up time). Exclusion criteria were a) lack of a randomized design; b) studies including patients undergoing treatment for in-stent restenosis; c) studies including patients with de novo small vessel CAD; d) lack of any clinical outcome data.
A reference vessel diameter ≥ 2.5 mm was established as the cut-off value to define large vessel based on a recent proposed standardized definition.12
Data extraction
Three investigators (J. Llau García, S. Huélamo Montoro and J. A. Sorolla Romero) independently assessed studies for possible inclusion, with the senior investigator (J. Sanz-Sánchez) resolving discrepancies. Non-relevant articles were excluded based on title and abstract. The same investigators independently extracted data on study design, measurements, patient characteristics, and outcomes using a standardized data-extraction form. Data extraction conflicts were discussed and resolved with the senior investigator.
Data on authors, year of publication, inclusion and exclusion criteria, sample size, patients’ baseline patients, endpoint definitions, effect estimates, and follow-up time were collected.
Endpoints
The prespecified primary endpoint was TLR. Secondary clinical endpoints were all-cause mortality, cardiac death, myocardial infarction (MI), target vessel revascularization (TVR) and major adverse cardiovascular events (MACE). Secondary angiographic endpoints were minimum lumen diameter (MLD) and late lumen loss (LLL). Each endpoint was assessed according to the definitions reported in the original study protocols, as summarized in table 1 of the supplementary data. All the endpoints were assessed at the maximum follow-up available.
Table 1. Main features of included studies
| Study | Year of publication | No. of patients | Type of Device | Reference vessel diameter (mean ± SD) (mm) | Multicenter | Clinical follow up (months) | Angiographic follow-up (months) | |
|---|---|---|---|---|---|---|---|---|
| DCB | DES | |||||||
| REC-CAGEFREE I7 | 2024 | 1133 | 1139 | Paclitaxel-DCB Sirolimus-DES |
3.00 ± 0.55 | YES | 24 | NO |
| Nishiyama et al.13 | 2016 | 30 | 30 | Paclitaxel-DCB Everolimus-DES |
2.80 ± 0.63 | NO | 8 | 8 |
| Xue Yu et al.8 | 2022 | 85 | 85 | Paclitaxel-DCB Everolimus-DES |
2.89 ± 0.33 | NO | 12 | 9 |
| REVELATION9 | 2019 | 60 | 60 | Paclitaxel-DCB Sirolimus and everolimus DES |
3.24 ± 0.50 | NO | 24 | 9 |
| Gobic et al.15 | 2017 | 38 | 37 | Paclitaxel-DCB Sirolimus-DES |
> 2.50 | NO | 6 | 6 |
| Hao et al.16 | 2021 | 38 | 42 | Paclitaxel-DCB NA |
> 2.50 | NO | 12 | 12 |
| Wang et al.14 | 2022 | 92 | 92 | Paclitaxel-DCB Sirolimus-DES |
3.37 ± 0.52 | NO | 12 | 9 |
|
DCB, drug-coated balloon; DES, drug-eluting stent; NA, not available. |
||||||||
Risk of bias
The risk of bias in each study was assessed using the revised Cochrane risk of bias tool (RoB 2.0).11 Three investigators (J. Llau García, S. Huélamo Montoro and J. A. Sorolla Romero) independently assessed 5 domains of bias in RCT: a) randomization process, b) deviations from intended interventions, c) missing outcome data, d) outcome measurement, and e) selection of reported results (table 2 of the supplementary data).
Table 2. Baseline clinical characteristics of included patients
| Study | Age (years) | Male (%) | Diabetes (%) | Smoking (%) | Hypertension (%) | LVEF (%) | Clinical Presentation (CCS/ACS) (%) | Multivessel (%) | Complex lesion (%) |
|---|---|---|---|---|---|---|---|---|---|
| REC-CAGEFREE I7 | 62 | 69.3 | 27.3 | 45 | 60.1 | 60 | 44.9/55.3 | 4.8 | 0 |
| Nishiyama et al.13 | 69 | 73.3 | 41.6 | 60 | 83.3 | NA | 0/100 | NA | 36 |
| Xue Yu et al.8 | 63.3 | 69.3 | 24.1 | 54 | 63.9 | > 40 | 11.1/88.9 | 84 | 44.1 |
| REVELATION9 | 57 | 87 | 10 | 60 | 31 | 57.6 | 0/100 | 71.6 | N/A |
| Gobic et al.15 | 57.4 | 87 | 10 | 49.5 | 33.4 | 50.2 | 0/100 | NA | N/A |
| Hao et al.16 | 57.5 | 78.5 | 31.5 | 29.5 | 24 | 46 | 0/100 | NA | N/A |
| Wang et al.14 | 49.5 | 93.5 | 81.6 | 81.5 | 71.8 | NA | 0/100 | NA | N/A |
|
ACS, acute coronary syndrome; CCS, chronic coronary syndrome; NA, not available. |
|||||||||
Statistical analysis
Odds ratios (OR) and 95% confidence intervals (95%CI) were calculated using the DerSimonian and Laird random-effects model, with the estimate of heterogeneity being obtained from the Mantel-Haenszel method. The presence of heterogeneity among studies was evaluated with the Cochran Q chi-square test, with P ≤ .10 being considered of statistical significance, and using the I2 test to evaluate inconsistency. A value of 0% indicates no observed heterogeneity, and values of ≤ 25%, ≤ 50%, > 50% indicate low, moderate, and high heterogeneity, respectively. Prediction intervals (95%) in addition to conventional 95%CI around ORs were calculated to assess residual uncertainty. Publication bias and the small study effect were assessed for all outcomes, using funnel plots. The presence of publication bias was investigated using Harbord and Egger tests and visual estimation with funnel plots. We performed a sensitivity analysis by removing one study at a time to confirm that the findings, when compared with DES, were not driven by any single study. To account for different lengths of follow-up across studies, another sensitivity analysis was performed using the Poisson regression model with random intervention effects to calculate inverse-variance weighted averages of study-specific log stratified incidence rate ratios (IRRs). Results were displayed as IRRs, which are exponential ratios of the regression model. Additionally, random-effect meta-regression analyses were performed to assess the impact of the following variables on treatment effect with respect to the primary endpoint: eg, percentage of patients with acute coronary syndrome (ACS), percentage of patients with diabetes mellitus, mean reference vessel diameter and follow-up duration. The statistical level of significance was 2-tailed P < .05. Stata version 18.0 (StataCorp LP, College Station, United States), was used for statistical analyses.
RESULTS
Search results
Figure 1 illustrates the PRISMA study search and selection process. A total of 7 RCT were identified and included in this analysis. The main features of included studies are shown in table 1.
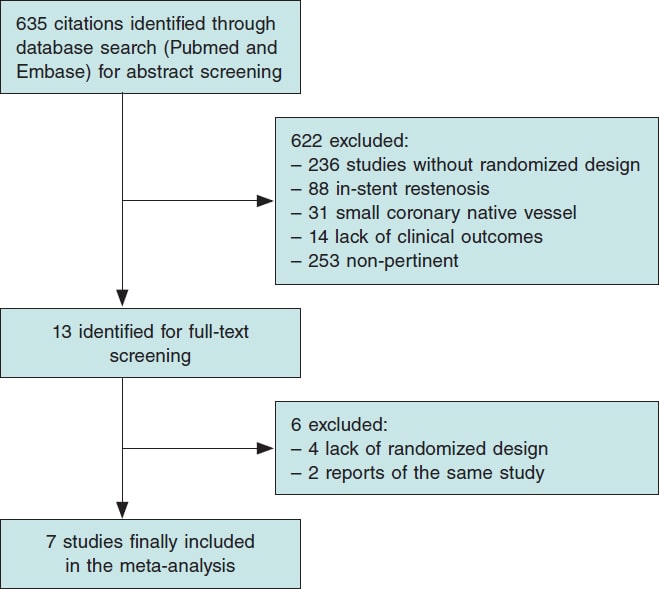
Figure 1. Flow diagram of the search for studies included in the meta-analysis according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Statement.
All studies had a non-inferiority design. A clinical primary endpoint was selected in 1 study,7 and an invasive functional endpoint was selected in another trial,9 while angiographic primary endpoints were prespecified in the remaining studies.8,13-16 The mean clinical and angiographic follow-up were 21.5 months and 8.9 months respectively. A total of 4 studies were conducted in the context of ACS9,14-17 and 1 study in the context of chronic coronary syndrome (CCS).13 Finally, 2 studies enrolled both ACS and CCS patients.7,8 A total of 3 trials enrolled patients treated with second-generation DES (Firebird 2.0 [Microport, China], Xience Xpedition [Abbott Vascular, United States], Orsiro [Biotronik, Germany]),7,9,13 and 2 studies enrolled patients treated with third-generation DES (Biomine [Meril Life Sciences, India], Cordimax [Rientech, China]).14,15 One trial enrolled patients treated with second and third-generation DES (Xience Xpedition [Abbott Vascular, United States], Resolute Integrity, [Medtronic, United States], Firehawk, [MicroPort, China]).8 All studies included patients who underwent paclitaxel-DCB-PCI ([Pantera Lux, Biotronik, Germany],9,14 [SeQuent Please, B Braun, Germany],7,8,13,15 [Bingo DCB, Yinyi Biotech,China]),16 and none with sirolimus-DCB-PCI.
Baseline characteristics
A total of 2961 patients were included, 1476 of whom received DCB and 1485, DES for de novo large vessel CAD. The patients main baseline characteristics are shown in table 2.
Publication bias and asymmetry
Funnel-plot distributions of the pre-specified outcomes indicate absence of publication bias for all the outcomes (figures 1-8 of the supplementary data).
Risk of bias assessment
Table 2 of the supplementary data illustrates the results of the risk of bias assessment with the RoB 2.0 tool. One trial was considered at low overall risk of bias,7 5 raised some concerns8,9,13,14,16 and 1 presented a high overall risk of bias.15
Outcomes
Clinical outcomes
DCB use compared with DES was associated with a similar risk of TLR (OR, 1.21; 95%CI, 0.44-3.30; I2 = 48%), all-cause mortality (OR, 1.56; 95%CI, 0.94- 2.57; I2 = 0%), cardiac death (OR, 1.65; 95%CI, 0.90-3.05; I2 = 0%), MI (OR, 0.97; 95%CI, 0.58-1.61; I2 = 0%) and MACE (OR, 1.19; 95%CI, 0.74-1.90; I2 = 13.5%). However, DCB was associated with a higher risk of TVR (OR, 2.47; 95%CI, 1.52- 4.03; I2 = 0%) (figure 2, figure 3 and figures 9-10 of the supplementary data).
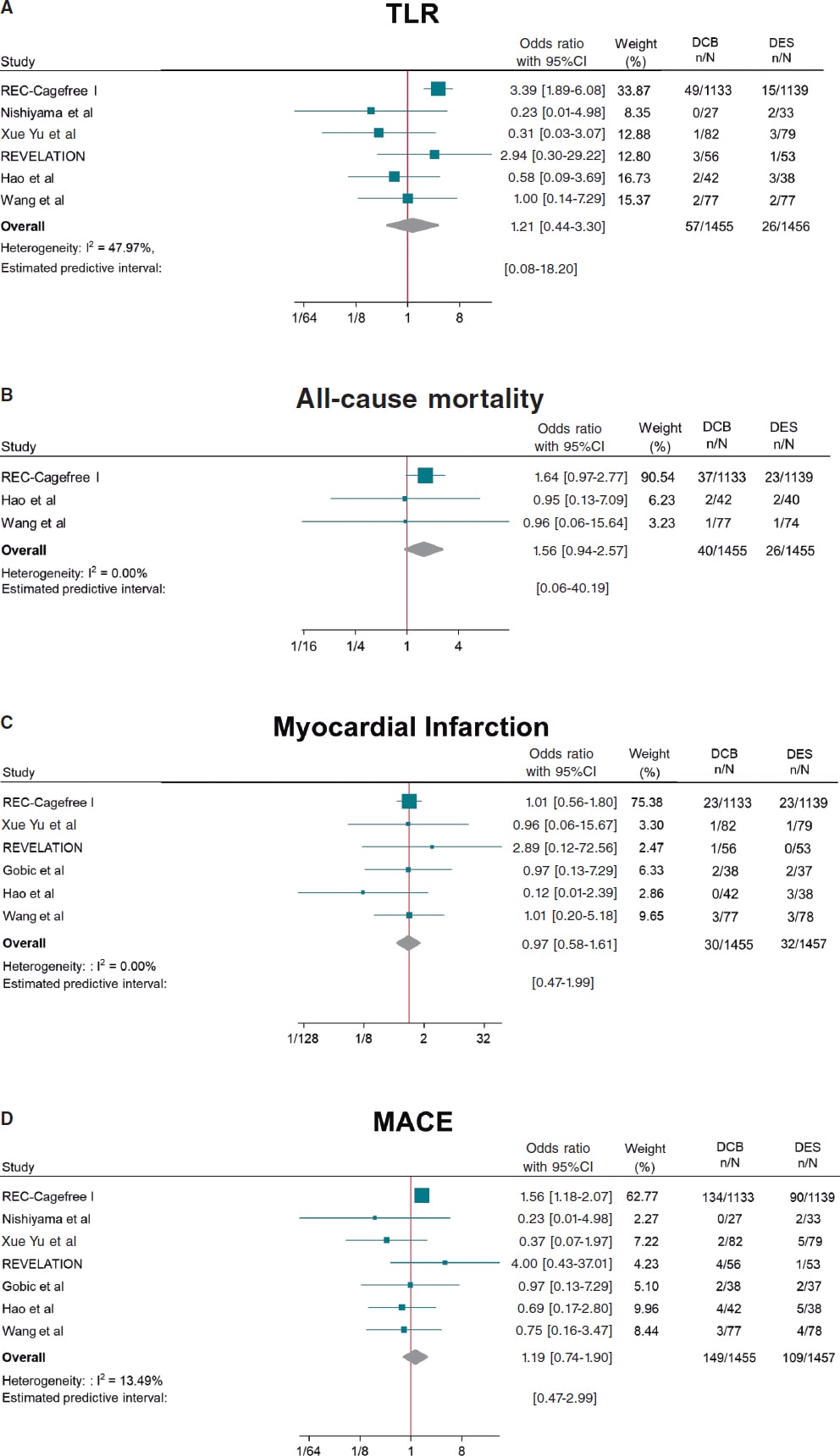
Figure 2. Forest plot reporting trial-specific and summary ORs with 95%CIs for the endpoint of A) target lesion revascularization; B) all-cause mortality; C) myocardial infarction; D) MACE. 95%CI, 95% confidence interval; DCB, drug-coated balloon; DES, drug-eluting stents; MACE, major adverse cardiovascular events; OR, odds ratio. References: REC-Cagefree I.,7 Nishiyama et al.,13 Xue Yu et al.,8 REVELATION,9 Hao et al.,16 Wang et al.,14 and Gobic et al.15
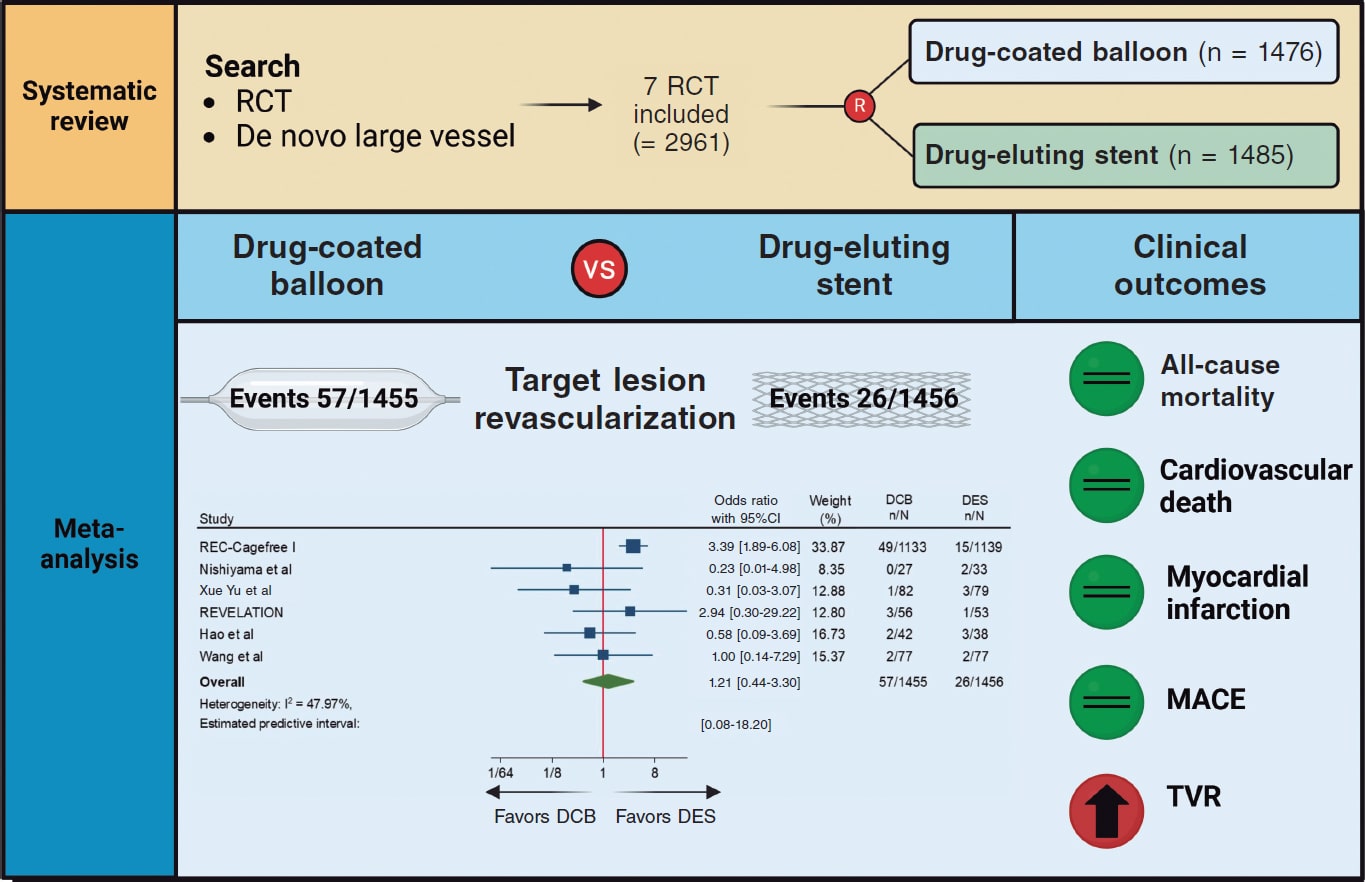
Figure 3. Central Illustration. DCB, drug-coated balloon; DES, drug-eluting stent; RCT, randomized clinical trial; TVR, target vessel revascularization. References: REC-Cagefree I.,7 Nishiyama et al.,13 Xue Yu et al.,8 REVELATION,9 Hao et al.,16 and Wang et al.14
Angiographic outcomes
Compared with DES, DCB use yielded significant smaller MLD (SMD, −0.36; 95%CI, −0.56 to −0.15; I2 = 34.5%) and similar risk of LLL (SMD, −0.35; 95%CI, −0.74 to 0.04; I2 = 81.4%) at follow-up (figure 4).
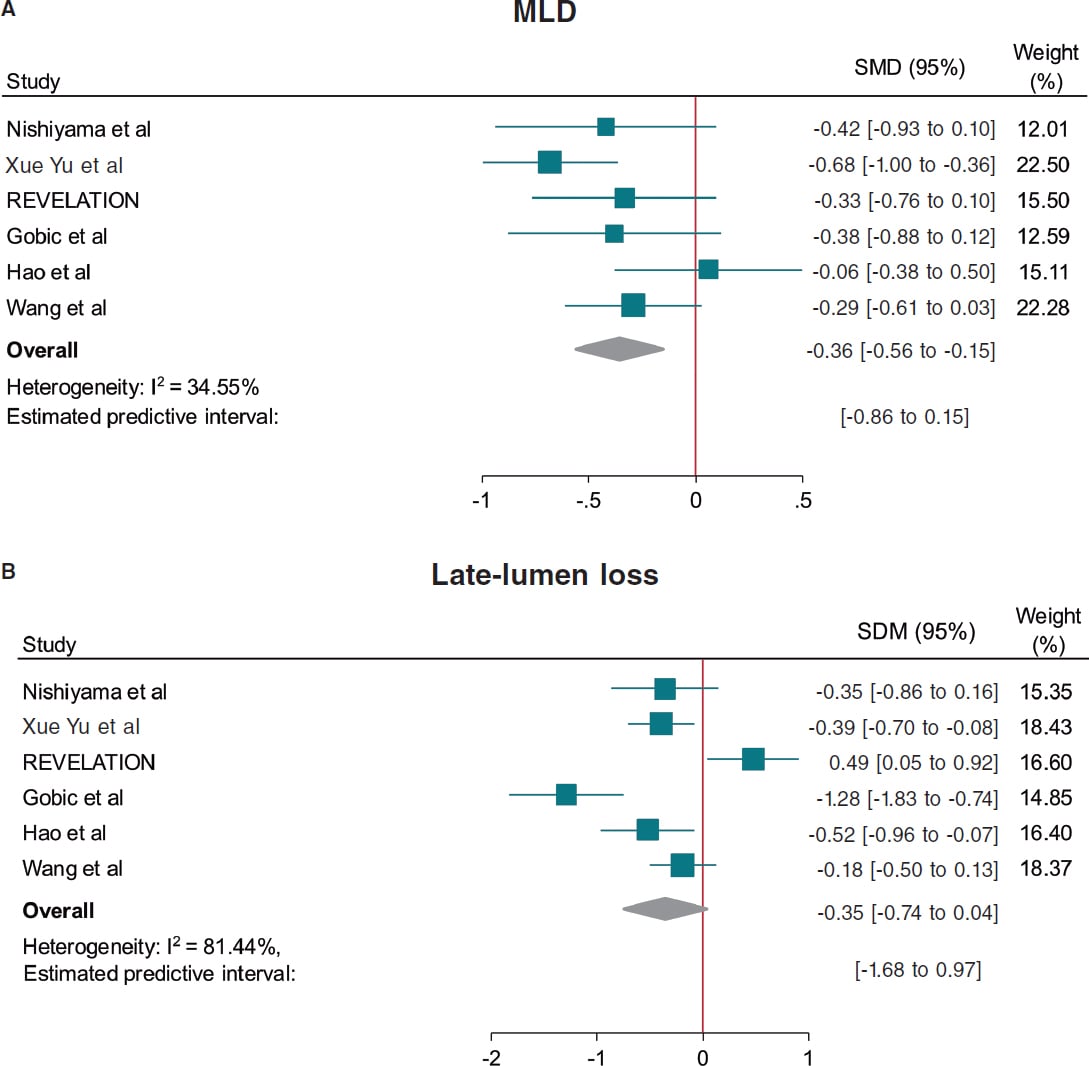
Figure 4. Forest plot reporting trial-specific and summary ORs with 95%CIs for the endpoint of A: minimum lumen diameter, and B: late-lumen loss. 95%CI, 95% confidence interval; DCB, drug-coated balloon; DES, drug-eluting stents; MACE, major adverse cardiovascular events; MLD, minimum lumen diameter; SMD, standardized mean difference; OR, odds ratio. References: Nishiyama et al.,13 Xue Yu et al.,8 REVELATION,9 Gobic et al.,15 Hao et al.,16 and Wang et al.14.
Prediction intervals were consistent with CI for all the outcomes except for TVR and MLD, which included the value of no difference.
Sensitivity analysis
A leave-one-out pooled analysis by iteratively removing one study at a time was performed for all endpoints. Treatment effects were consistent with the main analysis for TLR, all-cause mortality, cardiac death, MI and MLD. The risk of TVR was no longer significantly higher among patients undergoing DCB when removing the CAGEFREE I trial,7 and the risk of LLL was significantly lower among patients undergoing DCB-PCI when removing the REVELATION trial.9 However, an increased risk of MACE was observed among patients undergoing DCB-PCI when removing the study by Xue Yu et al.18 (tables 3-10 of the supplementary data). A sensitivity analysis using estimated IRRs was performed to account for varying follow-up lengths, confirming that our main analysis findings remained unchanged (table 11 of the supplementary data).
Random effect meta-regression analysis found no significant impact of the proportion of patients presenting with ACS (P = .882), diabetes mellitus (P = .641), mean reference vessel diameter (P = .985) and follow-up duration (P = .951) on treatment effect with respect to the primary endpoint.
DISCUSSION
This meta-analysis provides a comprehensive and updated quantitative analysis of available evidence on the comparison of DCB vs DES in de novo large vessel CAD, including data from 2961 patients enrolled in 7 RCT. The main findings of the study are:
a) The use of DCB was associated with a similar risk of clinical events vs DES except for TVR. However, data for this outcome was only available in 3 of the 7 included studies and the increased risk in patients undergoing DCB-PCI was not significant when the CAGEFREE I trial was removed. In addition, prediction intervals were not consistent with the CI. Therefore, the results of this outcome should be interpreted with caution.
b) The effect of DCB on the risk of TLR was not affected by the proportion of patients presenting with ACS or diabetes, as well as the mean reference vessel diameter or follow-up duration as assessed by meta-regression analysis.
c) DCB was associated with lower MLD at angiographic follow-up, but with similar LLL vs DES.
DES are the standard of treatment for patients undergoing PCI. However, complications such as stent thrombosis and in-stent restenosis still occur with rates estimated at 0.7-1% and 5-10% at the 10-year follow-up respectively.19,20 Therefore, in recent years there has been a growing concern for developing strategies to reduce stent-related adverse events. In this context, DCBs have emerged as a potential treatment alternative based on a “leaving nothing behind” strategy. Nevertheless, data of patients presenting with de novo large CAD is scarce and conflicting. The CAGEFREE I is the only available clinically powered RCT that included 2272 patients undergoing de novo non-complex CAD revascularization across 40 centers in China. A strategy of DCB-PCI did not achieve non-inferiority vs DES in terms of device-oriented composite endpoint driven by higher rates of TLR in the DCB-PCI group (3.1% vs 1.2%, P = .002). On the other hand, in single-center RCT conducted by Nishiyama et al. with 60 patients with CCS undergoing elective PCI a trend toward lower rates of TLR in the DCB-PCI group (0% vs 6.1%, P = .193) was shown at the 8-mont follow-up.13 Similarly, in a RCT including 170 patients undergoing PCI for de novo large CAD lower rates of TLR at the 12-month follow-up were found in patients undergoing DCB-PCI (1.6% vs 3.4%, P = .306).14 In our analysis when pooling data from all available RCT, the risk of TLR was similar among patients undergoing DCB-PCI or DES-PCI. Notably, since this result was obtained with a moderate heterogeneity (I2 ≈ 50%), it should be interpreted with caution regarding its general applicability. These findings remained unvaried at the leave-one-out analysis. In addition, prediction intervals were consistent with CI around ORs showing lack of residual uncertainty. Previous studies have shown that in-stent restenosis after DES is not a benign phenomenon, presenting as an ACS in about 70% of the cases, with 5-10% of these resulting in MI.21 We could speculate that the lack of permanent scaffold with DCB vs DES may predispose to a less aggressive pattern of restenosis and not increase the risk of thrombotic vessel closure beyond 3 months when vessel healing after DCB-PCI has occurred.22
Notably, 5 of the 7 studies included in this meta-analysis enrolled patients presenting with ACS. A total of 34% of the patients included in the CAGEFREE study presented with ACS, with 16% being STEMI cases.7 Four other studies only included STEMI patients.7,9,14-16 Although the performance of DCB in the STEMI scenario is unknown, its use in clinical practice is increasing.23 Culprit lesion plaques in STEMI patients are usually soft and adequate plaque modification can be easily achieved through DCB-PCI (< 30% residual stenosis and low grade of dissection).23 Moreover, the ruptured lipid rich plaque can potentially be an ideal reservoir for effective paclitaxel uptake.24 On the other hand, DCBs carry specific risks for STEMI patients, such as acute recoil and culprit lesion closure, because they don’t provide vessel scaffolding.
In our study, the proportion of patients presenting with ACS had no impact on treatment effects on the meta-regression analysis. Nevertheless, further RCT with adequate sample size are needed to obtain more solid evidence in this field. Of note, complex lesions (eg, severe calcification and bifurcations with planned two-stent technique) were excluded from the studies that included patients presenting with CCS.7,8 Therefore, our findings might not be generalized to this population.
The better angiographic surrogate outcomes with DES-PCI vs DCB-PCI found in our meta-analysis after pooling data from 6 studies can be explained by the absence of a metal scaffold to expand the vessel lumen and the acute recoil following balloon angioplasty. This justifies the lower MLD achieved after DCB-PCI vs DES-PCI. While our analysis did not show significant differences regarding LLL during follow-up, the value of LLL was lower among patients undergoing DCB-PCI when excluding the REVELATION trial.9,17 This study showed extremely low LLL in both DCB and DES groups vs other available evidence from RCT.15,16 The presence of positive vessel remodeling with a late lumen enlargement after the use of DCB evaluated by intracoronary imaging modalities has been evidenced in multiple studies, and seems to be associated with small vessel disease, fibrous and layered plaques and a post-PCI medial dissection arc > 90°.25,26,27 However, evidence of this phenomenon in patients with large vessel CAD is less known.22 It should, therefore, be noted that all studies in this meta-analysis used paclitaxel-DCB. While the evidence comparing sirolimus and paclitaxel-DCB is scarce, 2 recent RCT have shown better angiographic results with the lipophilic component. In the first one, with 121 patients with the novo small vessel CAD, sirolimus-DCB failed to achieve non-inferiority for net-lumen gain at 6 months.28 In the second study, with 70 patients, the 2 devices showed similar results of LLL at 6 months, although patients treated with paclitaxel-DCB had more frequent late luminal enlargement.29 Due to the small sample size and although there is not enough evidence to evaluate differences across clinical endpoints, we cannot assume that there is a class effect across all DCBs. There are larger ongoing RCT to evaluate the outcomes of sirolimus DCB vs DES in large vessels that will provide evidence in this field.30,31
Limitations
The results of our investigation should be interpreted in light of some limitations. First, this is a study-level meta-analysis providing average treatment effects. The lack of patient-level data from the included studies prevents us from assessing the impact of baseline clinical, angiographic and procedural characteristics on treatment effects. Second, minor differences in definition were present for some endpoints (eg, MACE), limiting the reliability of effect estimates. Third, one study which accounted for approximately 75% of all patients included did not included angiographic follow-up,7 thus limiting the evaluation of DCB and DES on angiographic outcomes. Fourth, the clinical follow-up varied from 6 to 24 months. Ideally, outcomes such as TLR should be compared at uniform follow-up across studies (eg, at 1 year), which was not consistently possible in the current analysis. Nonetheless, these differences in follow-up duration were accounted with the IRRs, as detailed in the Methods section. However, longer follow-ups are needed to establish the safety and efficacy profile of DCB vs DES throughout time. Fifth, the definition of large vessel is inconsistent across trials, which might be a source of bias. Finally, the limited number of studies and patients, and the small event rate for some endpoints, such as all-cause mortality may reduce the power for detecting significant differences across groups.
CONCLUSIONS
This meta-analysis provides the most updated quantitative evidence on the use of DCB vs DES for the treatment of de novo large vessel CAD in both CCS and ACS. DCB-PCI is associated with similar TLR and LLL at mid-term follow-up representing an appealing treatment option for patients with large vessel CAD.
FUNDING
None declared.
ETHICAL CONSIDERATIONS
Ethics approval was deemed unnecesary for this meta-analysis as all data were collected and synthesized from previous studies. Additionally, no informed consent was required as there were no patients involved in our work. The meta-analysis of RCT was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2009 guidelines. We confirm that sex/gender biases have been taken into consideration.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCE
No artificial intelligence has been used in the preparation of this article.
AUTHORS’ CONTRIBUTIONS
J. Llau Garcia, S. Huelamo Montoro and J. A. Sorolla Romero participated in literature research and study selection. J. A. Sorolla Romero, L. Novelli and J. Sanz Sánchez contributed to the conception, design, drafting and revision of the article. P. Rubio, JL Luis Díez Gil, L. Martínez-Dolz, IJ. Amat Santos, B. Cortese, F Alfonso, and Hector M. Garcia-Garcia contributed to the critical revision of the intellectual content of the article.
CONFLICTS OF INTEREST
F. Alfonso is an associate editor of REC: Interventional Cardiology; the journal’s editorial procedure to ensure impartial handling of the manuscript has been followed. The authors declared no relevant relationships with the contents of this paper.
WHAT IS KNOWN ABOUT THE TOPIC?
- DCB are a well-established treatment for patients with small-vessel CAD.
- Available published evidence of patients with de novo large vessel CAD is scarce and shows conflicting results.
WHAT DOES THIS STUDY ADD?
- In this meta-analysis including data from 2961 patients enrolled in 7 RCT, DCB showed similar risk of clinical events at follow-up vs DES in the treatment of de novo large vessel CAD.
- The use of DCB might be considered as an alternative option to DES in patients undergoing PCI for non-complex de novo large vessel CAD.
REFERENCES
1. Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40:87-165.
2. Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization:Executive Summary:A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145:e4-e17.
3. Kong MG, Han JK, Kang JH, et al. Clinical outcomes of long stenting in the drug-eluting stent era:patient-level pooled analysis from the GRAND-DES registry. EuroIntervention J Eur Collab Work Group Interv Cardiol Eur Soc Cardiol. 2021;16:1318-1325.
4. Kawai T, Watanabe T, Yamada T, et al. Coronary vasomotion after treatment with drug-coated balloons or drug-eluting stents:a prospective, open-label, single-centre randomised trial. EuroIntervention. 2022;18:e140?e148.
5. Jeger RV, Eccleshall S, Wan Ahmad WA, et al. Drug-Coated Balloons for Coronary Artery Disease:Third Report of the International DCB Consensus Group. JACC Cardiovasc Interv. 2020;13:1391-1402.
6. Sanz Sánchez J, Chiarito M, Cortese B, et al. Drug-Coated balloons vs drug-eluting stents for the treatment of small coronary artery disease:A meta-analysis of randomized trials. Catheter Cardiovasc Interv Off J Soc Card Angiogr Interv. 2021;98:66-75.
7. Gao C, He X, Ouyang F, et al. Drug-coated balloon angioplasty with rescue stenting versus intended stenting for the treatment of patients with de novo coronary artery lesions (REC-CAGEFREE I):an open-label, randomised, non-inferiority trial. Lancet Lond Engl. 2024;404:1040-1050.
8. Yu X, Wang X, Ji F, et al. A Non-inferiority, Randomized Clinical Trial Comparing Paclitaxel-Coated Balloon Versus New-Generation Drug-Eluting Stents on Angiographic Outcomes for Coronary De Novo Lesions. Cardiovasc Drugs Ther. 2022;36:655-664.
9. Vos NS, Fagel ND, Amoroso G, et al. Paclitaxel-Coated Balloon Angioplasty Versus Drug-Eluting Stent in Acute Myocardial Infarction:The REVELATION Randomized Trial. JACC Cardiovasc Interv. 2019;12:1691-1699.
10. Gobbi C, Giangiacomi F, Merinopoulos I, et al. Drug coated balloon angioplasty for de novo coronary lesions in large vessels:a systematic review and meta-analysis. Sci Rep. 2025;15:4921.
11. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses:the PRISMA statement. BMJ. 2009;339:b2535.
12. Sanz-Sánchez J, Chiarito M, Gill GS, et al. Small Vessel Coronary Artery Disease:Rationale for Standardized Definition and Critical Appraisal of the Literature. J Soc Cardiovasc Angiogr Interv. 2022;1:100403.
13. Nishiyama N, Komatsu T, Kuroyanagi T, et al. Clinical value of drug-coated balloon angioplasty for de novo lesions in patients with coronary artery disease. Int J Cardiol. 2016;222:113-118.
14. Wang Z, Yin Y, Li J, et al. New Ultrasound-Controlled Paclitaxel Releasing Balloon vs. Asymmetric Drug-Eluting Stent in Primary ST-Segment Elevation Myocardial Infarction-A Prospective Randomized Trial. Circ J Off J Jpn Circ Soc. 2022;86:642-650.
15. Gobic´D, Tomulic´V, Lulic´D, et al. Drug-Coated Balloon Versus Drug-Eluting Stent in Primary Percutaneous Coronary Intervention:A Feasibility Study. Am J Med Sci. 2017;354:553-560.
16. Hao X, Huang D, Wang Z, Zhang J, Liu H, Lu Y. Study on the safety and effectiveness of drug-coated balloons in patients with acute myocardial infarction. J Cardiothorac Surg. 2021;16:178.
17. Niehe SR, Vos NS, Van Der Schaaf RJ, et al. Two-Year Clinical Outcomes of the REVELATION Study:Sustained Safety and Feasibility of Paclitaxel-Coated Balloon Angioplasty Versus Drug-Eluting Stent in Acute Myocardial Infarction. J Invasive Cardiol. 2022;34:E39-E42.
18. Xue W, Ma J, Yu X, et al. Analysis of the incidence and influencing factors associated with binary restenosis of target lesions after drug-coated balloon angioplasty for patients with in-stent restenosis. BMC Cardiovasc Disord. 2022;22:493.
19. Coughlan JJ, Maeng M, Räber L, et al. Ten-year patterns of stent thrombosis after percutaneous coronary intervention with new- versus early-generation drug-eluting stents:insights from the DECADE cooperation. Rev Esp Cardiol. 2022;75:894-902.
20. Madhavan MV, Redfors B, Ali ZA, Prasad M, et al. Long-Term Outcomes After Revascularization for Stable Ischemic Heart Disease:An Individual Patient-Level Pooled Analysis of 19 Randomized Coronary Stent Trials. Circ Cardiovasc Interv.2020;13:e008565.
21. Buchanan KD, Torguson R, Rogers T, et al. In-Stent Restenosis of Drug-Eluting Stents Compared With a Matched Group of Patients With De Novo Coronary Artery Stenosis. Am J Cardiol. 2018;121:1512-1518.
22. Antonio Sorolla Romero J, Calderón AT, Tschischke JPV, Luis Díez Gil J, Garcia-Garcia HM, Sánchez JS. Coronary plaque modification and impact on the microcirculation territory after drug-coated balloon angioplasty:the PLAMI study. Rev Esp Cardiol. 2025;78:481-482.
23. Merinopoulos I, Gunawardena T, Corballis N, et al. Assessment of Paclitaxel Drug-Coated Balloon Only Angioplasty in STEMI. JACC Cardiovasc Interv. 2023;16:771-779.
24. Maranhão RC, Tavares ER, Padoveze AF, Valduga CJ, Rodrigues DG, Pereira MD. Paclitaxel associated with cholesterol-rich nanoemulsions promotes atherosclerosis regression in the rabbit. Atherosclerosis. 2008;197:959-966.
25. Kleber FX, Schulz A, Waliszewski M, et al. Local paclitaxel induces late lumen enlargement in coronary arteries after balloon angioplasty. Clin Res Cardiol Off J Ger Card Soc. 2015;104:217-225.
26. Alfonso F, Rivero F. Late lumen enlargement after drug-coated balloon therapy:turning foes into friends. EuroIntervention J Eur Collab Work Group Interv Cardiol Eur Soc Cardiol. 2024;20:523-525.
27. Yamamoto T, Sawada T, Uzu K, Takaya T, Kawai H, Yasaka Y. Possible mechanism of late lumen enlargement after treatment for de novo coronary lesions with drug-coated balloon. Int J Cardiol. 2020;321:30-37.
28. Ninomiya K, Serruys PW, Colombo A, et al. A Prospective Randomized Trial Comparing Sirolimus-Coated Balloon With Paclitaxel-Coated Balloon in De Novo Small Vessels. JACC Cardiovasc Interv. 2023;16:2884-2896.
29. Ahmad WAW, Nuruddin AA, Abdul KMASK, et al. Treatment of Coronary De Novo Lesions by a Sirolimus- or Paclitaxel-Coated Balloon. JACC Cardiovasc Interv. 2022;15:770-779.
30. Spaulding C, Krackhardt F, Bogaerts K, et al. Comparing a strategy of sirolimus-eluting balloon treatment to drug-eluting stent implantation in de novo coronary lesions in all-comers:Design and rationale of the SELUTION DeNovo Trial. Am Heart J. 2023;258:77-84.
31. Greco A, Sciahbasi A, Abizaid A, et al. Sirolimus-coated balloon versus everolimus-eluting stent in de novo coronary artery disease:Rationale and design of the TRANSFORM II randomized clinical trial. Catheter Cardiovasc Interv Off J Soc Card Angiogr Interv. 2022;100:544-552.
ABSTRACT
Introduction and objectives: This study reviewed the management of heart block following transcatheter device closure of perimembranous ventricular septal defects in pediatric patients.
Methods: We evaluated the follow-up and treatment of 1 patient who developed complete atrioventricular block and 5 patients who developed left bundle branch block (LBBB) from January 2019 through December 2023 after transcatheter ventricular septal defect closure in our clinic.
Results: All patients who developed heart block weighed less than 10 kg. The only patient who developed complete atrioventricular block was successfully treated with temporary pacing, returning to sinus rhythm. In 2 of the 5 patients with LBBB, conduction disturbances were observed during the procedure, leading to termination without device release. One patient with postoperative LBBB returned to sinus rhythm following steroid therapy, and another one required surgical device removal. The patient with late-onset LBBB is still under close follow-up with serial ECG and echocardiography.
Conclusions: Heart block after transcatheter closure of perimembranous ventricular septal defect is a serious complication, particularly in young patients with low body weight. Early detection and appropriate management, including procedural interruption, steroid therapy, and surgery when necessary, can lead to favorable outcomes. Careful patient selection and close follow-up are essential to minimize the risk of conduction disturbances.
Keywords: Atrioventricular block. Left bundle branch block. Pediatric patients. Perimembranous ventricular septal defects. Transcatheter closure.
RESUMEN
Introducción y objetivos: En este estudio se revisó el tratamiento del bloqueo cardiaco después del cierre con dispositivo percutáneo de defectos del tabique ventricular perimembranoso en pacientes pediátricos.
Métodos: Se evaluó el seguimiento y el tratamiento de 1 paciente que desarrolló bloqueo auriculoventricular completo y de 5 pacientes que desarrollaron bloqueo de rama izquierda (BRI), entre enero de 2019 y diciembre de 2023, tras del cierre percutáneo de una comunicación interventricular en nuestro centro.
Resultados: Todos los pacientes que desarrollaron bloqueo cardiaco pesaban menos de 10 kg. El único paciente que desarrolló un bloqueo auriculoventricular completo respondió al tratamiento médico con estimulación temporal y recuperó el ritmo sinusal. En 2 de los 5 pacientes con BRI se observó una anomalía de conducción durante el procedimiento, lo que llevó a finalizarlo sin liberar el dispositivo. Un paciente con BRI después del procedimiento recuperó el ritmo sinusal tras recibir tratamiento con esteroides, mientras que otro requirió la retirada quirúrgica del dispositivo. El paciente con BRI de aparición tardía permanece bajo vigilancia estrecha con electrocardiogramas seriados y ecocardiografía.
Conclusiones: El bloqueo que se desarrolla después del cierre percutáneo de una comunicación interventricular perimembranosa es una complicación grave, sobre todo en pacientes jóvenes con bajo peso corporal. La detección precoz y el tratamiento adecuado, incluida la interrupción del procedimiento, el tratamiento con esteroides y la intervención quirúrgica en caso necesario, pueden producir resultados favorables. La selección cuidadosa de los pacientes y un seguimiento estrecho son esenciales para minimizar el riesgo de alteraciones de la conducción.
Palabras clave: Bloqueo auriculoventricular. Bloqueo de rama izquierda. Pacientes pediátricos. Defectos septales ventriculares perimembranosos. Cierre percutáneo.
Abbreviations
CAVB: complete atrioventricular block. LBBB: left bundle branch block. LV: left ventricle. RV: right ventricle. VSD: ventricular septal defect.
INTRODUCTION
Transcatheter closure of ventricular septal defects (VSD) offers numerous advantages, including less trauma, faster recovery, and a reduced length of stay.1 However, this technique has complications, such as device embolization, valve malfunction, and arrhythmias. One of the most concerning complications of transcatheter closure of perimembranous VSD is the development of complete atrioventricular block (CAVB).2 Although this complication is more likely to occur when an inappropriate device is selected, pinpointing the exact cause of the block can sometimes be challenging. Factors significantly contributing to CAVB include young age, low body weight, device malapposition due to septal aneurysm, selection of an excessively large device, and direct device compression. Despite its rarity, CAVB remains a severe complication associated with this procedure.3
The atrioventricular node is located at the posterior superior area of the membranous ventricular septum and branches into the left and right bundles at the lower posterior edge. This close anatomical relationship increases the risk of developing heart block during the transcatheter closure of perimembranous VSD.1,4,5 Left anterior fascicular block, a variant of left bundle branch block (LBBB), can result in ventricular asynchrony, which negatively impacts hemodynamics and left ventricular function.6
CAVB has been reported in 0-6.4% of cases after the transcatheter closure of VSD.7 Recent publications indicate that this rate is gradually declining. A systematic review by Yang et al. found that 107 of 4394 patients, 107 (2.4%) required permanent pacemaker implantation after the interventional closure of VSD, with a higher incidence rate being reported in young children.8 Additionally, Bergman et al. reported that CAVB was observed in 1 of 149 (0.7%) patients after the procedure involving various VSD devices at a 6-year follow-up.7
We evaluated a total of 180 patients, 42 of whom were under 10 kg, who underwent transcatheter closure of VSD in our center in the last 5 years, focusing on block development in young children. In this article we detail the treatment and follow-up of 1 patient who developed complete CAVB and 5 patients who developed LBBB.
METHODS
From January 2019 through December 2023, a total of 180 pediatric patients (42 of whom weighed less than 10 kg) underwent transcatheter closure of perimembranous ventricular septal defects (VSD) at our center.
The indications for closure included a left ventricular end-diastolic diameter Z score ≥ 2.0; Qp/Qs > 1.5, treatment-resistant heart failure, a cardiothoracic ratio ≥ 0.55 on chest radiography, and growth retardation unrelated to recurrent respiratory infections or malnutrition.
Patients with subaortic edge regurgitation, significant aortic regurgitation, ventricular outflow tract obstruction, mean pulmonary artery pressure > 20 mmHg, or associated surgical heart anomalies were excluded from the study.
The KONAR-MF VSD occluder (Lifetech, China) and Amplatzer Duct Occluder (ADO I and II, AGA Medical Corp., United States) devices were used in the procedures. The Konar MF was used more frequently due to its flexible design (Konar MF: 157, ADO I + ADO II: 23).
The device size was selected based on angiographic measurements, typically choosing a device 1–2 mm larger than the size of the left ventricular defect. In VSD with aneurysmal tissue, the left disc of the device was positioned inside the aneurysmal tissue.
All patients were continuously monitored with electrocardiography during the procedure and underwent serial electrocardiograms (ECG) and echocardiographic evaluations at the follow-up.
RESULTS
Heart block developed in 6 patients, all of whom weighed less than 10 kg: 1 CAVB and 5 LBBB.
Case 1
A 2-year-old female patient, weighing 9.9 kg (3rd to 10th percentile), was being followed by pediatric cardiology for a diagnosis of a VSD. She had a past medical history of failure to gain weight, growth retardation, and 2 hospitalizations due to lower respiratory tract infections. An echocardiogram revealed a perimembranous VSD, measuring 5 mm on the left ventricular (LV) side and 4 mm on the right ventricular (RV) one.
Due to the clinical and hemodynamic significance of the patient’s VSD, a decision was made to perform a transcatheter closure. Prior to the procedure, the patient was administered cefazolin (50 mg/kg) and heparin (100 U/kg). The VSD was successfully closed using a Lifetech Konar MFO 6-4 device via antegrade access while the patient remained under general anesthesia. There were no signs of conduction disturbances in the ECG performed intra- and postoperatively. An ECG performed on postoperative day 2 confirmed that the device was correctly positioned in the absence of residual shunt. The patient was prescribed a 6-month regimen of aspirin at a dosage of 3 mg/kg/day and was discharged without any complications. Three days after discharge, the patient exhibited cyanosis. An ECG revealed the presence of CAVB (figure 1).
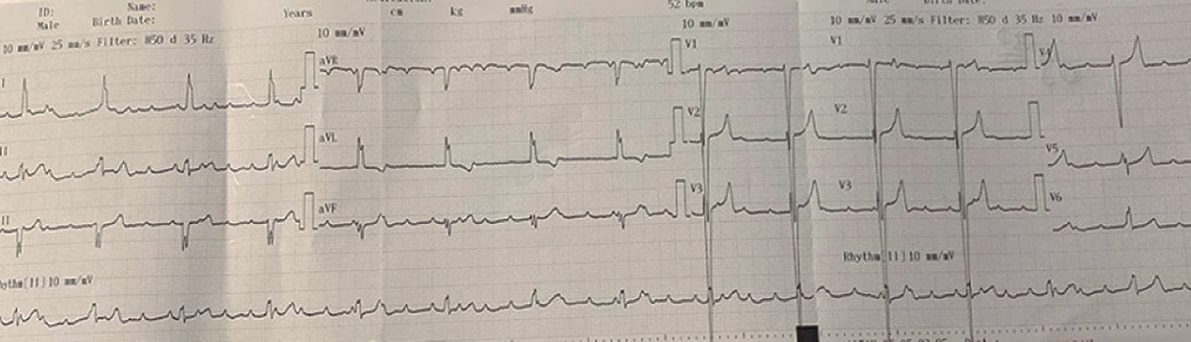
Figure 1. Case 1: electrocardiography of complete atrioventricular block after transcatheter closure of ventricular septal defect.
Atropine was administered twice at a dose of 0.02 mg/kg. The intervention successfully raised the peak heart rate to 135 beats per minute, and the patient’s rhythm normalized to a junctional ectopic rhythm. However, as the CAVB persisted, a temporary transvenous pacemaker was implanted, and the patient was admitted to the pediatric intensive care unit under continuous follow-up. Dexamethasone was initiated at a dosage of 0.6 mg/kg per day.
On hospitalization day 3, the patient’s ECG showed a return to sinus rhythm. After the temporary pacemaker was turned off, the patient underwent 24-hour Holter ECG monitoring. The Holter ECG showed a consistent sinus rhythm, meaning there was no evidence of CAVB or advanced second-degree block. On hospitalization day 5, the patient, whose ECG was still showing a consistent sinus rhythm, was discharged with a plan to complete a 10-day regimen of dexamethasone.
During the 3- and 6-month follow-up visits, the patient’s ECG continued to show a normal sinus rhythm without the need for medication.
Case 2
A 15-month-old male patient, weighing 8 kg (which is below the 3rd percentile), presented with a VSD and a large patent ductus arteriosus who underwent transcatheter closure at 3.5 months of age due to symptoms of heart failure that remained unresponsive to optimal medical therapy. During follow-up, the patient showed signs of inadequate weight gain and fatigue during feeding. Due to these clinical and hemodynamic indicators, a decision was made to close the VSD at 15 months of age. Echocardiography revealed a defect measuring 5 mm on the LV side and 4 mm on the RV side in the perimembranous region. The defect was closed using a transcatheter approach via retrograde access with a Lifetech Konar MFO 6-4 device.
Postoperative follow-up revealed the widening of the QRS complex. An ECG showed that the patient had developed a LBBB. As a result, the device was removed without being released. The patient then began dexamethasone at a dosage of 0.6 mg/kg per day.
By the end of week 1 of postoperative follow-up, the patient’s ECG showed a normal sinus rhythm with no evidence of LBBB.
Case 3
An 8-month-old patient, weighing 6.4 kg (below the 3rd percentile), was monitored for a VSD measuring 5 mm on the LV side and 4.5 mm on the RV side in the perimembranous region. Due to poor weight gain and left ventricular enlargement on the echocardiography, transcatheter closure was performed.
A Lifetech Konar MFO 6-4 device was successfully implanted under general anesthesia without immediate complications. However, 3 hours later, the patient developed a LBBB on the ECG (figure 2). Although dexamethasone was started at 0.6 mg/kg/day, the LBBB persisted by day 4, and the patient was discharged.
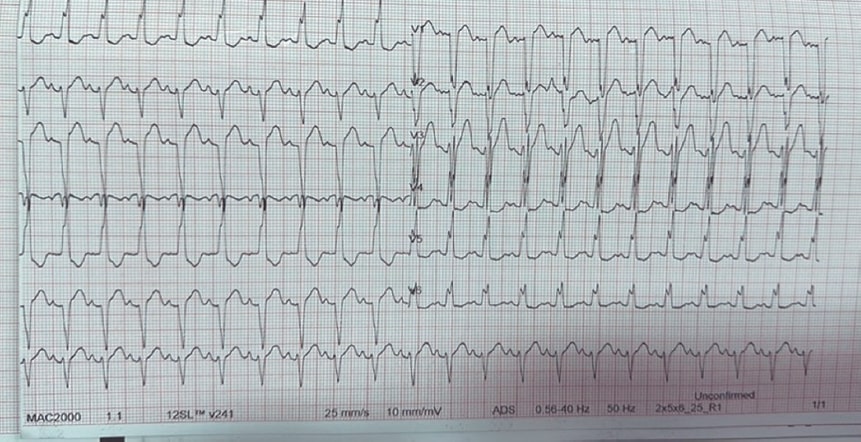
Figure 2. Case 3: electrocardiography of left bundle branch block after transcatheter closure of ventricular septal defect closure.
During the 1-week follow-up, an incomplete LBBB was noted on the ECG. Dexamethasone treatment went on for another 2 weeks, and at the 1-month follow-up, the LBBB had resolved, indicating successful treatment.
Case 4
A 14-month-old female patient, weighing 8 kg (which falls within the 3rd to 10th percentile), was being monitored for a VSD. The ECG indicated a 6 mm perimembranous VSD. A decision was made to perform the transcatheter closure of the defect. The procedure was performed with a Lifetech Konar MFO 8-6 device via retrograde access in the absence of immediate complications.
However, after the procedure, an ECG showed the development of LBBB. The patient began dexamethasone at a dosage of 0.6 mg/kg/day. After discharge, she was closely monitored through frequent outpatient follow-up. Despite ongoing treatment, LBBB persisted, and echocardiography performed at the 1-week follow-up showed onset of aortic regurgitation. At the 3-week follow-up, the device was surgically removed and the VSD repaired. This decision was made because her echocardiography showed increased aortic regurgitation, and the lLBBB persisted on her ECG.
Case 5
A 12-month-old male patient, weighing 7 kg (below the 3rd percentile), was admitted to the clinic with symptoms of growth retardation and evidence of left ventricular enlargement on echocardiography. The patient exhibited a perimembranous VSD measuring 6 mm on the LV side and 3.5 mm on the RV side. The defect was closed using a Lifetech Konar MFO 6-4 device, delivered through a transcatheter procedure, which went completed smoothly and without conduction disturbances being observed on the ECG at the follow-up. Echocardiography confirmed that the device had been implanted appropriately and in the absence of residual shunt. However, at the 4-year follow-up, LBBB was observed on the ECG. Since the left ventricular functions remained normal on echocardiography, the patient remained under close follow-up in the outpatient clinic without any additional treatment.
Case 6
A decision was made to perform a transcatheter closure of a VSD in an 11-month-old female patient who weighed 9 kg (falling within the 25th to 50th percentile). She had been on optimal medical therapy for heart failure and exhibited left ventricular dilatation on echocardiography. The defect measured 7 mm on the LV side and 4 mm on the RV side.
The procedure was performed via retrograde access using a Lifetech Konar MFO 7-5 device. After device implantation, QRS complex widening was observed on the monitor, and an ECG confirmed the development of LBBB. The device had to be removed without being released.
The patient began dexamethasone at a dose of 0.6 mg/kg/day. Four weeks after the procedure, the patient’s ECG showed a return to sinus rhythm in the absence of LBBB.
The patients’ demographic and clinical characteristics are shown in table 1.
Table 1. Demographic and clinical characteristics
| Case | Age, months | Body weight, kg | VSD LV side (mm) | VSD RV side (mm) | Device | VSA | Approach | Time of block developing | Block | Administration | Follow-up |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 25 | 9.9 | 5 | 4 | 6-4 | No | Antegrade | Day 4 | CAVB | Transient pacemaker | Sinus |
| 2 | 15 | 8 | 5 | 4 | 6-4 | No | Retrograde | Intraoperatively | LBBB | Not released | Sinus |
| 3 | 8 | 6.4 | 5 | 4.5 | 6-4 | No | Antegrade | Hour 2 | LBBB | Dexamethasone | Sinus |
| 4 | 14 | 8 | 6 | 5.5 | 8-6 | Yes | Retrograde | Hour 3 | LBBB | Surgery | Sinus |
| 5 | 11 | 7 | 6 | 3.5 | 6-4 | No | Retrograde | Year 4 | LBBB | Follow-up | LBBB |
| 6 | 11 | 9 | 7 | 4 | 7-5 | No | Antegrade | On the Intraoperatively | LBBB | Not released | Sinus |
|
CAVB, complete atrioventricular block; LBBB, left bundle branch block; LV, left ventricle; RV, right ventricle; VSA, ventricular septal aneurysm; VSD, ventricular septal defect. |
|||||||||||
DISCUSSION
Blocks that occur after transcatheter closure of perimembranous VSDs are primarily caused by the conduction bundle close proximity to the defect.9,10 The edge of the perimembranous VSD is located in an area of fibrous continuity between the atrioventricular valves, which forms the posteroinferior border. In this region, the atrioventricular conduction bundle leaves the central fibrous body and runs just subendocardial. This position makes it vulnerable to damage from devices used to close perimembranous VSDs.9
AVB due to direct mechanical compression of the atrioventricular node typically occur immediately after performing the procedure or 2 to 7 days after percutaneous closure. Later onset AVB may result from inflammation and fibrosis.2,9 CAVB are usually observed in the early postoperative period. In patients undergoing transcatheter closure, the timing of AVB formation can be unpredictable, with most cases being detected 2 to 7 days after the procedure.7,10 However, late-onset AVBs have been reported as late as 2 to 4 weeks or even 10 to 20 months after the procedure. The need for permanent pacemaker implantation is greater in younger patients.7 Although in our patient with complete AVB, symptoms developed 4 days after the procedure, there was no need for permanent pacemaker implantation.
After the perimembranous closure of VSD, bundle branch block is a more finding than CAVB. Right bundle branch block occurs more frequently than LBBB, likely because the right bundle branch is smaller and more prone to damage. While bundle branch blocks usually develop within 1 week after transcatheter closure, cases have been reported up to 3 years after the procedure.11 Most bundle branch blocks may resolve spontaneously or with steroid treatment, such as IV dexamethasone at 1 mg/kg/day or oral prednisone at 1-2 mg/kg/day.2,9 Close follow-up of patients is essential within the first 7 days after the procedure.10 LBBB has been reported to lead to abnormal left ventricular remodeling and heart failure.11
If CAVB occurs intraoperatively while crossing the defect, it is advisable to abandon the procedure. For postoperative CAVB, high doses of IV steroids followed by a 2-week regimen of oral steroids are recommended.9 The decision to remove the device is complex and depends on the patient’s symptoms, parental preference, and the experience of the clinic.9
If AVB resolves with steroid therapy, leaving the device in place is recommended. In symptomatic patients, a temporary pacemaker should be implanted, and response to steroid treatment should be monitored.9 In our patient with complete AVB, and in the 2 patients who developed postoperative LBBB, these blocks resolved after 2 weeks of steroid treatment, and sinus rhythm was restored. These patients have been closely monitored for any potential recurrence of the block.
For those patients who developed intraoperative bundle branch blocks, the devices were removed without release, as suggested in the literature.
In the patient who developed postoperative LBBB, which did not regress during follow-up, the device was surgically removed, and the VSD was repaired. The LBBB regressed with the removal of pressure on the left bundle branch.
Factors such as young age, low body weight, improper device positioning according to septal aneurysm and the choice of a large device have been identified as significant contributors to the development of conduction block.3 In our 5-year review, we observed that 5 of 180 cases of LBBB occurred in children weighing under 10 kg, which underscores the importance of age and body weight in the risk of developing LBBB.
To minimize the risk of a heart block, it is essential to prevent trauma and inflammation to the heart conduction tissue.4,7 This means an experienced operator should perform the procedure, using appropriately sized and flexible devices for the defect, and avoiding large carrier sheaths.7,9 The KONAR-MF VSD occluder, or KONAR-MFO, has become the primary choice in recent years for device selection due to its procedural flexibility, soft structure, and defect compatibility. We prefer to use KONAR-MFO in patients with low body weight and young age.3,12 While keeping septal aneurysmal tissue within the device during device implantation increases the risk of block, placing the left disc of the device inside the aneurysm may reduce the risk of block by removing it from the conduction system.13 Additionally, it is important to note that optimal medical therapy may be effective in cases without complete AVB basing the final treatment decision on the patient’s response.9
The reported rate of complete heart block after the surgical closure of VSD is < 2%. While the risk of CAVB (1-5%) in interventional closure of VSD raises concern, recent publications indicate a decreasing trend in the rates of CAVB.2,9,10 In our series, CAVB developed in only 1 patient (0.5%) and resolved with steroids after temporary transvenous pacing. Yang et al. (2012) reported that 8 of 228 patients (3.5%) developed postoperative LBBB.14 In a retrospective study of 2349 patients published in 2019, Wang et al. reported LBBB in 57 patients (2.4%) after the transcatheter closure of perimembranous VSD.11 In our center, LBBB developed in 5 of 180 transcatheter closures of VSD (2.7%), and the device was not implanted in 2 patients due to the development of intraoperative LBBB. Follow-up continues for our patient who developed late-onset LBBB.
Limitations
This study was conducted at a single center and retrospectively. Although patients were regularly monitored, longer follow-up periods are required, especially to detect conduction disturbance that may arise in the late period. Results may vary depending on the use of different devices or results obtained from different centers.
Considering these limitations, the findings should be interpreted with caution, particularly on the development of conduction block in low-birth-weight children. Further studies with larger sample groups, multicenter designs, and prospective follow-up data are required.
CONCLUSIONS
The risk of heart block in transcatheter procedures performed at experienced centers is lower than anticipated. Interventional closure of VSD has emerged as a viable alternative to surgery, providing benefits such as less trauma, faster recovery, and a reduced length of stay. With the arrival of newly developed devices, the risk of heart block in the transcatheter closure of VSD is steadily decreasing. Additionally, treatment often restores sinus rhythm in patients, and any heart block that may occur typically does not persist.
DATA AVAILABILITY
The raw data supporting the conclusions of this article will be made available by the authors upon request to any qualified researcher.
FUNDING
None declared.
ETHICAL CONSIDERATIONS
The study protocol was approved by the SBU Tepecik Training and Research Hospital ethics committee in full compliance with national rules and regulations and the ethical principles outlined in the revised Declaration of Helsinki (2008). Prior written informed consent and assent was obtained to participate in this study from each patient or caregiver. Furthermore, the authors confirm that sex and gender variables were considered in full compliance with the SAGER guidelines.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCE
No artificial intelligence technologies were utilized in the conception, data analysis, writing, or revision of this manuscript.
AUTHORS’ CONTRIBUTIONS
S. Oksuz and K. Yildiz designed the study protocol, analyzed the integrity of clinical data, and revised it. N. Narin and R. Aktas contributed to the conception and design, acquisition, and critically revised the manuscript, gave final approval, and agreed to be accountable for all aspects of work, ensuring integrity and accuracy. M.A. Atlan and S. Oksuz critically reviewed the article. R. Aktas and E. Gerceker contributed to the design, collected clinical data, and interpreted the results. C. Karadeniz provided editing and supervision. S. Oksuz took the lead in writing and reviewing the entire draft. All authors critically discussed the results and read and approved the final draft.
CONFLICTS OF INTEREST
None declared.
WHAT IS KNOWN ABOUT THE TOPIC?
- The transcatheter closure of perimembranous VSD offers advantages such as less trauma, faster recovery, and a reduced length of stay vs surgical procedures.
- One of the most serious complications of transcatheter closure is CAVB and LBBB, which can develop, particularly in small and low-weight children.
- The development of heart block may be associated with factors such as the anatomical proximity of the device to the conduction system, inappropriate and large device selection, and device malapposition relative to the septal aneurysm.
- The rate of CAVB has been reported between 0% and 6.4%. This rate, however, has been decreasing in recent years with the use of newly developed devices.
- Although CAVB and LBBB usually occur within the first week after the procedure, they can occur later as well.
- Early diagnosis, steroid therapy, temporary pacemaker implantation, and device removal if necessary can restore sinus rhythm in most cases.
WHAT DOES THIS STUDY ADD?
- This study presents original data on the development of conduction block following transcatheter perimembranous closure of VSD in underweight children.
- In particular, the use of new-generation, flexible, and small-sized devices (eg, Konar-MF) has demonstrated that procedural success and safety can be improved.
- The study highlights that serious complications, such as conduction block primarily emerge in the early stages; however, with appropriate patient selection, close follow-up, and prompt intervention, these complications can be largely reversed.
- By emphasizing the importance of patient selection and device selection in low-weight and small children, the study supports the transcatheter closure of VSD as a safe and effective option for this patient group.
- The study contributes to the literature, particularly in terms of complication management and device selection in high-risk patient groups.
REFERENCES
1. Schubert S. Current and new perspectives for interventional closure of ventricular septal defect. Kardiol Pol. 2021;79:378-379.
2. Bai Y, Xu X-D, Li C-Y, et al. Complete atrioventricular block after percutaneous device closure of perimembranous ventricular septal defect:A single-center experience on 1046 . Heart Rhythm. 2015;12:2132-2140.
3. Yildiz K, Narin N, Oksuz S, et al. Safety and efficacy of Amplatzer duct occluder II and Konar-MF™VSD occluder in the closure of perimembranous ventricular septal defects in children weighing less than 10 . Front Cardiovasc Med. 2023;10:1255808.
4. Landman G, Kipps A, Moore P, Teitel D, Meadows J.Outcomes of a modified approach to transcatheter closure of perimembranous ventricular septal defects. Catheter Cardiovasc Interv. 2013;82:143-149.
5. Saurav A, Kaushik M, Alla VM, et al. Comparison of percutaneous device closure versus surgical closure of peri-membranous ventricular septal defects:A systematic review and meta-analysis. Catheter Cardiovasc Interv. 2015;86:1048-1056.
6. Wu Z, Yang P, Xiang P, Ji X, Tian J, Li M. Left anterior fascicular block after transcatheter closure ofventricular septal defect in children. Front Cardiovasc Med. 2021;8:609531.
7. Bergmann M, Germann CP, Nordmeyer J, Peters B, Berger F, Schubert S. Short- and long-term outcome after interventional VSD closure:A single-center experience in pediatric and adult patients. Pediatr Cardiol. 2021;42:78-88.
8. Yang L, Tai BC, Khin LW, Quek SC. A systematic review on the efficacy and safety of transcatheter device closure of ventricular septal defects (VSD). J Interv Cardiol. 2014;27:260-272.
9. Walsh MA, Bialkowski J, Szkutnik M, Pawelec-Wojtalik M, Bobkowski W, Walsh KP. Atrioventricular block after transcatheter closure of perimembranous ventricular septal defects. Heart. 2006;92:1295-1297.
10. Butera G, Carminati M, Chessa M, et al. Transcatheter closure of perimembranous ventricular septal defects:Early and long-term results. J Am Coll Cardiol. 2007;50:1189-1195.
11. Wang C, Zhou K, Luo C, et al. Complete left bundle branch block after transcatheter closure of perimembranous ventricular septal defect. JACC Cardiovasc Interv. 2019;12:1625-1633.
12. Haddad RN, Houeijeh A, Odemis E, et al.MIOS-MFO, a multicenter international observational study of the Lifetech KONAR-MF ventricular septal defect occluder in treating perimembranous ventricular septal defects. Rev Esp Cardiol. 2025. https://doi.org/10.1016/j.rec.2025.02.010.
13. Jiang D, Zhang S, Zhang Y, et al. Predictors and long-term outcomes of heart block after transcatheter device closure of perimembranous ventricular septal defect. Front Cardiovasc Med. 2022;9:1041852.
14. Yang R, Kong X-Q, Sheng Y-H, et al. Risk factors and outcomes of post-procedure heart blocks after transcatheter device closure of perimembranous ventricular septal defect.JACC Cardiovasc Interv. 2012;5:422-427.
ABSTRACT
Introduction and objectives: Assessment and treatment of intermediate coronary lesions, defined as those which represent 30%-90% of the vessel lumen, remains a clinical challenge. Physiological evaluation techniques, such as fractional flow reserve (FFR), non-adenosine-based methods, such as instantaneous wave-free ratio or resting full-cycle ratio, and angiography-derived physiological assessment techniques (ADPAT) have transformed the diagnostic landscape. This meta-analysis aimed to systematically review and compare the diagnostic performance of ADPAT and FFR evaluating intermediate coronary lesions.
Methods: We conducted a systematic review of comparative research on FFR and ADPAT from January through February 2024.
Results: A total of 27 studies were finally included in the meta-analysis for a total of 4818 patients and 5440 vessels. Overall, a strong correlation between the different ADPAT and FFR was observed (r = 0.83; 95%CI, 0.80-0.85), with a mean ADPAT value of 0.82; 95%CI, 0.81-0.83 and a mean FFR of 0.83; 95%CI, 0.82-0.85. The summary area under the curve for predicting significant FFR (≤ 0.80) was excellent at 0.947. The overall sensitivity rate was 85% (95%CI, 81-87) with a specificity rate of 93% (95%CI, 91-94). The positive predictive value was 86% (95%CI, 83-88) with a total negative predictive value of 92% (95%CI, 91-94).
Conclusions: ADPAT show good correlation and concordance with FFR for intermediate coronary lesion evaluation. However, due to unfavorable outcomes observed in the FAVOR III Europe trial1 with quantitative flow ratio-guided revascularization, its clinical role should be reconsidered and potentially limited to scenarios where invasive assessment or adenosine use is not feasible. Further evaluation is warranted to confirm its diagnostic performance in broader clinical contexts.
Registered at PROSPERO: CRD420251042828.
Keywords: Clinical research. Fractional flow reserve. Angiographic/fluoroscopic. Meta-analysis.
RESUMEN
Introducción y objetivos: La evaluación y el tratamiento de las lesiones coronarias intermedias, definidas como aquellas que comprometen entre el 30 y el 90% de la luz del vaso, continúan representando un desafío clínico. Las técnicas de evaluación fisiológica (como la reserva fraccional de flujo [RFF]), los métodos que no requieren adenosina (como el índice instantáneo libre de ondas o el índice de ciclo completo en reposo) y las técnicas de evaluación fisiológica derivadas de la angiografía (ADPAT) han transformado el panorama diagnóstico. Este metanálisis tuvo como objetivo revisar sistemáticamente y comparar el rendimiento diagnóstico de las ADPAT frente a la RFF en la evaluación de lesiones coronarias intermedias.
Métodos: Entre enero y febrero de 2024 se realizó una revisión sistemática de investigaciones comparativas entre RFF y ADPAT.
Resultados: Se incluyeron 27 estudios en el metanálisis, con un total de 4.818 pacientes y 5.440 vasos. En general, se observó una fuerte correlación entre las distintas ADPAT y la RFF (r = 0,83; IC95%, 0,80-0,85), con un valor medio de ADPAT de 0,82 (IC95%, 0,81-0,83) y un valor medio de FFR de 0,83 (IC95%, 0,82-0,85). El área bajo la curva resumen para predecir una RFF significativa (≤ 0,80) fue excelente, con un valor de 0,947. La sensibilidad global fue del 85% (IC95%, 81-87) y la especificidad fue del 93% (IC95%, 91-94). El valor predictivo positivo fue del 86% (IC95%, 83-88) y el valor predictivo negativo total fue del 92% (IC95%, 91-94).
Conclusiones: Las ADPAT muestran una buena correlación y concordancia con la RFF en la evaluación de lesiones coronarias intermedias. Sin embargo, debido a los resultados desfavorables observados en el estudio FAVOR III Europe1 con la revascularización guiada por el índice cuantitativo de flujo, su papel clínico se debe reconsiderar y posiblemente limitar a escenarios en los que no sea factible realizar una evaluación invasiva ni utilizar adenosina. Se requiere una evaluación adicional para confirmar su rendimiento diagnóstico en contextos clínicos más amplios.
Registrado en PROSPERO: CRD420251042828.
Palabras clave: Investigación clínica. Reserva fraccional de flujo. Angiografía/fluoroscopia. Metanálisis.
Abbreviations
ADPAT: angiography-derived physiological assessment techniques. AUC: area under the curve. FFR: fractional flow reserve. QFR: quantitative flow ratio. uFR: Murray law-based quantitative flow reserve.
INTRODUCTION
Assessment and treatment of intermediate coronary lesions (those where percent diameter stenosis accounts for 30%-90% of the vessel lumen) remains a clinical challenge.1 Over the past 10 years this field has undergone significant changes, primarily due to theoretical and technological advances in physiological evaluation techniques.2,3
Prior to the existence of these techniques, the assessment of intermediate lesions was based on the degree of relative narrowing of the vessel lumen vs healthy segments, being this reduction subjectively determined by the operator, without knowledge of its physiological repercussion.2 The development of pressure guidewire methods, along with their validation and proven prognostic significance (particularly in the context of chronic coronary syndrome) from the late 1990s to the early 2000s,4 has led to substantial progress in intermediate lesions evaluation, which has enabled a more accurate classification based on their clinical relevance.5
The initial method developed, and still considered the gold standard, is fractional flow reserve (FFR).5 This technique estimates blood flow across a coronary lesion by measuring pressure differences.6 To make this estimation between pressure and flow, maximal coronary vessel hyperemia, primarily achieved through adenosine infusion, is necessary.6 FFR is defined as significant if flow difference across the lesion is > 20% (FFR ≤ 0.80).6 Beyond merely identifying which lesions benefit from revascularization, FFR has shown improved survival vs revascularization based on relative narrowing assessment. Furthermore, it has allowed lesion exclusion where revascularization is deemed unnecessary, thus reducing stent implantation rates and any potential complications associated with both this procedure and antiplatelet therapy.7
Despite the clear benefits of using intracoronary physiology, the need for invasive pressure guidewires, IV adenosine (with its potential complications), the time required, and even the outright rejection by interventional cardiologist may have led to a lower than expected adoption.8 These limitations triggered the appearance of non-adenosine-based methods, such as the instantaneous wave-free ratio (iFR) or resting full-cycle ratio.9,10 These methods use a specific moment of the cardiac cycle (for example the iFR uses the diastolic wave-free period) where microvascular resistances are minimal, allowing correlation between pressures and flow without the use of adenosine.11,12 However, despite eliminating this limitation, the use of pressure guidewires is still a barrier.8
Simultaneously with the development of these adenosine-free techniques, angiography-derived physiological assessment techniques (ADPAT) emerged, enabling the physiological evaluation of coronary lesions without the need for a guidewire or adenosine. These techniques, initially derived from those used in coronary lesion assessment in computational tomography,13 are based on the computational evaluation of lesions through fluid dynamics in coronary angiography. Since then, multiple options have emerged including QFR, Murray law-based quantitative flow ratio (uFR), vessel fractional flow reserve (vFRR), fractional flow reserve derived from routine coronary angiography (FFRangio) and coronary angiography-derived fractional flow reserve (CaFFR). All of them have been validated and compared with the gold standard FFR in prospective direct comparative studies of diagnostic accuracy.14-20
The aim of this article was to provide a review of the different validation studies of ADPAT vs FFR and offer a meta-analysis on the accuracy of each option, both collectively and individually.
METHODS
Literature search strategy
We conducted a systematic review of comparative research on FFR and ADPAT from January through February 2024. The PubMed database was used to search for articles on concordance, agreement, and diagnostic accuracy. Multiple searches were conducted using the following algorithm: FFR/FFR permuted with each mainly commercialized tool (QFR, uFR, vFRR, FFRangio and CaFFR) while trying to avoid CT and articles developed mainly in acute coronary syndrome through the commands “NOT (CT) NOT (“acute coronary syndrome”)”. Date range was limited from January 2012 through December 2023. PRISMA statement guidelines were followed, and the review was prospectively registered in the International Prospective Register of Systematic Reviews (PROSPERO) with registration No. CRD420251042828.
Eligible criteria
A total of 4580 terms were identified through the entire search process. These terms and their combinations were carefully selected by 2 different operators to refine the search for articles comparing the main ADPAT from the main commercial vs FFR. Articles involving coronary computed tomography angiography and those where comparisons were mainly drawn within the context of acute coronary syndrome were also excluded by the operators. Based on these criteria, an initial pool of studies was established.
A total of 15 studies were subsequently excluded based on prespecified criteria, including those that specified the presence of patients with concurrent or treated aortic stenosis, had more than 25% of patients diagnosed with atrial fibrillation, or involved angiography- derived physiological assessments for coronary lesions conducted within the first 29 days of acute myocardial infarction (either on the culprit lesion or non-culprit lesions).
In cases where the time elapsed from myocardial infarction to angiography-derived evaluation was nonspecific; articles were also excluded if more than 30% of patients had undergone coronary angiography due to acute myocardial infarction.
Furthermore, studies specifying the presence of 10% or more patients with prior surgical revascularization were excluded, as were those where the comparison between angiography-based physiological assessment methods and FFR was conducted on mammary artery grafts, radial artery grafts, or saphenous vein grafts.
After applying the selection criteria, a total of 29 articles were initially chosen for analysis. However, 2 articles (FAST [virtual FFR])21 and Ai et al.22 were subsequently excluded because they did not provide or calculate sensitivity and specificity data from their analyses. Consequently, the final analysis included 27 articles.
Two articles were divided and included as different items in the analysis as they showed 2 different analyzed cohorts on their studies: Smit et al.,23 where QFR was compared with the FFR in 2 cohorts: 1 with diabetes mellitus and the other without the disease; Zuo et al.24 divided patients in 2 cohorts based on whether the vessel was severely calcified or not. The uFR was compared with the FFR in each group. Each cohort was included in our analysis. Finally, the study by Emori et al.25 “Diagnostic accuracy of quantitative flow ratio for assessing myocardial ischemia in prior myocardial infarction,” presented 2 distinct cohorts based on the presence of prior myocardial infarction (≥ 30 days from coronary angiography). Although one cohort depicted an acute coronary syndrome scenario, it fulfilled our inclusion criteria, leading to the inclusion of both cohorts in the final analysis.
Statistical and methodologic analysis
The homogeneity across studies was contrasted using the QH statistic. Regarding the low sensitivity of this test, P < .10 values were considered significant. To overcome this limitation, the I2 statistic was estimated as well, which measures the proportion of the total variation of the studies, explained by the heterogeneity and its 95% confidence interval (95%CI). A random effects model was used for all cases using the pooled method of DerSimonian Laird. If heterogeneity was present, meta-regression analyses were conducted to explore the sources of heterogeneity (figure 1 of the supplementary data). The presence of publication bias was tested using the Deek funnelplot (figure 2 of the supplementary data).

Figure 1. Selected articles flowchart and exclusion criteria. ADPAT, angiography-derived physiological assessment techniques; AMI, acute myocardial infarction.

Figure 2. Summary receiver operating characteristic (SROC) curves and Q* index for subgroup analyses of software-derived coronary angiography-derived fractional flow reserve (caFFR); FFR, fractional flow reserve; QFR, quantitative flow ratio; uFR, Murray law-based quantitative flow reserve; VFAI, vessel fractional anatomy index; vFFR, vessel fractional flow reserve.
From the reported values of sensitivity, specificity, negative predictive value, positive predictive value, accuracy, and the number of vessels assessed, all 2 × 2 tables for the 0.8 cutoff point of the tests were constructed. Subsequently, pooled estimates for sensitivity, specificity, positive predictive value, negative predictive value, positive likelihood ratio, and negative likelihood ratio were derived from these data.26
The confidence intervals of sensitivity and specificity were calculated using the F distribution method to compute the exact confidence limits for the binomial proportion (x/n). The summary receive operator curve (SROC) was also calculated from which we drew all the points of sensitivity and 1-specificity and adjusted the weighted regression curve using Moses’ Model. Spearman correlation coefficient between sensitivity and specificity was used to assessed constant diagnostic odds ratio (positive likelihood ratio and negative likelihood ratio) employing a symmetric SROC.27 The area under curve (AUC) was computed by numeric integration of the curve equation using the trapezoidal method. Additionally, we applied the bootstrap methods for estimated AUC of multiple SROC. We provided the resultant bootstrap P values and 95%CI of the AUC for pairwise comparisons of the different methods (table 1 of the supplementary data). Furthermore, we provided an influence diagnostic method based on the AUC by performing leave-one-study-out analyses (table 2 of the supplementary data). Pearson correlation coefficients were transformed into Fisher’s z-values to calculate variance and we performed a meta-analysis and calculated the 95%CI (figure 3 of the supplementary data). Fagan’s Nomogram (figure 4 of the supplementary data) was used to graphically estimate how the result from a diagnostic test altered the probability of a patient having a disease. We assessed applicability and risk of bias based on the modified version of the QUADAS-2 tool28 (figure 5A,B of the supplementary data). All analyses were conducted using R Statistical Software (v4.2.0; R Core Team 2022) and performed using dmetatools R package (1.1.1; Noma H 2023), mada R package (0.5.11; Sousa-Pinto 2022) and TeachingDemos R package (2.13; Greg Snow 2024).
Table 1. Patients’ baseline characteristics
| Patients’ baseline characteristics (n = 4818) | |
|---|---|
| Characteristics (cohorts where this data is available) | (± 95%CI) or % |
| Mean age (26) | 66.4 ± 1.3 |
| Male (26) | 3318 (68.9%) |
| Mean BMI (kg/m2) (17) | 26 ± 0.8 |
| Hypertension (25) | 3189 (66.2%) |
| Diabetes (25) | 1263 (26.2%) |
| Dyslipidemia (21) | 2438 (50.6%) |
| Mean LVEF (%) (10) | 59.6 ± 3.3 |
| Prior or current smoker (23) | 1406 (29.2%) |
| Prior MI (20) | 566 (11.7%) |
| Prior PCI (20) | 1314 (27.3%) |
| Prior CABG (13) | 47 (1%) |
|
BMI, body mass index; CABG, coronary artery bypass grafting; LVEF, left ventricular ejection fraction; MI, myocardial infarction; PCI, percutaneous coronary intervention. Data are expressed as mean value and standard deviation across the studies. |
|
Table 2. Indications for cardiac catheterization
| Indication for cardiac catheterization | (%) |
|---|---|
| Silent isquemia | 323 (6.8) |
| Stable angina | 2483 (51.5) |
| Acute coronary syndrome | 1475 (30.6) |
| Unstable angina | 1142 (23.7) |
| AMI | 333 (6.9) |
| NSTEMI | 204 (4.2) |
| STEMI | 13 (0.3) |
| MI subtype not specified | 116 (2.4) |
| Others | 127 (2.6) |
|
AMI, acute myocardial infarction; MI, myocardial infarction; NSTEMI, non-ST-segment elevation myocardial infarction; STEMI, ST-segment elevation myocardial infarction. |
|

Figure 3. Forest plots and summary statistics for sensitivity and specificity estimates from a meta-analysis of FFR across different indices, using a random-effects model. 95%CI, 95% confidence interval; caFFR, coronary angiography–derived fractional flow reserve; FFR, fractional flow reserve; QFR, quantitative flow ratio; uFR, Murray law-based quantitative flow reserve; VFAI, vessel fractional anatomy index; vFFR, vessel fractional flow reserve. Xu et al.,16 2017; Fearon et al.,36 2019; Yuasa et al.,33 2023; Morris et al.,39 2013; Westra et al.,29 2018; Echavarría-Pinto et al.,31 2022; Stähli et al.,34 2019; Omori et al.,35 2019; Westra et al.,17 2018; Li et al.,18 2020; Pellicano et al.,14 2017; Emori et al.,25 2018; Tu et al.,15 2014; Zuo et al.,24 2024; Tu et al.,19 2021; Omori et al.,42 2023; Hrakesh et al.,32 2020; Kornowski et al.,37 2016; Masdjedi et al.,20 2022; Tröbs et al.,38 2016; Yazaki et al.,30 2017; Smit et al.23 2019; Daemen et al.,43 2022; and Papafaklis et al.,41 2014.

Figure 4. Forest plots and summary statistics for positive predictive value (PPV) and negative predictive value (NPV) estimates from a meta-analysis of FFR across different indices, using a random-effects model. 95%CI, 95% confidence interval; caFFR, coronary angiography–derived fractional flow reserve; FFR, fractional flow reserve; QFR, quantitative flow ratio; uFR, Murray law-based quantitative flow reserve; VFAI, vessel fractional anatomy index; vFFR, vessel fractional flow reserve. Xu et al.,16 2017; Fearon et al.,36 2019; Yuasa et al.,33 2023; Morris et al.,39 2013; Westra et al.,29 2018; Echavarría-Pinto et al.,31 2022; Stähli et al.,34 2019; Omori et al.,35 2019; Westra et al.,17 2018; Li et al.,18 2020; Pellicano et al.,14 2017; Emori et al.,25 2018; Tu et al.,15 2014; Zuo et al.,24 2024; Tu et al.,19 2021; Omori et al.,42 2023; Hrakesh et al.,32 2020; Kornowski et al.,37 2016; Masdjedi et al.,20 2022; Tröbs et al.,38 2016; Yazaki et al.,30 2017; Smit et al.,23 2019; Daemen et al.,43 2022; and Papafaklis et al.,41 2014.
RESULTS
Finally, a total of 27 articles were suitable for inclusion, as illustrated in figure 1. From these articles, a total of 4818 patients and 5440 vessels were added to the analysis. The population characteristics and mean cardiovascular risk factors are detailed in table 1 highlighting the existence of 3189 (66.18%) patients with hypertension, 2438 (50.6%) with dyslipidemia, and 1263 (26.2%) with diabetes. Notably, most patients included in the study were men (68.86% of the sample).
Thirteen of the selected articles were prospective in design. The most extensively studied vessel was the left anterior descending coronary artery (2921; 53.69%), followed by the right coronary artery (1075; 19.61%) and the left circumflex artery (772; 14.2%). Additionally, 89 left main coronary arteries were analyzed, accounting for 1.6% of all vessels. Angiography was primarily performed for stable angina (2483; 51.53%). Of note, while 1475 (30.61%) angiographies were prompted by acute coronary syndrome, only 333 (6.9% of the total) were performed in the context of acute myocardial infarction with or without ST-segment elevation, and the remaining 1142 in the context of unstable angina. Indications for cardiac catheterization are shown in table 2. The left anterior descending coronary artery was the most frequently studied vessel, accounting for 2921 patients (53.7% of the total studies). Proportions for other vessels are available in table 3.
Table 3. Number of studies per vessel performed across the different studies
| Vessel characteristics (n = 5440) | (%) |
|---|---|
| Left main coronary artery | 89 (1.7) |
| Left anterior descending coronary artery | 2921 (53.7) |
| Diagonal branch | 52 (1) |
| Ramus intermedius | 54 (1) |
| Left circumflex artery | 772 (14.2) |
| Obtuse marginal branch | 108 (2) |
| Right coronary artery | 1075 (19.8) |
| Posterolateral branch | 7 (0.1) |
| Interventricular branch | 8 (0.15) |
The QFR15-17,23,25,29-34 (QAngio XA 3D QFR, Medis Medical Imaging System; The Netherlands) was the most widely used software with a total of 13 patient cohorts from 11 articles, comprising 1987 patients and 2315 vessels, which accounts for 41.2% and 42.6% of the total, respectively. The correlation between QFR and FFR was excellent, showing an r = 0.82 (95%CI, 0.77-0.877). The overall sensitivity rate of QFR was 84% (95%CI, 80-88) with a specificity rate of 90% (95%CI, 87-93). The positive predictive value was 81% (95%CI, 77-84) with a total negative predictive value of 92% (95%CI, 90-94). The AUC for this technique was 0.937.
The second most analyzed technique, with a total of 5 articles, was FFRangio14,35-38 (Cathworks FFRangio, Israel), where this technology was employed in 696 patients and 841 vessels (14.4% and 15.45% of the total, respectively). The overall sensitivity rate of FFRangio was 90% (95%CI, 83-94) with a specificity rate of 95% (95%CI, 91-97). The positive predictive value was 90% (95%CI, 85-93) with a total negative predictive value of 94% (95%CI, 91-96).
vFFR (Pie Medical Imaging, The Netherlands) on the other hand, had an excellent correlation with FFR across the 3 included studies,20,39,40 contributing 647 patients and 663 vessels to the analysis (representing 13.42% of patients and 11.96% of vessels). The mean sensitivity and specificity rates were 82% (95%CI, 72-89) and 0.94% (95%CI, 89-97), respectively. The summary positive predictive value was 89% (95%CI, 82-93), and the summary negative predictive value, 91% (95%CI, 86-94).
Following its recent validation in 2022, the uFR (AngioPlus, Pulse Medical Imaging Technology, China) is supported by only 2 articles,19,24 one of which includes 2 cohorts based on vessel calcification. The uFR had a sensitivity rate of 80% (95%CI, 69-87) and a specificity rate of 0.94 (95%CI, 89-97). The summary positive predictive value was 85% (95%CI, 79-90), and the summary negative predictive value, 91% (95%CI, 87-94).
Only 1 article of CaFFR (Flashangio, Rainmed Ltd., China) was included.18
The analysis included 2 non-commercialized tools, VFAI41 and AngioFFR,42 which were not individually evaluated. Both were compared to FFR only once.
Overall, a strong correlation between the different ADPAT and FFR was observed (r = 0.83, 95%CI, 0.80-0.85), with a mean ADPAT value of 0.82 (95%CI, 0.81-0.83) (all the ADPAT set a value ≤ 0.80 for lesion significance) and a mean FFR of 0.83 (95%CI, 0.82-0.85).
The summary AUC for predicting significant FFR (≤ 0.80) was excellent at 0.947. The SROC for the different ADPAT is shown in figure 2.
The overall sensitivity rate was 85% (95%CI, 81-87) with a specificity rate of 93% (95%CI, 91-94). The positive predictive value was 86% (95%CI, 83-88) with a total negative predictive value of 92% (95%CI, 91-94). The main commercially available ADPAT values of sensibility, specificity, positive predictive value and negative predictive value are shown in figure 3 and figure 4.
DISCUSSION
Key findings
Our key findings were: a) ADPAT emerge as a reliable and practical method for assessing the physiological significance of intermediate coronary lesions, which is consistent with previous literature.44-46 ADPAT consistently demonstrates agreement with the current gold standard (FFR) regarding mean values and lesion classification, without vasodilator medication or pressure guidance; b) By summarizing the diagnostic capabilities of each ADPAT from the included studies, we were able to perform the first direct comparison of various angiography-based methods for evaluating coronary lesions. We presented the main commercially available options and their respective diagnostic accuracies relative to FFR. Additionally, an overview of these techniques was provided; c) We also included innovative methods, such as uFR, based on Murray’s Law, while offering a unique approach by using a single projection to estimate lesion significance, potentially overcoming a significant limitation of current techniques, which often require specific projections and a certain quality image.
The overall results confirmed that different ADPAT serve as an appropriate method for evaluating intermediate coronary lesions, as they demonstrated a strong correlation with FFR. This correlation extended to sensitivity, specificity, and predictive values as illustrated in figure 4. Notably, the studies exhibited homogeneity without significant discrepancies in their weighting within the analysis, as observed through the resampling techniques employed.
In comparative analysis, while ADPAT exhibit adequate sensitivity and positive predictive values regarding lesion significance, their specificity and negative predictive value exceed 90%. This high specificity allows ADPAT to more accurately identify physiologically non-significant lesions, thereby avoiding unnecessary revascularization.
From a technical standpoint, it was notable that these results were primarily obtained from assessments of the left anterior descending coronary artery (53.6%), with only 1 dedicated study on the left main coronary artery. Despite this, left main coronary arteries contributed a significant proportion (1.66%) to the overall analysis, showcasing proficient classification of significant lesions (AUC = 0.82) and indicating the feasibility of applying tools in this context.
QFR was the most frequently included tool in the analysis, representing 13 out of 27 cohorts. Despite multiple validations vs the FFR in diverse contexts, most studies align closely, demonstrating a correlation between QFR and FFR.
Comparing results across different tools, minimal differences were observed, with FFRangio and CaFFR showing slightly superior overall results vs other methods. However, it’s important to note that the results of the CaFFR are based solely on validation articles, and when considering only validation studies, results among tools are very similar.
Although QFR is frequently studied, its results might require more robust validation because there are limited articles on FFRangio, especially on chronic coronary syndrome in patient groups like those with left main disease or diabetes.
While ADPAT have been validated vs the FFR in various clinical scenarios, such as severe aortic stenosis, atrial fibrillation, or non-culprit coronary lesions in acute coronary syndrome, the inclusion of these scenarios in our analysis could potentially bias the results due to variations in study characteristics and the unique features of each disease affecting lesion assessment.
The limitation of this study stems from including a large proportion of pivotal studies for each analyzed tool, which were not performed under real-world clinical conditions. Consequently, the applicability of their results may be restricted, as demonstrated by a recent study from independent laboratories comparing the 5 main non-hyperemic indices with FFR under real-life conditions.47
Although the study demonstrated a good correlation between the indices and FFR, the levels of diagnostic accuracy reported in the pivotal studies were not achieved.
In this regard, QFR has been recently evaluated vs the FFR in the FAVOR III Europe trial,1 which included 2000 patients who were randomized (1:1) to QFR-guided or FFR-guided treatment of intermediate lesions. The results showed that the QFR-guided group had higher rates of mortality, myocardial infarction, and unplanned revascularization at 12 months.
Although these findings may initially seem discouraging, they do not contradict the results of our study, in which non-hyperemic indices demonstrated superior performance over conventional angiography in the functional classification of lesions. Therefore, their use remains valuable in clinical scenarios where invasive assessment with a pressure guidewire or the use of adenosine is not feasible or contraindicated.
Of note, while QFR is currently the most widely used non-hyperemic index, it is the only one that has been evaluated in clinical trials with hard clinical endpoints vs FFR. Other tools with promising results are still to be investigated in this context.
CONCLUSIONS
Substantial correlations and concordances have been demonstrated between ADPAT and FFR. These techniques have also shown accurate categorization of lesions deemed significant by the current gold standard (FFR). However, the results of the FAVOR III Europe study1 indicate that QFR–guided revascularization, compared with FFR-guided revascularization, is associated with higher rates of mortality, myocardial infarction, and unplanned revascularization. Therefore, the current role of ADPAT requires re-evaluation.
In this context, the use of QFR may be most appropriate when invasive assessment using a pressure guidewire is not feasible or when adenosine is contraindicated. Additionally, due to the unique characteristics of other clinical scenarios, further reviews are warranted to evaluate the diagnostic accuracy of this index.
FUNDING
C. Cortés-Villar is beneficiary of a Contrato Río Hortega grant from Instituto de Salud Carlos III with code CM22/00168.
ETHICAL CONSIDERATIONS
The present study was conducted in full compliance with the clinical practice guidelines set forth in the Declaration of Helsinki for clinical research and was approved by the ethics committees of the reference hospital (Hospital Clínico Universitario de Valladolid) and other participant centers. Possible sex- and gender-related biases were also taken into consideration according to the SAGER recommendations.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCE
No artificial intelligence was used in the writing of this text.
AUTHORS’ CONTRIBUTIONS
J. Ruiz-Ruiz and C. Cortés-Villar participated in the study design, data analysis, manuscript drafting, and critical revision. C. Fernández-Cordón and M. García-Gómez contributed to data collection and results analysis. A. Lozano-Ibáñez and D. Carnicero-Martínez contributed to data gathering. S. Blasco-Turrión and M. Carrasco-Moraleja contributed to the statistical analysis. J.A. San Román-Calvar and I.J. Amat-Santos performed the final review and approved the version for publication.
CONFLICTS OF INTEREST
None declared.
REFERENCES
1. Andersen BK, Sejr-Hansen M, Maillard L, et al. Quantitative flow ratio versus fractional flow reserve for coronary revascularisation guidance (FAVOR III Europe):a multicentre, randomised, non-inferiority trial. Lancet. 2024;404:1835-1846.
2. Patil CV, Beyar R. Intermediate coronary artery stenosis:Evidence-based decisions in interventions to avoid the oculostenotic reflex. Int J Cardiovasc Intervent. 2000;3:195-206.
3. Gould KL, Lipscomb K, Hamilton GW. Physiologic basis for assessing critical coronary stenosis. Instantaneous flow response and regional distribution during coronary hyperemia as measures of coronary flow reserve. Am J Cardiol. 1974;33:87-94.
4. De Bruyne B, Paulus WJ, Vantrimpont PJ, Sys SU, Heyndrickx GR, Pijls NHJ. Transstenotic coronary pressure gradient measurement in humans:In vitro and in vivo evaluation of a new pressure monitoring angioplasty guide wire. J Am Coll Cardiol. 1993;22:119-126.
5. Sousa-Uva M, Neumann FJ, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur J Cardio-thoracic Surg. 2019;55:4-90.
6. Tonino PAL, De Bruyne B, Pijls NHJ, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2011;365:213-224.
7. De Bruyne B, Pijls NHJ, Kalesan B, et al. Fractional Flow Reserve–Guided PCI versus Medical Therapy in Stable Coronary Disease. N Engl J Med. 2012;367:991-1001.
8. Johnson NP, Koo BK. Coronary Psychology:Do You Believe?JACC Cardiovasc Interv. 2018;11:1492-1494.
9. De Waard GA, Di Mario C, Lerman A, Serruys PW, Van Royen N. Instantaneous wave-free ratio to guide coronary revascularisation:Physiological framework, validation and differences from fractional flow reserve. EuroIntervention. 2017;13:450-458.
10. Svanerud J, Ahn JM, Jeremias A, et al. Validation of a novel non-hyperaemic index of coronary artery stenosis severity:The Resting Full-cycle Ratio (VALIDATE RFR) study. EuroIntervention. 2018;14:806-814.
11. Davies JE, Sen S, Dehbi H-M, et al. Use of the Instantaneous Wave-free Ratio or Fractional Flow Reserve in PCI. N Engl J Med. 2017;376:1824-1834.
12. Götberg M, Christiansen EH, Gudmundsdottir IJ, et al. Instantaneous Wave-free Ratio versus Fractional Flow Reserve to Guide PCI. N Engl J Med. 2017;376:1813-1823.
13. Min JK, Leipsic J, Pencina MJ, et al. Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. Jama. 2012;308:1237-1245.
14. Pellicano M, Lavi I, De Bruyne B, et al. Validation study of image-based fractional flow reserve during coronary angiography. Circ Cardiovasc Interv. 2017;10:E005259.
15. Tu S, Barbato E, Köszegi Z, et al. Fractional flow reserve calculation from 3-dimensional quantitative coronary angiography and TIMI frame count:A fast computer model to quantify the functional significance of moderately obstructed coronary arteries. JACC Cardiovasc Interv. 2014;7:768-777.
16. Xu B, Tu S, Qiao S, et al. Diagnostic Accuracy of Angiography-Based Quantitative Flow Ratio Measurements for Online Assessment of Coronary Stenosis. J Am Coll Cardiol. 2017;70:3077-3087.
17. Westra J, Andersen BK, Campo G, et al. Diagnostic performance of in-procedure angiography-derived quantitative flow reserve compared to pressure-derived fractional flow reserve:The FAVOR II Europe-Japan study. J Am Heart Assoc. 2018;7:e009603.
18. Li J, Gong Y, Wang W, et al. Accuracy of Computational Pressure-Fluid Dynamics applied to Coronary Angiography to Derive Fractional Flow Reserve –FLASH FFR. Cardiovasc Res. 2020;116:1349-1356.
19. Tu S, Ding D, Chang Y, Li C, Wijns W, Xu B. Diagnostic accuracy of quantitative flow ratio for assessment of coronary stenosis significance from a single angiographic view:A novel method based on bifurcation fractal law. Catheter Cardiovasc Interv. 2021;97(S2):1040-1047.
20. Masdjedi K, Tanaka N, Van Belle E, et al. Vessel fractional flow reserve (vFFR) for the assessment of stenosis severity:the FAST II study. EuroIntervention. 2022;17:1498-1505.
21. Masdjedi K, van Zandvoort LJC, Balbi MM, et al. Validation of a three-dimensional quantitative coronary angiography-based software to calculate fractional flow reserve:The FAST study. EuroIntervention. 2021;16:591-599.
22. Ai H, Zheng N, Li L, et al. Agreement of Angiography-Derived and Wire-Based Fractional Flow Reserves in Percutaneous Coronary Intervention. Front Cardiovasc Med. 2021;8:654392.
23. Smit JM, El Mahdiui M, van Rosendael AR, et al. Comparison of Diagnostic Performance of Quantitative Flow Ratio in Patients With Versus Without Diabetes Mellitus. Am J Cardiol. 2019;123:1722-1728.
24. Zuo W, Sun R, Xu Y, et al. Impact of calcification on Murray law-based quantitative flow ratio for physiological assessment of intermediate coronary stenoses. Cardiol J. 2024;31:205-214.
25. Emori H, Kubo T, Kameyama T, et al. Diagnostic accuracy of quantitative flow ratio for assessing myocardial ischemia in prior myocardial infarction. Circ J. 2018;82:807-814.
26. Deeks JJ. Systematic reviews of evaluations of diagnostic and screening tests. Bmj. 2001;323:157.
27. Walter SD. Properties of the summary receiver operating characteristic (SROC) curve for diagnostic test data. Stat Med. 2002;21:1237-1256.
28. Whiting PF, Reitsma JB, Leeflang MMG, et al. QUADAS-2:a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529-536.
29. Westra J, Tu S, Winther S, et al. Evaluation of Coronary Artery Stenosis by Quantitative Flow Ratio during Invasive Coronary Angiography:The WIFI II Study (Wire-Free Functional Imaging II). Circ Cardiovasc Imaging. 2018;11:1-8.
30. Yazaki K, Otsuka M, Kataoka S, et al. Applicability of 3-dimensional quantitative coronary angiography-derived computed fractional flow reserve for intermediate coronary stenosis. Circ J. 2017;81:988-992.
31. Echavarría-Pinto M, Van de Hoef TP, Pacheco-Beltran N, et al. Diagnostic agreement of quantitative flow ratio with fractional flow reserve in a Latin-American population. Int J Cardiovasc Imaging. 2022;38:1423-1430.
32. Hrakesh O, Hay M, Lim RY, et al. Comparison of diagnostic performance between quantitative flow ratio, non-hyperemic pressure indices and fractional flow reserve. Cardiovasc Diagn Ther. 2020;10:442-452.
33. Yuasa S, Lauri FM, Mejia-Renteria H, et al. Angiography-derived functional assessment of left main coronary stenoses. Catheter Cardiovasc Interv. 2023;101:1045-1052.
34. Stähli BE, Erbay A, Steiner J, et al. Comparison of resting distal to aortic coronary pressure with angiography-based quantitative flow ratio. Int J Cardiol. 2019;279:12-17.
35. Omori H, Witberg G, Kawase Y, et al. Angiogram based fractional flow reserve in patients with dual/triple vessel coronary artery disease. Int J Cardiol. 2019;283:17-22.
36. Fearon WF, Achenbach S, Engstrom T, et al. Accuracy of Fractional Flow Reserve Derived from Coronary Angiography. Circulation. 2019;139:477-484.
37. Kornowski R, Lavi I, Pellicano M, et al. Fractional Flow Reserve Derived From Routine Coronary Angiograms. J Am Coll Cardiol. 2016;68:2235-2237.
38. Tröbs M, Achenbach S, Röther J, et al. Comparison of Fractional Flow Reserve Based on Computational Fluid Dynamics Modeling Using Coronary Angiographic Vessel Morphology Versus Invasively Measured Fractional Flow Reserve. Am J Cardiol. 2016;117:29-35.
39. Morris PD, Ryan D, Morton AC, et al. Virtual fractional flow reserve from coronary angiography:Modeling the significance of coronary lesions. Results from the VIRTU-1 (VIRTUal fractional flow reserve from coronary angiography) study. JACC Cardiovasc Interv. 2013;6:149-157.
40. Neleman T, Masdjedi K, Van Zandvoort LJC, et al. Extended Validation of Novel 3D Quantitative Coronary Angiography-Based Software to Calculate vFFR:The FAST EXTEND Study. JACC Cardiovasc Imaging. 2021;14:504-506.
41. Papafaklis MI, Muramatsu T, Ishibashi Y, et al. Fast virtual functional assessment of intermediate coronary lesions using routine angiographic data and blood flow simulation in humans:Comparison with pressure wire - fractional flow reserve. EuroIntervention. 2014;10:574-583.
42. Omori H, Kawase Y, Mizukami T, et al. Diagnostic Accuracy of Artificial Intelligence-Based Angiography-Derived Fractional Flow Reserve Using Pressure Wire-Based Fractional Flow Reserve as a Reference. Circ J. 2023;87:783-790.
43. Scoccia A, Tomaniak M, Neleman T, Groenland FTW, Plantes ACZ des, Daemen J. Angiography-Based Fractional Flow Reserve:State of the Art. Curr Cardiol Rep. 2022;24:667-678.
44. Cortés C, Carrasco-Moraleja M, Aparisi A, et al. Quantitative flow ratio—Meta-analysis and systematic review. Catheter Cardiovasc Interv. 2021;97:807-814.
45. Faria D, Hennessey B, Shabbir A, et al. Functional coronary angiography for the assessment of the epicardial vessels and the microcirculation. EuroIntervention. 2023;19:203-221.
46. Leone AM, Campo G, Gallo F, et al. Adenosine-Free Indexes vs. Fractional Flow Reserve for Functional Assessment of Coronary Stenoses:Systematic Review and Meta-Analysis. Int J Cardiol. 2020;299:93-99.
47. Ninomiya K, Serruys PW, Kotoku N, et al. Anonymous Comparison of Various Angiography-Derived Fractional Flow Reserve Software With Pressure-Derived Physiological Assessment. JACC Cardiovasc Interv. 2023;16:1778-1790.
Special articles
Original articles
Editorials
Original articles
Editorials
Post-TAVI management of frail patients: outcomes beyond implantation
Unidad de Hemodinámica y Cardiología Intervencionista, Servicio de Cardiología, Hospital General Universitario de Elche, Elche, Alicante, Spain
Original articles
Debate
Debate: Does the distal radial approach offer added value over the conventional radial approach?
Yes, it does
Servicio de Cardiología, Hospital Universitario Sant Joan d’Alacant, Alicante, Spain
No, it does not
Unidad de Cardiología Intervencionista, Servicio de Cardiología, Hospital Universitario Galdakao, Galdakao, Vizcaya, España














