ABSTRACT
Introduction and objectives: There is scarce information available on the long-term outcomes of primary angioplasty (PA) in patients over 80 years of age. Our objective was to analyze the characteristics and results of PA in these patients and recognize the prognostic factors and long-term survival.
Methods: Observational and retrospective single-center study of consecutive patients over 80 years of age treated with PA between January 2013 and September 2019. A long-term clinical follow-up was performed (mean follow-up of 29 ± 25 months).
Results: The study included 133 patients (mean age 85.3 ± 3.8 years and 57 women [43%]). Seventeen percent of the patients were in Killip class III-IV at admission. The mean Charlson Comorbidity index was 2.3 ± 1.6. During the hospitalization, almost half of the patients developed heart failure and mortality rate was 18%. The overall mortality rate at the follow-up was 23%, yet 97.2% of the deaths were due to non-cardiac causes. The independent predictors of overall mortality at the follow-up were chronic kidney disease (HR, 5.7; 95%CI, 1.29-25.5; P = .022), and a Charlson Comorbidity index > 2 (HR, 2.57; 95%CI, 1.07-6.18; P = .035).
Conclusions: Patients over 80 years of age treated with PA have high in-hospital and long-term mortality rates. Comorbidities and chronic kidney disease were the only independent predictors of long-term mortality.
Keywords: Elderly. Myocardial infarction. Primary angioplasty.
RESUMEN
Introducción y objetivos: Existe poca información sobre los resultados a largo plazo de la angioplastia primaria (AP) en pacientes mayores de 80 años. Nuestro objetivo fue analizar las características y los resultados de la AP en estos pacientes, y valorar los predictores pronósticos y la supervivencia a largo plazo.
Métodos: Estudio observacional, retrospectivo y unicéntrico de pacientes mayores de 80 años consecutivos sometidos a AP entre enero de 2013 y septiembre de 2019. Se efectuó un seguimiento clínico a largo plazo (media de 29 ± 25 meses).
Resultados: Se incluyeron 133 pacientes (57 [43%] mujeres) con una edad media de 85,3 ± 3,8 años. El 17% se encontraban en clase Killip III o IV. El índice de Charlson medio fue de 2,3 ± 1,6. En cuanto a la evolución hospitalaria, casi la mitad de los pacientes desarrollaron insuficiencia cardiaca y un 18% fallecieron durante el ingreso. La mortalidad total en el seguimiento a largo plazo fue del 23%, siendo el 97,2% de las muertes de causa no cardiaca. Los predictores independientes de mortalidad total en el seguimiento a largo plazo fueron la enfermedad renal crónica (hazard ratio [HR] = 5,7; intervalo de confianza del 95% [IC95%], 1,29-25,5; p = 0,022) y el índice de Charlson mayor de 2 (HR = 2,57; IC95%, 1,07-6,18; p = 0,035).
Conclusiones: Los pacientes mayores de 80 años sometidos a AP tienen una elevada mortalidad hospitalaria y en el seguimiento a largo plazo. La comorbilidad y la enfermedad renal crónica resultaron ser los únicos predictores independientes de mortalidad a largo plazo.
Palabras clave: Anciano. Infarto de miocardio. Angioplastia primaria.
Abbreviations
PA: primary angioplasty.
INTRODUCTION
The current estimates reveal the population gradual aging, which will be more evident in the coming years.1 Based on these estimates, by the year 2050, our country will become one of the oldest worldwide with more than 4 million people over 80 years of age. This means that the percentage of patients treated with primary angioplasty (PA) is on the rise in our setting.
Although old age is associated with worse prognoses, PA is still the best reperfusion strategy for these patients.2-5 This segment of the population has a high prevalence of comorbidities, is often recommended fewer treatments, and has a higher risk of complications during revascularization procedures. Also, these patients are often misrepresented in the clinical trials, meaning that there is little scientific evidence available on the clinical characteristics, results, and long-term prognosis after PA.6
The objectives of this study were to analyze the characteristics, results, mortality, and prognostic predictors of patients > 80 treated with PA in our center.
METHODS
Single-center, retrospective, and observational study. All patients > 80 treated with PA in our center from January 2013 through September 2019 were included. Different clinical and epidemiological variables like age, sex, cardiovascular risk factors, presence of comorbidities, and the total ischemic time were prospectively registered in the unit database. The Charlson Comorbidity was retrospectively obtained at admission to stratify the patients’ overall comorbidities.7,8 This study was approved by Hospital Universitario Fundación Alcorcón ethics committee and waiver of informed consent was accepted.
Catheterization and treatment
Most cases were treated with percutaneous coronary intervention using the standard technique via radial access. The contrast agents used in all the cases were iohexol (Omnipaque 350, and Omnipaque 300), and iodixanol (Visipaque 320). The number of main vessels damaged seen on the coronary angiography, the access route, the dose of contrast used, the x-ray image time, and the number and type of stent use were recorded. Angiographic success and the presence of complications during the procedure were recorded as well. The operator chose the type of stent he would use during the procedure, although the local protocol recommended the use of conventional stents preferably. Drug-eluting stents were spared for situations of high risk of restenosis.
Follow-up and endpoints
Follow-up data were obtained after reviewing our hospital electronic health records. Also, phone calls to the patient or his family were made followed by a standard survey when appropriate. The endpoints studied were in-hospital mortality and complications, cardiovascular events, and cardiac death at the long-term follow-up.
Definitions
Left ventricular systolic function was estimated on the echocardiogram. The presence of a left ventricular ejection fraction < 45% was considered moderate-to-severe left ventricular dysfunction. Cardiogenic shock was defined as systolic arterial pressure < 90 mmHg for, at least, 1 hour followed by tissue hypoperfusion that required inotropic support and/or intra-aortic balloon pump implantation. Cardiac deaths were due to acute coronary syndrome, heart failure or ventricular arrhythmia. Angiographic success was defined as the presence of TIMI grade ≥ 2 flow in the absence of residual stenosis > 50%. The glomerular filtration rate was estimated using the simplified modification of diet in renal disease (MDRD) equation.9 Chronic kidney disease was defined as a glomerular filtration rate < 60 mL/min/ 1.73 m2 at admission. Bleeding complications associated with vascular access were classified based on the Bleeding Academic Research Consortium (BARC) definitions.10 BARC type > 2 hemorrhages were considered major bleeding. Target lesion revascularization was defined as the need for a new revascularization procedure (whether percutaneous or surgical) of the coronary segment with stenting in the presence of angiographic restenosis (stenosis > 50%) and symptoms or signs of myocardial ischemia.
Statistical analysis
The statistical software package SPSS version 20 was used for the analysis of data. Quantitative variables were expressed as mean ± standard deviation. The categorical ones were expressed as absolute value and percentage.
Univariate and multivariate modified Poisson regression analyses were conducted to determine the independent prognostic factors of in-hospital mortality. The variables included in the multivariate analyses were those considered of the greatest clinical relevance: Killip Class > I at admission, age > 85, chronic kidney disease, Charlson Comorbidity index > 2, and presence of moderate-to-severe left ventricular dysfunction. Results were expressed as relative risks and their 95% confidence interval (95%CI).
Univariate and multivariate Cox regression analyses were conducted to determine the independent predictors of overall mortality at the long-term follow-up. The variables included in the multivariate analyses were those associated with a higher mortality rate in the univariate analysis and also those of the greatest clinical relevance: Killip Class > I at admission, age > 85, chronic kidney disease, Charlson Comorbidity index > 2, and presence of moderate-to-severe left ventricular dysfunction. Results were expressed as hazard ratios (HR) and their 95%CI. P values < .05 were considered statistically significant. The inter-group overall mortality-free survival rates based on the presence of chronic kidney disease and a Charlson comorbidity index > 2 were compared using the Kaplan-Meier Curves (log-rank test).
RESULTS
Clinical characteristics and of the interventional procedure
A total of 1269 PAs were performed in our center from January 2013 through September 2019. A total of 10.5% were ≥ 80 years old at admission. The study group included 133 patients (57 women [43%]) with a median age of 85.3 ± 3.8 years treated with PA. The study population had a high prevalence of cardiovascular risk factors. A total of 66.2% of the patients had chronic kidney disease. The anterior was the most common location of the infarction. A total of 16.6% of the patients were Killip Class III-IV. In 28.5% of the cases delays of more than 6 hours between the beginning of pain and reperfusion were reported. The mean Charlson Comorbidity index used to assess the comorbidities of the patients included in our series was 2.3 ± 1.6 (table 1).
Table 1. Clinical angiographic, and interventional procedure data
| Patients | N = 133 |
|---|---|
| Age (years) | 85.3 ± 3.8 |
| Sex (woman) | 57 (43%) |
| Diabetes mellitus | 46 (34.6%) |
| Dyslipidemia | 77 (57.9%) |
| Arterial hypertension | 110 (82.7%) |
| Active smoking | 4 (3%) |
| Charlson Comorbidity index | 2.3 ± 1.6 |
| Body mass index | 26.4 ± 3.3 |
| Previous infarction | 23 (17.3%) |
| Previous angioplasty | 18 (13.5%) |
| Previous coronary artery bypass surgery | 3 (2.3%) |
| Atrial fibrillation | 31 (23.3%) |
| LVEF echocardiogram | 47.1 ± 11 |
| LVEF < 50% | 61 (45.8%) |
| Creatinine levels at admission (mg/dL) | 1.25 ± 0.44 |
| GFR-MDRD (mL/min/1.73 m2) | 52.2 ± 18.5 |
| Chronic kidney disease* | 88 (66.2%) |
| Location of the infarction | |
| Anterior | 62 (46.6%) |
| Inferior | 48 (36.1%) |
| Lateral | 11 (8.3%) |
| Undetermined | 9 (6.8%) |
| Cardiac arrest | 3 (2.3%) |
| Killip Class | |
| I | 100 (75.1%) |
| II | 11 (8.3) |
| III | 7 (5.3) |
| IV | 15 (11.3) |
| Total ischemic time > 6h | 37 (28.5%) |
| Median of total ischemic time (min) | 268 [177-406] |
| Median of time from symptom onset until arrival at the PA-capable left (min) | 203 [124-330] |
| Median of time from the arrival at the PA-capable leftuntil guidewire passage (min) | 50 [37-77] |
| X-ray image time (min) | 16.6 ± 13 |
| Volume of contrast (mL) | 173 ± 72 |
| Radial access | 107 (80.5%) |
| Number of diseased vessels | |
| 1 | 70 (52.6%) |
| 2 | 39 (29.3%) |
| 3 | 24 (18%) |
| Number of stents implanted | 1.04 ± 0.2 |
| Thrombus aspiration | 34 (25.6%) |
| Glycoprotein IIb/IIIa inhibitors | 17 (12.8%) |
| Drug-eluting stent | 41 (30.8%) |
| PCI of NC lesions in the acute phase | 4 (3%) |
| PCI of NC lesions in another procedure at admission | 11 (8.3%) |
| Complete revascularization | 69 (51.9%) |
| Angiographic success | 127 (95.5%) |
| In-hospital mortality | 24 (18%) |
|
GFR-MDRD, glomerular filtration rate (Modification of Diet in Renal Disease); LVEF, left ventricular ejection fraction; NC, non-culprit; PA, primary angioplasty; PCI, percutaneous coronary intervention. Data are expressed as no. (%), mean ± standard deviation or median [interquartile range]. * Defined as a glomerular filtration rate < 60 mL/min/1.73 m2. |
|
Regarding the angiographic and procedural data, the radial access was used in 80.5% of the patients of whom 47.4% had multivessel disease. Almost half of the patients were released from the hospital with incomplete angiographic revascularizations. Thrombus aspiration was performed in one fourth of the patients and drug-eluting stents were implanted in 30.8% of these patients (table 1).
Patient progression at the hospital setting
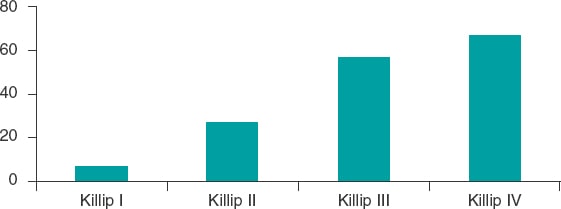
Regarding patient progression at the hospital setting, 63 patients (49%) developed heart failure and 24 patients (18%) died during admission. Two patients (1.5%) had stent thrombosis during their hospital stay. The cause of death of 21 of the dead patients (87.5%) was cardiovascular. There was a statistically significant higher in-hospital mortality rate in patients with Charlson comorbidity indices > 2 (28.9% vs 13.7%, P = .039), Killip Class > I (51.5% vs 7%; P < .001), and worse ventricular (26% vs 4.3%, P = .003) and renal functions (23.9% vs 6.7%; P = .031). The Killip Class-based mortality rate based was 7% for Killip Class I, 27.3% for Killip Class II, 57.1% for Killip Class III, and 66.7% for Killip Class IV (figure 1).
Figure 1. In-hospital mortality based on Killip Class.
In the multivariate modified Poisson regression analysis, the only independent prognostic factor of in-hospital mortality was the Killip Class at admission (relative risk, 6.5; 95%CI, 2.01-20.36; P = .001) (table 2).
Table 2. Factors associated with a higher in-hospital mortality rate. Univariate and multivariate modified Poisson regression analyses
| RR | 95%CI | P | |
|---|---|---|---|
| Univariate analysis | |||
| Age | 1.06 | 0.8-1.15 | .135 |
| Sex (woman) | 1.58 | 0.76-3.27 | .221 |
| Diabetes Mellitus | 1.35 | 0.65-2.81 | .42 |
| Killip Class > I | 7.36 | 3.34-16.22 | < .001 |
| Moderate-to-severe left ventricular dysfunction | 6.07 | 1.81-20.28 | .003 |
| Total ischemic time (hours) | 1.05 | 0.98-1.22 | .163 |
| Atrial fibrillation | 1.65 | 0.78-3.48 | .193 |
| Charlson Comorbidity index > 2 | 2.12 | 1.04-4.31 | .039 |
| Chronic kidney disease | 3.58 | 1.12-11.41 | .031 |
| Anterior location | 1.60 | 0.77-3.36 | .211 |
| Multivessel disease | 1.49 | 0.70-3.17 | .297 |
| Incomplete revascularization | 1.38 | 0.67-2.86 | .383 |
| Drug-eluting stent | 1.1 | 0.43-2.82 | .846 |
| Mulivariate analysis | |||
| Age | 1.1 | 0.99-1.21 | .074 |
| Killip Class > I | 6.5 | 2.01-20.36 | .001 |
| Chronic kidney disease | 1.23 | 0.26-5.96 | .793 |
| Charlson Comorbidity index > 2 | 2.2 | 0.9-5.38 | .083 |
| Moderate-to-severe left ventricular dysfunction | 3.05 | 0.95-9.81 | .062 |
|
95%CI, 95% confidence interval; RR, relative risk.Statistically significant results are highlighted in bold. |
|||
Long-term follow-up
A long-term follow-up was conducted of the 109 survivors. The median clinical follow-up was 24.3 months (interquartile range, 6.9-49.4 months) with 3 patients (2.8%) lost to follow-up. The clinical events occurred at the follow-up are shown on table 3. The overall mortality rate at the long-term follow-up was 23% with 97.2% of deaths due to noncardiac deaths.
Table 3. Events at the long-term follow-up
| Patients | N = 106 |
|---|---|
| New acute coronary syndrome | 10 (9.2%) |
| Target lesion revascularization | 4 (3.7%) |
| Stent thrombosis | 3 (2.8%) |
| BARC bleeding type > 2 | 19 (17.4%) |
| Stroke | 9 (8.3%) |
| Overall mortality | 25 (22.9%) |
| Cardiovascular mortality | 3 (2.8%) |
| Infection | 6 (5.5) |
| Neoplasm | 6 (5.5) |
| Respiratory failure | 5 (4.6) |
| Unknown | 5 (4.6) |
|
BARC, Bleeding Academic Research Consortium. |
|
In the univariate Cox regression analysis, the variables associated with a higher overall mortality rate were Killip Class > I (HR, 4.26; 95%CI, 2.38-7.62; P = .001), chronic kidney disease (HR, 7.24; 95%CI, 1.7-30.8; P = .007), and a Charlson Comorbidity index > 2 (HR, 2.74; 95%CI, 1.18-6.36; P = .019) (table 4). Patients with chronic kidney disease had a higher percentage of cases with Charlson Comorbidity indices > 2, but this difference was not statistically significant (19% vs 28,4%; P = .27).
Table 4. Factors associated with a higher mortality rate at the long-term follow-up. Univariate and multivariate Cox regression analyses
| HR | 95%CI | P | |
|---|---|---|---|
| Univariate analysis | |||
| Age | 1.1 | 0.99-1.23 | .076 |
| Sex (woman) | 1.66 | 0.71-3.91 | .244 |
| Diabetes Mellitus | 1.98 | 0.89-4.41 | .094 |
| Killip Class > I | 4.26 | 2.38-7.62 | .001 |
| Moderate-to-severe left ventricular dysfunction | 2.16 | 0.97-4.84 | .06 |
| Total ischemic time (hours) | 1.05 | 0.98-1.12 | .159 |
| Atrial fibrillation | 1.54 | 0.61-3.9 | .361 |
| Charlson Comorbidity index > 2 | 2.74 | 1.18-6.36 | .019 |
| Chronic kidney disease | 7.24 | 1.7-30.81 | .007 |
| Anterior location | 1.36 | 0.77-2.40 | .287 |
| Multivessel disease | 1.43 | 0.81-2.53 | .214 |
| Incomplete revascularization | 1.590 | 0.898-2.817 | .112 |
| Drug-eluting stent | 0.949 | 0.46-1.957 | .887 |
| Multivariate analysis | |||
| Age | 1.07 | 0.95-1.21 | .258 |
| Charlson Comorbidity index > 2 | 2.57 | 1.07-6.18 | .035 |
| Chronic kidney disease | 5.7 | 1.29-25.5 | .022 |
| Killip Class > I | 0.96 | 0.31-2.98 | .943 |
| Moderate-to-severe left ventricular dysfunction | 1.77 | 0.77-4.04 | .177 |
|
95%CI, 95% confidence interval; HR, hazard ratio. Statistically significant results are highlighted in bold. |
|||
In the multivariate Cox regression analysis, the only independent predictors of overall mortality were chronic kidney disease (HR, 5.7; 95%CI, 1.29-25.5; P = .022), and a Charlson Comorbidity index > 2 (HR, 2.57; 95%CI, 1.07-6.18; P = .035) (table 4).
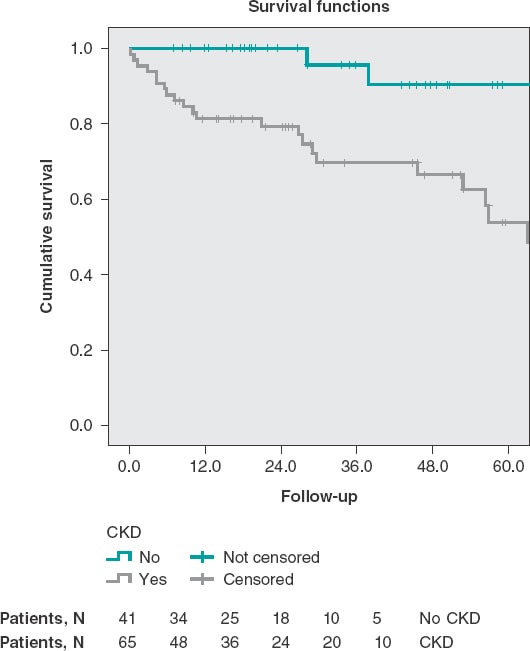
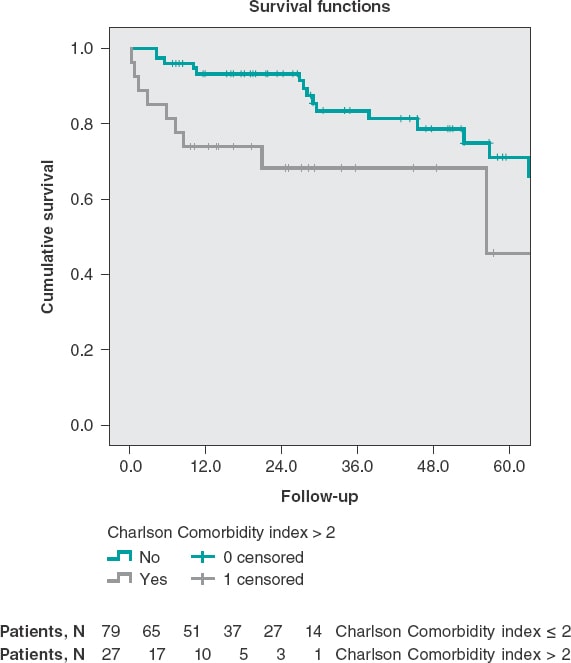
Patients with chronic kidney disease had lower survival rates at the long-term follow-up (56 ± 4.4 months vs 75 ± 3 months; P = .002) (figure 2). Patients with Charlson comorbidity indices > 2 also had lower survival rates at the long-term follow-up (45.5 ± 5.9 months vs 65.8 ± 3.3 months; P = .015) (figure 3).
Figure 2. Survival curves at the long-term follow-up stratified based on the presence of chronic kidney disease (log rank test, P = .002). ERC, chronic kidney disease.
Figure 3. Survival curves at the long-term follow-up stratified based on the presence of Charlson comorbidity indices > 2 (log rank test, P = .015).
DISCUSSION
Information on the results of PA in elderly patients and its long-term prognosis is scarce because this group of patients is often misrepresented in clinical trials.6 Our study emphasizes these patients’ high mortality rate (mainly due to cardiac causes)—both in-hospital and at the long-term follow-up—with a significant contribution from noncardiac mortality and comorbidities as prognostic predictors.
This segment of the population has special characteristics that pose an added risk. These are patients with a high prevalence of comorbidities and worse renal function.5 Diagnosis is not always easy because of the atypical symptoms reported and possible presence of previous changes on the EKG, factors that contribute to delaying reperfusion therapy.11 Finally, these are patients with a higher risk of bleeding and other complications during PA.12
Regarding the clinical profile of patients > 80 treated with PA in our center we should mention the higher percentage of women (43%) compared to other series from the general population, and the high prevalence of chronic kidney disease (66%), delays of more than 6 hours (29%), and advanced Killip Class (17%). All these characteristics are consistent with what has already been described by former studies in this population.5,13
Regarding the procedural aspects, the radial access was used in 80.5% of the cases. Elderly patients, especially women, have higher rates of failure with this access, but at the same time, these patients have the highest risk of bleeding with the femoral access. Rodríguez-Leor et al.14 reported on the possibility of achieving radial access in 95.1% in a population of patients > 75 treated with PA.
The in-hospital mortality seen in our study (18) is obviously higher to that of the general population, but not significantly different from that reported by other registries of elderly patients.12-17 In a group of 34 80-year-old patients treated with PA Sim et al.5 reported an in-hospital mortality rate of 18%. However, it went up to 37% in patients with ST-segment elevation acute coronary syndrome not treated with PA. In their prospective registry of 496 patients > 80 who received invasive treatment, Kvakkestad et al.12 reported an in-hospital mortality rate of 13%. In our series the main prognostic factor during admission was the patient’s hemodynamic situation measured using Killip Class. It is a well-known prognostic factor that has been widely described in PA studies.18
The mortality rate at the long-term follow-up was 23% with a striking contribution from noncardiac mortality, which is a differential factor with respect to series from the general population. This lower rate of adverse cardiovascular events in elderly patients who survive a myocardial infarction was found in other registries and may be due to the high early selection during the acute phase.13,17 In the aforementioned registry of Kvakkestad et al.12 the mortality rate at the 3-year follow-up was 29%. In the Swedish registry of 80-year-old patients treated with PA from 2001 to 2010, the annual mortality rate reported was 25%.17 In our series, the fact that mortality at the long-term follow-up was mostly noncardiac contributed to the fact that the main prognostic predictors at the long-term follow-up are extracardiac factors like renal function and the Charlson Comorbidity index. These factors may be understudied at the follow-up after PA.
The effect of comorbidities in the prognosis of patients is often quantified using the Charlson Comorbidity index.7,8 This index assigns a given score to a series of comorbidities based on the risk of mortality of every comorbidity. The overall score is associated with a given mortality risk. Over the last few years, interest has been growing on the analysis of comorbidities and other variables associated with age. However, data are still scarce on their prognostic influence on patients with infarction treated invasively. The existing growing heterogeneity among 80-year-old patients with infarction requires prognostic indices to stratify these patients into risk groups based on uniform criteria. Using a tool to guide us in the long-term prognosis of these patients may help us decide what the most suitable follow-up is. Several studies have proven the utility of the Charlson Comorbidity index in the acute coronary syndrome as a predictor of mortality. Núñez et al. determined the prognostic predictive value of this index in patients with myocardial infarction mostly treated conservatively.19 They found that the comorbidities present at admission were associated with higher rates of mortality or reinfarction at the 30-day and 1-year follow-up. In our series of invasive management, we found that a Charlson Comorbidity index > 2 was an independent predictor of mortality at the long-term follow-up. However, it is not a predictor of patient progression at the hospital setting where the most important thing is the patient’s hemodynamic situation. Therefore, in this population the Charlson Comorbidity index can help us plan their long-term follow-up.
Glomerular filtration rate impairment is a powerful predictor of mortality in different conditions including myocardial infarction.20 Same as it happens with the Charlson Comorbidity index, in our series of patients, renal function impairment was also an independent predictor of long-term mortality. This confirms that a more comprehensive assessment of 80-year-old survivors of a PA including an accurate assessment of comorbidities and renal function can optimize the management of this population after hospital discharge.
Risk stratification and decision-making are especially complex in 80-year-old patients with myocardial infarction because these a highly heterogeneous patients in whom chronological age may not reflect their actual biological situation. In view of our study findings we believe that in elderly patients it is important to include the measurement of the glomerular filtration rate and, above all, the assessment of comorbidities in the decision-making process at the long-term follow-up after PA. The close follow-up of these patients with several comorbidities can help diagnose potential decompensations (both cardiac and noncardiac) to prevent new hospitalizations. On the other hand, comorbidities determine a high use of drugs which favors the appearance of adverse events, interactions, and therapeutic compliance mistakes. The best thing to do would be to maximize compliance in this population, specify the benefits expected, and minimize the risks associated with the therapy used. Also, optimizing the management of noncardiac diseases can be the key to stabilize coronary artery disease. For all this, keeping a close collaboration with geriatric units after the hospital discharge of 80-year-old patients treated with PA improves their prognosis.
Limitations and strengths
Although the demographic, clinical, and angiographic data were collected prospectively, this was a retrospective analysis with the corresponding limitations of this type of studies. The size of the sample may have limited the statistical power of our study to detect the statistical significance of some associations. Also, the low number of events may have limited the reliability of the multivariate analysis regarding in-hospital mortality and mortality at the long-term follow-up since it included 5 variables in each of these 2 analyses. Since this was a single-center study, results may not be generalizable to other settings.
One of the strengths of the study is that results are based on a thorough and consecutive registry of patients from our setting who were hospitalized after a PA. Also, that a great deal of clinical, analytical, and angiographic information was obtained during their hospital stay and several evolutionary variables were registered at the very long follow-up.
CONCLUSIONS
Patients over 80 treated with PA have a high in-hospital mortality rate (18% in our series). The only independent predictor of in-hospital mortality was Killip Class. Over the next 2 years, mortality is still very high (23%), but is basically associated with noncardiac problems. The independent predictors of overall mortality at the long-term follow-up were chronic kidney disease and a Charlson Comorbidity index > 2
FUNDING
None.
AUTHORS’ CONTRIBUTIONS
L. Hernando Marrupe and J. Botas Rodríguez had the study idea. L. Hernando Marrupe, J. Botas Rodríguez, C. Marco Quirós, and R. Gayoso Gayo designed the study. L. Hernando Marrupe, C. Marco Quirós, R. Gayoso Gayo, V. Espejo Bares, V. Artiaga de la Barrera, C. Jiménez Martínez, R. Del Castillo Medina, and A. Núñez García collaborated in the study data mining. L. Hernando Marrupe, and E. Pérez Fernández conducted the statistical analysis. L. Hernando Marrupe, C. Marco Quirós, and R. Gayoso Gayo interpreted the results and wrote the manuscript first draft. L. Hernando wrote the manuscript final version, and J. Botas conducted the manuscript critical review.
CONFLICTS OF INTEREST
None reported.
WHAT IS KNOWN ABOUT THE TOPIC?
- Primary angioplasty has been considered the best reperfusion strategy in patients with ST-segment elevation myocardial infarction for years. However, elderly patients have special characteristics that pose an added risk. Also, they are misrepresented in the clinical trials. Risk stratification and the decision-making process are especially complex in 80-year-old patients with myocardial infarction because this is a highly heterogeneous population.
WHAT DOES THE STUDY ADD?
- In 80-year-old patients treated with PA it seems that the main prognostic factor of in-hospital mortality is the patient’s hemodynamic situation at admission. However, if the patient survives the index event his prognosis is more associated with the presence of comorbidities. Our study proved that measuring the glomerular filtration rate and Charlson Comorbidity index can help us treat these patients more effectively at the long-term follow-up.
REFERENCES
1. Christensen K, Doblhammer G, Rau R, et al. Ageing populations:the challenges ahead. Lancet. 2009;374:1196-1208.
2. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Rev Esp Cardiol. 2017;70:1082.
3. Bueno H, Betriu A, Heras M, et al. Primary angioplasty vs. fibrinolysis in very old patients with acute myocardial infarction:TRIANA (TRatamiento del Infarto Agudo de miocardio eN Ancianos) randomized trial and pooled analysis with previous studies. Eur Heart J. 2011;32:51-60.
4. Doizon T, Orion L, Dimet J, et al. ST elevation myocardial infarction (STEMI) in patients aged 85 and over. Invasive management versus exclusive medical treatment:Departmental study. Ann Cardiol Angeiol (Paris). 2015;64:345-351.
5. Sim WL, Mutha V, Ul-Haq MA, et al. Clinical characteristics and outcomes of octogenarians presenting with ST elevation myocardial infarction in the Australian population. World J Cardiol. 2017;9:437-441.
6. Lee PY, Alexander KP, Hammill BG, et al. Representation of elderly persons and women in published randomized trials of acute coronary syndromes. JAMA. 2001;286:708-713.
7. Charlson M, Szatrowski TP, Peterson J, et al. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245-1251.
8. Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies:development and validation. J Chronic Dis. 1987;40:373-383.
9. Levey AS, Bosch JP, Lewis JB, et al. A more accurate method to estimate glomerular filtration rate from serum creatinine:a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130:461-470.
10. Hicks KA, Stockbridge NL, Targum SL, et al. Bleeding Academic Research Consortium consensus report:the Food and Drug Administration perspective. Circulation. 2011;123:2664-2665.
11. Ladwig KH, Fang X, Wolf K, et al. Comparison of delay times between symptom onset of an acute ST-elevation myocardial infarction and hospital arrival in men and women <65 years versus >65 years of age:findings from Multicenter Munich Examination of Delay in Patients Experiencing Acute Myocardial Infarction (MEDEA) study. Am J Cardiol. 2017;120:2128-2134.
12. Kvakkestad KM, Abdelnoor M, Claussen PA, et al. Long-term survival in octogenarians and older patients with ST-elevation myocardial infarction in the era of primary angioplasty:A prospective cohort study. Eur Heart J Acute Cardiovasc Care. 2016;5:243-252.
13. De la Torre Hernández JM, Brugaletta S, Gómez Hospital JA, et al. Primary Angioplasty in Patients Older Than 75 Years. Profile of Patients and Procedures, Outcomes, and Predictors of Prognosis in the ESTROFA IM+75 Registry. Rev Esp Cardiol. 2017;70:81-87.
14. Rodríguez-Leor O, Fernández-Nofrerias E, Carrillo X, et al. Results of primary percutaneous coronary intervention in patients ≥75 years treated by the transradial approach. Am J Cardiol. 2014;113:452-456.
15. DeGeare VS, Grines CL. Primary percutaneous intervention in octogenarians with acute myocardial infarction:the treatment of choice. Am J Med. 2000;108:257-258.
16. Forman DE, Chen AY, Wiviott SD, et al. Comparison of outcomes in patients aged <75, 75 to 84, and ≥85 years with ST-elevation myocardial infarction (from the ACTION Registry-GWTG). Am J Cardiol. 2010;106:1382-1388.
17. Velders MA, James SK, Libungan B, et al. Prognosis of elderly patients with ST-elevation myocardial infarction treated with primary percutaneous coronary intervention in 2001 to 2011:A report from the Swedish Coronary Angiography and Angioplasty Registry (SCAAR) registry. Am Heart J. 2014;167:666-673.
18. DeGeare VS, Boura JA, Grines LL, et al. Predictive value of the Killip classification in patients undergoing primary percutaneous coronary intervention for acute myocardial infarction. Am J Cardiol. 2001;87:1035-1038.
19. Nunez JE, Nunez E, Facila L, et al. Prognostic value of Charlson comorbidity index at 30 days and 1 year after acute myocardial infarction. Rev Esp Cardiol. 2004;57:842-849.
20. Szummer K, Lundman P, Jacobson SH, et al. Relation between renal function, presentation, use of therapies and in-hospital complications in acute coronary syndrome:data from the SWEDEHEART register. J Intern Med. 2010;268:40-49.