ABSTRACT
Introduction and objectives: The presence of comorbidities in elderly patients with non-ST-segment elevation acute coronary syndrome worsens its prognosis. The objective of the study was to analyze the impact of the burden of comorbidities in the decision of using invasive management in these patients.
Methods: A total of 7211 patients > 70 years old from 11 Spanish registries were included. Individual data were analyzed in a common database. We assessed the presence of 6 comorbidities and their association with coronary angiography during admission.
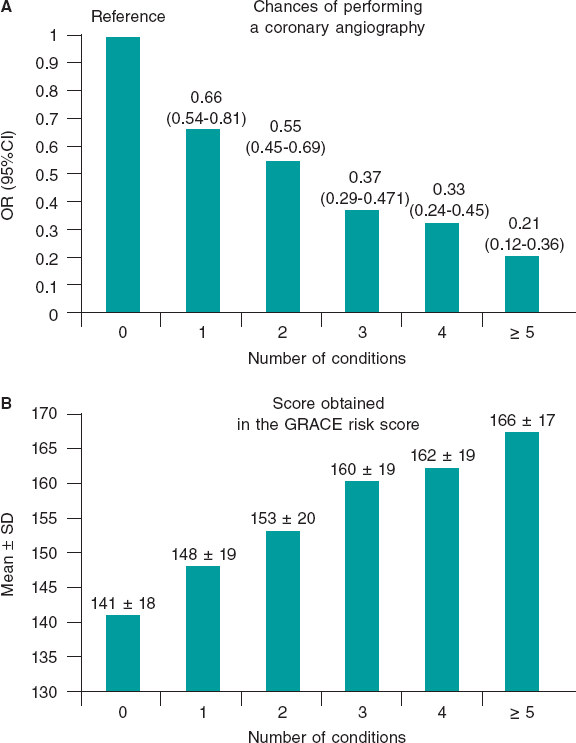
Results: The mean age was 79 ± 6 years and the mean CRACE score was 150 ± 21 points. A total of 1179 patients (16%) were treated conservatively. The presence of each comorbidity was associated with less invasive management (adjusted for predictive clinical variables): cerebrovascular disease (OR, 0.78; 95%CI, 0.64-0.95; P = .01), anemia (OR, 0.64; 95%CI, 0.54-0.76; P < .0001), chronic kidney disease (OR, 0.65; 95%CI, 0.56-0.75; P < .0001), peripheral arterial disease (OR, 0.79; 95%CI, 0.65-0.96; P = .02), chronic lung disease (OR, 0.85; IC95%, 0.71-0.99; P = .05), and diabetes mellitus (OR, 0.85; 95%CI, 0.74-0.98; P < .03). The increase in the number of comorbidities (comorbidity burden) was associated with a reduction in coronary angiographies after adjusting for the GRACE score: 1 comorbidity (OR, 0.66; 95%CI, 0.54-0.81), 2 comorbidities (OR, 0.55; 95%CI, 0.45-0.69), 3 comorbidities (OR, 0.37; 95%CI, 0.29-0.47), 4 comorbidities (OR, 0.33; 95%CI, 0.24-0.45), ≥ 5 comorbidities (OR, 0.21; 95%CI, 0.12-0.36); all P values < .0001 compared to 0.
Conclusions: The number of coronary angiographies performed drops as the number of comorbidities increases in elderly patients with non-ST-segment elevation acute coronary syndrome. More studies are still needed to know what the best management of these patients should be.
Keywords: Comorbidities. Elderly. Acute coronary syndrome. Coronary angiography.
Resumen
Introducción y objetivos: La comorbilidad en ancianos con síndrome coronario agudo sin elevación del segmento ST empeora el pronóstico. El objetivo fue analizar la influencia de la carga de comorbilidad en la decisión del tratamiento invasivo en ancianos con SCASEST.
Métodos: Se incluyeron 7.211 pacientes mayores de 70 años procedentes de 11 registros españoles. Los datos se analizaron en una base de datos conjunta. Se evaluó la presencia de 6 enfermedades simultáneas y su asociación con la realización de coronariografía durante el ingreso.
Resultados: La edad media fue de 79 ± 6 años y la puntuación GRACE media fue de 150 ± 21 puntos. Fueron tratados de manera conservadora 1.179 pacientes (16%). La presencia de cada enfermedad se asoció con un menor abordaje invasivo (ajustado por variables clínicas predictivas): enfermedad cerebrovascular (odds ratio [OR] = 0,78; intervalo de confianza del 95% [IC95%], 0,64-0,95; p = 0,01), anemia (OR = 0,64; IC95%, 0,54-0,76; p < 0,0001), insuficiencia renal (OR = 0,65; IC95%, 0,56-0,75; p < 0,0001), arteriopatía periférica (OR = 0,79; IC95%, 0,65-0,96; p = 0,02), enfermedad pulmonar crónica (OR = 0,85; IC95%, 0,71-0,99; p = 0,05) y diabetes mellitus (OR = 0,85; IC95%, 0,74-0,98; p = 0,03). Asimismo, el aumento del número de enfermedades (carga de comorbilidad) se asoció con menor realización de coronariografías, ajustado por la escala GRACE: 1 enfermedad (OR = 0,66; IC95%, 0,54-0,81); 2 (OR = 0,55; IC95%, 0,45-0,69); 3 (OR = 0,37; IC95%, 0,29-0,47); 4 (OR = 0,33; IC95%, 0,24-0,45); ≥ 5 (OR = 0,21; IC95%, 0,12-0,36); todos p < 0,0001, en comparación con ninguna enfermedad.
Conclusiones: Conforme aumenta la comorbilidad disminuye la realización de coronariografías en ancianos con síndrome coronario agudo sin elevación del segmento ST. Se necesitan estudios que investiguen la mejor estrategia diagnóstico-terapéutica en estos pacientes.
Palabras clave: Comorbilidad. Ancianos. Síndrome coronario agudo. Coronariografía.
Abbreviations:
ACS: acute coronary syndrome. DM: diabetes mellitus. NSTEACS: non-ST-segment elevation acute coronary syndrome.
INTRODUCTION
Population ageing leads to an increase in the number of elderly patients who suffer non-ST-segment elevation acute coronary syndrome (NSTEACS). This population group, that has been misrepresented in large studies, has a great comorbidity burden that increases with age1 and an important impact on prognosis.2-4 The ideal therapeutic strategy for the management of these patients is still unknown. The benefit of an invasive strategy in elderly patients with NSTEACS and comorbidities is still unclear.5-9 In general, elderly patients with comorbidities undergo fewer coronary angiographies despite their worse prognosis.10 This clinical practice —apparently in contrast with the recommendations published in the clinical practice guidelines11— seems to be based on the perception of a scarce benefit due to the worse intrinsic prognosis associated with comorbidities.
In this study the data of 11 Spanish NSTEACS registries were collected to set up a common database with over 7000 elderly patients with NSTEACS. In this preliminary analysis, the objective was to study the impact of comorbidities on the decision to go with invasive approach.
METHODS
Study design
The study was conducted from 11 cohorts of Spanish registries of patients with NSTEACS (annex).2,12-20 All cases were included in a single database of patients with chest pain and a diagnosis of NSTEACS, > 70 years of age and with, at least, a 1-year follow-up.
ANNEX. Registries included in the study.
| Hospital Clínico Universitario, Valencia2 |
| Hospital Universitario Joan XXIII, Tarragona12 |
| Hospital Universitario de Bellvitge, Barcelona13 |
| Hospital Ramón y Cajal, Madrid14 |
| Hospital Universitario de San Juan, Alicante15 |
| LONGEVO multicenter registry16 |
| ACHILLES multicenter registry17 |
| Hospital Álvaro Cunqueiro, Vigo18 |
| Hospital Clínico Universitario, Santiago de Compostela19 |
| Hospital Universitario Vall d’Hebron, Barcelona20 |
| Hospital Universitario de La Princesa, Madrid* |
|
* Unpublished data. |
The anthropometric and social-demographic data, main cardiovascular risk factors, and analytical and hemodynamic data at admission or during hospitalization were registered.
Patients were treated according to each center routine clinical practice and the decision to treat the NSTEACS invasively, with or without a coronary angiography, was left to the discretion of the treating physician. The 6-month mortality GRACE risk score was determined in all the patients.21
A total of 6 conditions that proved to have a higher prognostic impact on elderly patients hospitalized due to acute coronary syndrome (ACS) in a previous study were included:22 renal failure (glomerular filtration rate < 60mL/min/1.73m2), anemia (hemoglobin levels < 11 g/dL), diabetes mellitus (DM), cerebrovascular disease, peripheral arterial disease, and chronic pulmonary disease.
Endpoints
The study primary endpoint was to assess how the presence of comorbidities impacted the decision to perform a coronary angiography during admission.
Statistical analysis
Categorical variables were expressed as absolute values (percentages) and compared using the unpaired Student t test or the ANOVA. The continuous ones were expressed as mean ± standard deviation and compared using the chi-square test.
Initially, the correlation between each disease and the performance of a coronary angiography through univariable analysis were assessed. Then, a first binary logistics regression model was conducted including the 6 conditions and the clinical variables associated with the performance of the coronary angiography in the univariable analysis. The odds ratio (OR) and the 95% confidence intervals (95%CI) were estimated. Afterwards, patients were classified according to their comorbidity burden, defined by the number of concomitant conditions (from 0 to 6). A second logistics regression model was conducted where comorbidity burden was adjusted for the predictive clinical variables in the previous analysis. Finally, a third logistics regression model was conducted where the comorbidity burden was adjusted based on the GRACE risk score. Differences were considered statistically significant with P values < .05
RESULTS
A total of 7211 patients with a mean age of 79 ± 6 years were included; 62% were males. Table 1 shows the population baseline characteristics. The prevalence of comorbidities was DM in 2874 patients (40%), chronic kidney disease in 3070 patients (42.6%), anemia in 1025 (14.2%), peripheral arterial disease in 1006 (14%), chronic pulmonary disease in 1161 (16%), and previous stroke in 831 (11.5%).
Table 1. Differences in the baseline characteristics based on the therapeutic approach
| All N = 7211 | Conservative approach N = 1 179 (16) | Invasive approach N = 6 032 (84) | P | |
|---|---|---|---|---|
| Age (years) | 79 ± 6 | 82 ± 6 | 78 ± 5 | .001 |
| Males | 4 441 (61.6) | 597 (50.6) | 3 844 (63.7) | .0001 |
| Smoking | 621 (8.6) | 72 (6.1) | 549 (9.1) | .0001 |
| Hypertension | 5 723 (79.4) | 943 (80) | 4 780 (79.2) | .58 |
| Dyslipidemia | 4 262 (59) | 609 (51.7) | 3 653 (60.6) | .0001 |
| Previous myocardial infarction | 1 682 (23.3) | 371 (31.7) | 1 308 (21.7) | .0001 |
| Pervious percutaneous coronary intervention | 1 334 (19) | 175 (14.8) | 1 159 (19.2) | .0001 |
| Previous coronary surgery | 573 (7.9) | 104 (8.8) | 469 (7.8) | .24 |
| Previous heart failure | 641 (8.9) | 198 (16.8) | 443 (7.3) | .0001 |
| Killip ≥ 2 | 1 889 (26.2) | 463 (39.3) | 1 426 (23.6) | .0001 |
| ST-segment depression | 2 638 (36.6) | 396 (33.6) | 2 242 (37.2) | .02 |
| High troponin levels | 5 319 (73.7) | 920 (78) | 4 399 (73) | .001 |
| Left ventricular ejection fraction (%) | 54 ± 11 | 54 ± 12 | 55 ± 11 | .03 |
| GRACE | 150 ± 21 | 159 ± 21 | 147 ± 19 | .0001 |
| Comorbidities | ||||
| Anemia | 1 025 (14.2) | 273 (23.2) | 752 (12.5) | .0001 |
| Peripheral arterial disease | 1 006 (14) | 196 (16.6) | 810 (13.4) | .04 |
| Chronic pulmonary disease | 1 161 (16.1) | 210 (17.8) | 951 (15.8) | .08 |
| Diabetes mellitus | 2 874 (39.9) | 522 (44.3) | 2 352 (39) | .0001 |
| Cerebrovascular disease | 831 (11.5) | 186 (15.8) | 645 (10.7) | .0001 |
| Chronic kidney disease | 3 070 (42.6) | 716 (60.7) | 2 354 (39) | .0001 |
|
Data are expressed as no. (%) or mean ± standard deviation. |
||||
During admission 6032 patients (84%) underwent a coronary angiography. A total of 4339 patients (60%) were revascularized: 3848 (53%) of them through percutaneous coronary intervention and 491 (7%) through surgery. Patients on conservative management (1179, 16%) were predominantly women with higher scores in the GRACE score, and a past medical history of infarction or heart failure. Conversely, smoking and high levels of troponins or ST-segment depressions on the electrocardiogram performed at admission and a previous percutaneous coronary intervention were associated with a higher invasive approach (table 1). The GRACE risk score was lower in patients who underwent catheterization (147 ± 19 vs 159 ± 21; P = .0001).
The presence of each of the 6 conditions studied was associated with fewer coronary angiographies performed: chronic kidney disease, 60.7% vs 39% (P = .0001); anemia, 23.2% vs 12.5% (P = .0001); DM, 44.3% vs 39% (P = .0001); cerebrovascular disease, 15.8% vs 10.7% (P = .0001); peripheral arterial disease, 16.6% vs 13.4% (p = .04); and chronic pulmonary disease, 17.8% vs 15.8% (P = .08) (table 1).
In the multivariable analysis adjusted for the main cardiovascular risk factors and clinical variables that were statistically significant in the univariable analysis, the 6 conditions associated with a lower probability of an indication for coronary angiography were: cerebrovascular disease, OR, 0.78 (IC95%, 0.64-0.95; P = .01); anemia, OR, 0.64 (IC95%, 0.54-0.76; P < .0001); chronic kidney disease, OR, 0.65 (IC95%, 0.56-0.75; P < .0001); peripheral arterial disease, OR, 0.79 (IC95%, 0.65-0.96; P = .02); chronic pulmonary disease, OR, 0.85 (IC95%, 0.71-0.99; P = .05); and DM, OR, 0.85 (IC95%, 0.74-0.98; P = .03). Table 2 shows the clinical variables associated with the indication for coronary angiography.
Table 2. Results: multivariable analysis for the indication of a coronary angiography
| Variable | OR | 95%CI | P | |
|---|---|---|---|---|
| Age (years) | 0.89 | 0.88-0.91 | .0001 | |
| Males | 1.48 | 1.28-1.71 | .0001 | |
| Dyslipidemia | 1.44 | 1.26-1.66 | .0001 | |
| Previous myocardial infarction | 0.46 | 0.39-0.54 | .0001 | |
| Previous heart failure | 0.68 | 0.56-0.84 | .0001 | |
| Previous percutaneous coronary intervention | 1.91 | 1.55-2.34 | .0001 | |
| Killip ≥ 2 | 0.68 | 0.56-0.80 | .0001 | |
| ST-segment depression | 1.44 | 1.25-1.66 | .0001 | |
| Left ventricular ejection fraction (by 5%) | 0.98 | 0.98-0.99 | .001 | |
| Anemia | 0.64 | 0.54-0.76 | .0001 | |
| Peripheral artery disease | 0.79 | 0.65-0.96 | .02 | |
| Chronic pulmonary disease | 0.85 | 0.71-0.99 | .05 | |
| Diabetes mellitus | 0.85 | 0.74-0.98 | .03 | |
| Cerebrovascular disease | 0.78 | 0.64-0.95 | .01 | |
| Chronic kidney disease | 0.65 | 0.56-0.75 | .0001 | |
|
95%CI: 95% confidence interval; OR: odds ratio. |
||||
Comorbidity burden was defined as the number of present conditions (from 0 to 6). This was their distribution: 0 conditions, N = 1891 (26%); 1 condition, N = 2413 (33.5%); 2 conditions, N = 1638 (22.7%); 3 conditions, N = 879 (12.2%); 4 conditions, N = 314 (4.4%); and 5 or 6 conditions, N = 76 (1.1%). The analysis of the comorbidity burden adjusted for the clinical variables associated with the indication for coronary angiography showed a negative correlation between the number of conditions and the probability to perform a coronary angiography: 1 condition, OR, 0.66 (95%CI, 0.54-0.81); 2 conditions, OR, 0.55 (95%CI, 0.45-0.69); 3 conditions, OR, 0.37 (95%CI, 0.29-0.46); 4 conditions, OR, 0.32 (95%CI, 0.23-0.45); and 5 or 6 conditions, OR, 0.21 (95%CI, 0.12-0.37); All P values < .0001 compared to no condition.
With more conditions, higher GRACE risk scores (table 3). The negative correlation between the comorbidity burden and the performance of the coronary angiography was kept after adjusting for the GRACE risk score. Figure 1 shows that with more conditions, the probability to perform a coronary angiography increased too (figure 1A) despite the higher risk posed by higher GRACE risk scores (figure 1B, table 3).
Table 3. Distribution of comorbidity burden and the score obtained in the GRACE risk score (P < .0001 for the tendency)
| Conditions | N = 7 211 | GRACE risk score |
|---|---|---|
| 0 | 1891 (26) | 141 ± 18 |
| 1 | 2413 (33.5) | 148 ± 19 |
| 2 | 1638 (22.7) | 153 ± 20 |
| 3 | 879 (12.2) | 160 ± 19 |
| 4 | 314 (4.4) | 162 ± 19 |
| ≥ 5 | 76 (1.1) | 166 ± 17 |
|
Data are expressed as no. (%) or mean ± standard deviation. |
||
Figure 1. A: chances of undergoing a coronary angiography based on the number of concomitant conditions. The odds ratio (OR) with a 95% confidence interval (95%IC) can be seen. Analysis adjusted for the GRACE risk score. B: Representation of the correlation between comorbidity burden and the GRACE risk score. The mean ± standard deviation (SD) of the GRACE risk score can be seen.
DISCUSSION
The main findings of our study were: a) the 6 conditions studied (cerebrovascular disease, anemia, chronic kidney disease, peripheral arterial disease, chronic pulmonary disease, and DM) were independently associated with a lower probability to use the invasive approach; b) with higher comorbidity burdens, considered as the number of concomitant conditions, lower chances of performing coronary angiographies.
There is a high prevalence of comorbidities in elderly patients with NSTEACS that greatly impacts prognosis in the short and mid-term.2,4 The Charlson index is the most commonly used tool to assess comorbidities.23,24 However, the analysis of the 6 conditions studied (chronic kidney disease, anemia, DM, cerebrovascular disease, peripheral arterial disease, and chronic pulmonary disease) has proven to be a useful risk stratification tool and have great predictive discriminatory capabilities that are similar to the Charlson index.22
Comorbidity burden is very important for the in-hospital management of NSTEACS.2,3,6,9,10 Although the optimal therapeutic strategy for the management of elderly patients with NSTEACS is still unknown, several studies show certain benefits with revascularization.5,7,8,25-30
Our study shows that with higher comorbidity burdens, lower chances of undergoing coronary angiographies. This may be due to the fact that comorbidities are seen as contraindications for the invasive approach.10 However, the risk of suffering an acute myocardial infarction according to the GRACE risk score increases parallel to the number of concomitant conditions. Actually, these may be the patients who would benefit the most from an invasive approach.31,32
The presence of each one of these 6 conditions was independently associated with fewer invasive approaches. On the one hand, cerebrovascular disease and peripheral arterial disease are responsible for a greater spread of atherosclerotic disease.33 Anemia has proven to be a powerful predictor of mortality in the ACS setting;34-36 we used the 11 g/dL threshold as the cut-off value that had the greatest impact on mortality in former studies.34 Its specific weight in the decision to administer conservative treatment may be justified by its clear association with the occurrence of hemorrhagic events in the ACS setting.37 Chronic kidney disease is an expression of a greater spread of cardiovascular disease and is independently associated with more mortality after an ACS. There is a linear correlation between the risk of death due to cardiovascular causes and lower glomerular filtration rates.17,38 DM is a powerful predictor of mortality, and not only due to cardiovascular causes. There is a clear correlation between DM and major adverse cardiovascular events, and these are patients at very high risk.39 Chronic pulmonary disease is associated with a worse short-term prognosis after an acute myocardial infarction. Also, in the management of NSTEACS it is associated with diagnostic delays, fewer invasive approaches, and a lower use of drugs for secondary prevention purposes.40
In the multivariable analysis, age, previous acute myocardial infarctions, previous heart failure, Killip class ≥ 2 at admission, and a reduced ejection fraction were associated with fewer invasive approaches. Elderly patients receive fewer evidence-based therapies. The older the age, the lower the rate of performing coronary angiographies.41 On top of age, a past medical history of infarction, heart failure, a reduced ejection fraction, and scores ≥ 2 in the Killip classification are important aspects in the prognosis of ACS that, in general, translate into a worse ventricular function. Paradoxically, our findings suggest that the higher the risk, the lower the chances of performing a coronary angiography. Actually, these findings are consistent with former studies published.10,42 It is possible that the perception of fewer benefits from revascularization or higher risk in the revascularization procedures may explain these results.2 On the other hand, male sex, dyslipidemia, previous percutaneous coronary interventions, and ST-segment depressions at admission were associated with more invasive approaches. Several studies suggest that women undergo fewer invasive approaches compared to men despite the mortality benefits seen.43 Previous angioplasties, ST-segment depressions, and dyslipidemia are probably interpreted as ischemic risk factors, which may explain their association with a higher frequency of invasive approaches.20,28,44
Limitations
The main limitation of our study is that it is an observational registry with its corresponding selection bias and differences in the management of patients depending on the different centers involved. On the other hand, although the multivariable model was adjusted for percutaneous coronary intervention or previous coronary surgeries, it was not adjusted for previous coronary angiographies. It is possible that the previous knowledge of the coronary anatomy impacted the decision to perform fewer coronary angiographies in patients at higher risk.
CONCLUSIONS
The presence of comorbidities greatly impacts the therapeutic decision in elderly patients with ACS. With more conditions, higher GRACE risk scores, and lower chances of indicating a coronary angiography
This paradox of higher-risk and more conservative treatment justifies conducting new studies to determine the benefits of the invasive strategy in elderly patients with NSTEACS and comorbidities to establish the best therapeutic decision.
FUNDING
This article was funded by a grant from the Carlos III Health Institute: CIBERCV 16/11/00420, Madrid, Spain.
CONFLICTS OF INTEREST
J. Sanchis is an associate editor of REC: Interventional Cardiology; the journal’s editorial procedure to ensure impartial handling of the manuscript has been followed. J. Núñez has received funding from Novartis, Vitor Pharma, and Boehringer Ingelheim, and a grant from Astra Zeneca and Vitor Pharma. J.A. Barrabés has received funding for the educational activities conducted for AstraZeneca, and for his job as consultor for Bayer. The remaining authors did not declare any conflicts of interest whatsoever.
WHAT IS KNOWN ABOUT THE TOPIC?
- Elderly patients with NSTEACS have a higher comorbidity burden. Concomitant conditions are associated with worse prognosis. Elderly patients with comorbidities undergo fewer coronary angiographies despite their worse prognosis, which is in sharp contrast with the recommendations published in the clinical practice guidelines.
WHAT DOES THIS STUDY ADD?
- This analysis of a multicenter registry shows the correlation between comorbidity burden and invasive therapeutic approach in elderly patients with NSTEACS. With more concomitant conditions, higher GRACE risk scores, but lower chances of indicating a coronary angiography.
REFERENCES
1. Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education:a cross-sectional study. Lancet. 2012;380:37-43.
2. Sanchis J, Núñez J, BodíV, Núñez E, García-Alvarez A, Bonanad C, et al. Influence of comorbid conditions on one-year outcomes in non-ST-segment elevation acute coronary syndrome. Mayo Clin Proc. 2011;86:291-296.
3. Chirinos JA, Veerani A, Zambrano JP, Schob A, Perez G, Mendez AJ, et al. Evaluation of comorbidity scores to predict all-cause mortality in patients with established coronary artery disease. Int J Cardiol. 2007;117:97-102.
4. Sanchis J, Bonanad C, Ruiz V, Fernández J, García-Blas S, Mainar L, et al. Frailty and other geriatric conditions for risk stratification of older patients with acute coronary syndrome. Am Heart J. 2014;168:784-791.
5. Bardaji A, Barrabés JA, Ribera A, et al. Revascularization in older adult patients with non-ST-segment elevation acute coronary syndrome:effect and impact on 6-month mortality [published online ahead of print, 2019 May 14]. Eur Heart J Acute Cardiovasc Care. 2019;2048∖19849922.
6. Chuang AM, Hancock DG, Halabi A, et al. Invasive management of acute coronary syndrome:Interaction with competing risks. Int J Cardiol. 2018; 269:13-18.
7. Tegn N, Abdelnoor M, Aaberge L, et al. Invasive versus conservative strategy in patients aged 80 years or older with non-ST-elevation myocardial infarction or unstable angina pectoris (After Eighty study):an open-label randomized controlled trial. Lancet. 2016;387:1057-1065.
8. Sanchis J, Núñez E, Barrabés JA, et al. Randomized comparison between the invasive and conservative strategies in comorbid elderly patients with non-ST elevation myocardial infarction. Eur J Intern Med. 2016;35:89-94.
9. Palau P, Núñez J, Sanchis J, et al. Differential prognostic effect of revascularization according to a simple comorbidity index in high-risk non-ST- segment elevation acute coronary syndrome. Clin Cardiol. 2012;35:237-243.
10. Savonitto S, Morici N, De Servi S. Treatment of acute coronary syndromes in the elderly and in patients with comorbidities. Rev Esp Cardiol. 2014;67:564-573.
11. Roffi M, Patrono C, Collet JP, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation:Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016;37:267-315.
12. Camprubi M, Cabrera S, Sans J, et al. Body Mass Index and Hospital Mortality in Patients with Acute Coronary Syndrome Receiving Care in a University Hospital. J Obes. 2012;2012:287939.
13. Ariza-SoléA, Sánchez-Salado JC, Lorente V, et al. Is it possible to separate ischemic and bleeding risk in patients with non-ST segment elevation acute coronary syndromes?Int J Cardiol. 2014;171:448-450.
14. Alonso Salinas GL, Sanmartín Fernández M, Pascual Izco M, et al. Frailty predicts major bleeding within 30 days in elderly patients with Acute Coronary Syndrome. Int J Cardiol. 2016;222:590-593.
15. Cordero A, López-Palop R, Carrillo P, et al. Prevalence and Postdischarge Incidence of Malignancies in Patients With Acute Coronary Syndrome. Rev Esp Cardiol. 2018;71:267-273.
16. Alegre O, Formiga F, López-Palop R, et al. An Easy Assessment of Frailty at Baseline Independently Predicts Prognosis in Very Elderly Patients With Acute Coronary Syndromes. J Am Med Dir Assoc. 2018;19:296-303.
17. Rivera-Caravaca JM, Ruiz-Nodar JM, Tello-Montoliu A, et al. Disparities in the Estimation of Glomerular Filtration Rate According to Cockcroft-Gault, Modification of Diet in Renal Disease-4, and Chronic Kidney Disease Epidemiology Collaboration Equations and Relation With Outcomes in Patients With Acute Coronary Syndrome. J Am Heart Assoc. 2018;7:e008725.
18. Abu-Assi E, Raposeiras-Roubin S, Cobas-Paz R, et al. Assessing the performance of the PRECISE-DAPT and PARIS risk scores for predicting one-year out-of-hospital bleeding in acute coronary syndrome patients. EuroIntervention. 2018;13:1914-1922.
19. Álvarez Álvarez B, Abou Jokh Casas C, Cordero A, et al. Early revascularization and long-term mortality in high-risk patients with non-ST-elevation myocardial infarction. The CARDIOCHUS-HUSJ registry. Rev Esp Cardiol. 2020;73:35-42.
20. MilàL, Barrabés JA, Lidón RM, et al. Prior adherence to recommended lipid control targets in patients admitted for acute coronary syndrome. Rev Esp Cardiol. 2019;73:376-382.
21. Eagle KA, Lim MJ, Dabbous OH, et al. A validated prediction model for all forms of acute coronary syndrome:estimating the risk of 6-month postdischarge death in an international registry. JAMA. 2004:291:2727-2733.
22. Sanchis J, Soler M, Núñez J, et al. Comorbidity assessment for mortality risk stratification in elderly patients with acute coronary syndrome. Eur J Intern Med. 2019;62:48-53.
23. Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies:development and validation. J Chronic Dis. 1987;40:373-383.
24. Núñez J, Núñez E, Fácila L, et al. Prognostic value of Charlson comorbidity index at 30 days and 1 year after acute myocardial infarction. Rev Esp Cardiol. 2004;57:842-849.
25. De Servi S, Cavallini C, Dellavalle A, et al. Non-ST-elevation acute coronary syndrome in the elderly:treatment strategies and 30-day outcome. Am Heart J. 2004;147:830-836.
26. Sillano D, Resmini C, Meliga E, et al. Retrospective multicenter observational study of the interventional management of coronary disease in the very elderly:the NINETY. Catheter Cardiovasc Interv. 2013;82:414-421.
27. Kolte D, Khera S, Palaniswamy C, et al. Early invasive versus initial conservative treatment strategies in octogenarians with UA/NSTEMI. Am J Med. 2013;126:1076-1083.
28. Núñez J, Ruiz V, Bonanad C, et al. Percutaneous coronary intervention and recurrent hospitalizations in elderly patients with non ST-segment acute coronary syndrome:The role of frailty. Int J Cardiol. 2017;228:456-458.
29. LlaóI, Ariza-SoléA, Sanchis J, et al. Invasive strategy and frailty in very elderly patients with acute coronary syndromes. EuroIntervention. 2018;14:e336-342.
30. Sanchis J, Ariza-SoléA, Abu-Assi E, et al. Invasive Versus Conservative Strategy in Frail Patients With NSTEMI:The MOSCA-FRAIL Clinical Trial Study Design. Rev Esp Cardiol. 2019;72:154-159.
31. de Groot V, Beckerman H, Lankhorst GJ, et al. How to measure comorbidity. A critical review of available methods. J Clin Epidemiol. 2003;56:221-229.
32. Park JY, Kim MH, Bae EJ, et al. Comorbidities can predict mortality of kidney transplant recipients:comparison with the Charlson comorbidity index. Transplant Proc. 2018;50:1068-1073.
33. Chirinos JA, Veerani A, Zambrano JP, et al. Evaluation of comorbidity scores to predict all-cause mortality in patients with established coronary artery disease. Int J Cardiol. 2007;117:97-102.
34. Lawler PR, Filion KB, Dourian T, et al. Anemia and mortality in acute coronary syndromes:a systematic review and meta-analysis. Am Heart J. 2013;165:143-153.
35. Ford I, Bezlyak V, Stott DJ, et al. Reduced glomerular filtration rate and its association with clinical outcome in older patients at risk of vascular events:secondary analysis. PLoS Med. 2009;6:e16.
36. Sabatine MS, Morrow DA, Giugliano RP, et al. Association of hemoglobin levels with clinical outcomes in acute coronary syndromes. Circulation. 2005;111:2042-2049.
37. Vicente-Ibarra N, Marín F, Pernias-Escrig V, et al. Impact of anemia as risk factor for major bleeding and mortality in patients with acute coronary syndrome. Eur J Intern Med. 2019;61:48-53.
38. Goldenberg I, Subirana I, Boyko V, et al. Relation between renal function and outcomes in patients with non-ST-segment elevation acute coronary syndrome:real-world data from the European Public Health Outcome Research and Indicators Collection Project. Arch Intern Med. 2010;170:888-895.
39. Rao Kondapally Seshasai S, Kaptoge S, Thompson A, et al. Diabetes mellitus, fasting glucose, and risk of cause-specific death [published correction appears in N Engl J Med. 2011;364:1281]. N Engl J Med. 2011;364:829-841.
40. Rothnie KJ, Smeeth L, Herrett E, et al. Closing the mortality gap after a myocardial infarction in people with and without chronic obstructive pulmonary disease. Heart. 2015;101:1103-1110.
41. Avezum A, Makdisse M, Spencer F, et al. Impact of age on management and outcome of acute coronary syndrome:observations from the Global Registry of Acute Coronary Events (GRACE). Am Heart J. 2005;149:67-73.
42. Itzahki Ben Zadok O, Ben-Gal T, Abelow A, et al. Temporal Trends in the Characteristics, Management and Outcomes of Patients With Acute Coronary Syndrome According to Their Killip Class. Am J Cardiol. 2019;124:1862-1868.
43. Mehta LS, Beckie TM, DeVon HA, et al. Acute Myocardial Infarction in Women:A Scientific Statement From the American Heart Association. Circulation. 2016;133:916-947.
44. Yudi MB, Clark DJ, Farouque O, et al. Trends and predictors of recurrent acute coronary syndrome hospitalizations and unplanned revascularization after index acute myocardial infarction treated with percutaneous coronary intervention. Am Heart J. 2019;212:134-143.