The use of drug-eluting stents (DES) for the treatment of coronary artery stenosis substantially reduced the need for repeat revascularization compared to bare-metal stents.1 However, as many patients undergoing stenting have long life expectancy, and the incidence rate of stent failure increases with time since implantation, the number of patients presenting with DES restenosis is not insignificant and the treatment of these patients remains a challenge.2
Current clinical practice guidelines recommend treatment of restenosis associated with angina or ischemia by repeat revascularization with either repeat stenting with DES or angioplasty with drug coated balloon (DCB).3 Certain situations favour repeat stenting with DES, most notably loss of mechanical integrity of the restenosed stent. In general, however, although repeat stenting with DES may be more effective than angioplasty with DCB in the short-to-medium-term,4 avoidance of additional stent layers is an important consideration in the longer-term. Indeed, many centres prefer DCB angioplasty as a first-line approach for the treatment of restenosis in the absence of a compelling indication for repeat stenting.
The efficacy of DCB treatment relies on rapid transfer and subsequent tissue retention of the anti-proliferative agent, which is necessary for a persistent suppression of cell proliferation.5 Preclinical data suggest that micro-injuries to the vessel wall may enhance the ability of DCBs to inhibit neointimal growth.6 These micro-injuries can be achieved with a number of different types of modified balloon catheters, such as cutting or scoring balloons. Cutting balloon angioplasty is an attractive option thanks to its ability to effectively incise neointimal tissue and its ease of use.7 Scoring balloons are based on the same principle and may offer superior flexibility and deliverability at the expense of a somehow lower plaque disruption.
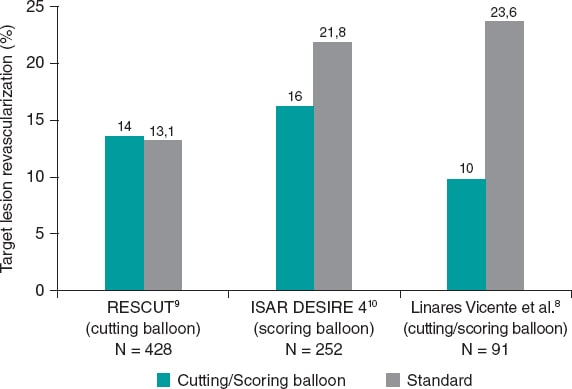
In a recent paper published in REC: Interventional Cardiology, Linares Vicente et al. reported on the 5-year results of cutting or scoring balloon angioplasty combined with DCB to treat in-stent restenosis.8 A total of 51 lesions (42 patients) were treated with cutting balloons plus DCBs, and 56 lesions (49 patients) with a standard DCB angioplasty. Both the SeQuent Please (B. Braun Melsungen AG, Germany), and the Pantera Lux (Biotronik, Switzerland) balloons were used. The primary endpoint was clinically driven target lesion revascularization at 5 years. It appears that, compared to the standard DCB strategy, the use of cutting or scoring balloons considerably reduced the 5-year rate of target lesion revascularization, although this difference was not statistically significant (9.8% vs 23.6%; odds ratio = 0.36; 95% confidence interval, 0.19-1.09; P = .05) (figure 1).
Figure 1. Target lesion revascularization (%): studies comparing cutting balloon/scoring balloon vs standard therapy in patients treated with percutaneous intervention for in-stent restenosis.
The study was retrospective and conducted at a single center with a small sample size of 91 patients. However, it is representative of real-world evidence, which may reflect clinical experiences across a broader and more diverse population of patients than those enrolled in randomized controlled trials. Regarding the baseline characteristics, almost 85% of patients were men with a mean age of 68.3 years. Patients had a high prevalence of diabetes mellitus and smoking (36% and 59%, respectively).
Interestingly, despite the current recommendations of the European Society of Cardiology,3 the use of intravascular ultrasound or optical coherence tomography was relatively low (5.9% in the cutting balloon group, and 8.9% in the standard group). Although this is consistent with rates observed in surveys of use in the clinical practice,11 it represents a missed opportunity for the mechanistic understanding of the disease etiology, and guidance for treatment optimization.12
The primary endpoint was the need for clinically driven target lesion revascularization at 5 years, which was 64% lower with cutting or scoring balloon angioplasty. Given the small sample size of this study and the relatively large treatment effect, it is a pity that insights from the angiographic follow-up were not available. Concordant data from systematic surveillance angiography would have given more confidence to the robustness of the observed treatment effect.
The results of this study should be interpreted in the context of earlier randomized controlled trials with cutting or scoring balloon angioplasty. In fact, evidence from such trials is scant including the RESCUT (Restenosis cutting balloon evaluation trial) trial9 published in 2003, and the more recent ISAR DESIRE 4 (Intracoronary stenting and angiographic results: optimizing treatment of drug-eluting stent in-stent restenosis 4) trial.10
In RESCUT, Albiero et al. randomized 428 patients with bare-metal stent in-stent restenosis across 23 European centers to receive either cutting balloon angioplasty or conventional balloon angioplasty.9 Overall, the trial showed neutral results: at late follow-up, the angiographic restenosis rate, minimal lumen diameter, and the rate of clinical events were similar in both arms (figure 1). Cutting balloon angioplasty, however, was associated with some important procedural advantages, such as use of fewer balloons, less requirement for additional stenting, and a significantly lower incidence of balloon slippage (6.5% vs 25%).
ISAR DESIRE 4 was a randomized, open-label, assessor-blinded trial that enrolled 252 patients with clinically significant DES restenosis undergoing DCB angioplasty at 4 different centres in Germany.10 This trial investigated scoring balloon rather than cutting balloon angioplasty. The primary endpoint–diameter stenosis at the 6-8-month follow-up angiography–was lower for the scoring balloon compared to the regular balloon angioplasty: 35% vs 40.4%; P = .047; in addition, target lesion revascularization was numerically lower (figure 1). Although, the size of treatment effect was modest, small incremental gains in efficacy in this challenging patient subset may translate into important clinical benefits.
Against this background, the observations made by Linares Vicente et al.8 are an important addition to the evidence supporting the clinical use of cutting or scoring balloons to treat stent failure. While repeat stenting with DES or angioplasty with DCB are the mainstay of in-stent restenosis procedures, the procedural efficiency and clinical efficacy of both approaches will likely improve with the adjunctive use of cutting or scoring balloons. The benefits of these devices are most likely mediated by a combination of factors: reduced balloon slippage (or watermelon-seeding), the mechanical advantage of increased disruption of restenotic tissue, and the potential for enhanced efficacy of the device-delivered drug. The management of patients with stent failure remains challenging and deserves the best treatment the operator can offer including the liberal use of cutting or scoring balloon lesion preparation. In this clinical setting, small margins can make a big difference.
FUNDING
L. McGovern is funded by the European Commission under the Horizons 2020 framework (grant agreement number 965246 CORE-MD).
CONFLICTS OF INTEREST
R.A. Byrne declared research or educational funding in the institution he currently works at from Abbott Vascular, Biosensors, Biotronik, and Boston Scientific. L. McGovern declared no conflicts of interest whatsoever.
REFERENCES
1. Cassese S, Byrne RA, Tada T, et al. Incidence and predictors of restenosis after coronary stenting in 10 004 patients with surveillance angiography. Heart. 2014;100:153-159.
2. Cutlip DE, Chhabra AG, Baim DS, et al. Beyond Restenosis. Circulation. 2004;110:1226-1230.
3. Neumann F-J, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2018;40:87-165.
4. Giacoppo D, Alfonso F, Xu B, et al. Paclitaxel-coated balloon angioplasty vs. drug-eluting stenting for the treatment of coronary in-stent restenosis:a comprehensive, collaborative, individual patient data meta-analysis of 10 randomized clinical trials (DAEDALUS study). Eur Heart J. 2020;41:3715-3728.
5. Byrne RA, Joner M, Alfonso F, Kastrati A. Drug-coated balloon therapy in coronary and peripheral artery disease. Nat Rev Cardiol. 2014;11:13-23.
6. Radke PW, Joner M, Joost A, et al. Vascular effects of paclitaxel following drug-eluting balloon angioplasty in a porcine coronary model:the importance of excipients. EuroIntervention. 2011;7:730-737.
7. Barath P, Fishbein MC, Vari S, Forrester JS. Cutting balloon:A novel approach to percutaneous angioplasty. Am J Cardiol. 1991;68:1249-1252.
8. Linares Vicente JA, Ruiz Arroyo JR, Lukic A, et al. 5-year results of cutting or scoring balloon before drug-eluting balloon to treat in-stent restenosis. REC Interv Cardiol. 2022;4:6-11.
9. Albiero R, Silber S, Di Mario C, et al. Cutting balloon versus conventional balloon angioplasty for the treatment of in-stent restenosis:Results of the restenosis cutting balloon evaluation trial (RESCUT). J Am Coll Cardiol. 2004;43:943-949.
10. Kufner S, Joner M, Schneider S, et al. Neointimal Modification With Scoring Balloon and Efficacy of Drug-Coated Balloon Therapy in Patients With Restenosis in Drug-Eluting Coronary Stents:A Randomized Controlled Trial. JACC Cardiovasc Interv. 2017;10:1332-1340.
11. Koskinas KC, Nakamura M, Raber L, et al. Current use of intracoronary imaging in interventional practice - Results of a European Association of Percutaneous Cardiovascular Interventions (EAPCI) and Japanese Association of Cardiovascular Interventions and Therapeutics (CVIT) Clinical Practice Survey. EuroIntervention. 2018;14:e475-e484.
12. Alfonso F, Sandoval J, Cárdenas A, Medina M, Cuevas C, Gonzalo N. Optical coherence tomography:from research to clinical application. Minerva Med. 2012;103:441-464.