To the Editor,
Coronary artery calcification occurs in up to 1 in 5 patients with ST-segment elevation myocardial infarction (STEMI),1 and its prevalence is expected to rise with population aging and the increasing burden of associated comorbidities. Calcification complicates percutaneous coronary intervention (PCI) and is associated with worse technical and clinical outcomes, including higher rates of in-stent thrombosis, target-lesion revascularization, reinfarction, and mortality.1,2 Therefore, appropriate lesion preparation using plaque modification techniques is essential. Although rotational atherectomy (RA) (ROTABLATOR/ROTAPRO, Boston Scientific, United States) is a widely used procedure for treating severely calcified lesions, evidence on its safety and efficacy profile in patients with STEMI remains limited.
We present a retrospective case series of patients with STEMI treated with RA between 2011 and 2023 at our center. Clinical and angiographic data were collected. Success rate was defined as successful stent implantation with residual percent diameter stenosis < 20% and distal Thrombolysis in Myocardial Infarction (TIMI) grade-III flow, without major in-hospital complications. Clinical follow-up was performed according to the standard practice of the unit.
Between 2011 and 2023, only 4 of 2490 patients with STEMI (0.16%) required RA due to severely calcified lesions that prevented conventional balloon dilation or in which such dilation was insufficient to achieve successful PCI (table 1). The main clinical aspects of each case are described below (figure 1).
Table 1. Main characteristics of the procedures
| Case | Sex and age | Comorbidity | Clinical presentation | Vascular access | Target vessel | Devices used | Burr size | Type and size of stent | Procedural time (min) | Contrast (mL) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Female, 74 years | Hypertension, diabetes mellitus, dyslipidemia, prior STEMI treated with thrombolysis | Inferior STEMI | Radial artery | RCA | 1.25 mm × 10 mm semicompliant balloon, 2 mm × 6 mm cutting balloon, 3 mm × 6 mm cutting balloon, 3.5 mm × 8 mm noncompliant balloon, 3.5 mm × 10 mm high-pressure balloon | 1.25 mm | 3.5 mm × 38 mm DES | 174 | 200 |
| 2 | Male, 67 years | Current smoker, dyslipidemia, prior PCI in left circumflex artery | Anterior STEMI | Radial artery | LAD | 2.5 mm × 15 mm noncompliant balloon, 2.75 mm × 15 mm, noncompliant balloon, 3 mm × 12 mm intracoronary lithotripsy balloon, 3 mm × 8 mm noncompliant balloon | 1.25 mm and 1.75 mm | 3.5 mm × 30 mm DES | 115 | 159 |
| 3 | Male, 84 years | Hypertension, diabetes mellitus, dyslipidemia, peripheral vascular disease | Anterior STEMI | Femoral artery | LAD | 2.5 mm × 15 mm noncompliant balloon, 2.5 mm × 6 mm cutting balloon, 3 mm × 14 mm noncompliant balloon, 3.35 mm × 15 mm noncompliant balloon | 1.5 mm | 3 mm × 38 mm DES | 113 | 250 |
| 4 | Male, 83 years | Hypertension, dyslipidemia, peripheral vascular disease | Anterior STEMI | Femoral artery | LAD | 2 mm × 15 mm noncompliant balloon, 2.5 mm × 15 mm noncompliant balloon, 2.5 mm × 6 mm cutting balloon, 3 mm × 8 mm noncompliant balloon | 1.25 mm | 2.75 mm × 13 mm DES | 112 | 111 |
|
DES: drug-eluting stent; LAD: left anterior descending coronary artery; PCI: percutaneous coronary intervention; RCA: right coronary artery; STEMI: ST-segment elevation myocardial infarction. |
||||||||||
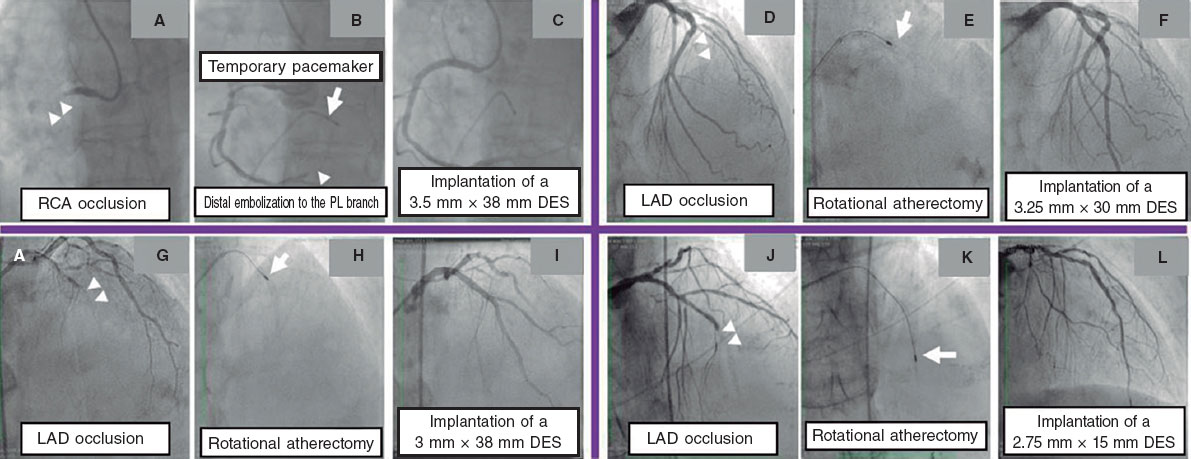
Figure 1. Images of percutaneous coronary interventions in the patient series. A: proximal occlusion of the right coronary artery (RCA) (arrowheads mark the occlusion site). B: temporary pacemaker implantation (arrow); after rotational atherectomy, distal embolization of the posterolateral artery (PL) is observed (arrowhead). C: deployment of a 3.5 mm × 38 mm DES. D: mid-LAD occlusion with severely calcified lesion (arrowheads). E: rotational atherectomy with a 1.25-mm burr (arrow). F: deployment of a 3.25 mm × 30 mm DES. G: mid-LAD occlusion (arrowheads). H: rotational atherectomy with a 1.5-mm burr (arrow). I: deployment of a 3 mm × 38 mm DES. J: mid-LAD occlusion (arrowheads). K: rotational atherectomy with a 1.25-mm burr (arrow). L: deployment of a 2.75 mm × 15 mm DES.
Case No. 1 involved a 74-year-old woman referred for emergency PCI due to an inferior subepicardial lesion. The right coronary artery showed severe calcification with acute proximal occlusion. A work guidewire was successfully advanced distally using a XBRCA catheter (Cordis Corporation, United States). However, further attempts to pass a thrombus aspiration catheter or a 1-mm balloon were unsuccessful. The guidewire was exchanged for a ROTAWIRE Floppy (Boston Scientific, United States) using a microcatheter, and RA was performed with a 1.25-mm burr after placement of a temporary pacemaker via femoral vein. After RA, antegrade flow was restored, allowing dilation with 2.5-mm and 3.0-mm balloons. A drug-eluting stent (DES) was then implanted in the right coronary artery, yielding an optimal final result.
Case No. 2 was a 67-year-old man who presented with anterior STEMI. Coronary angiography revealed a proximal medial occlusion of the left anterior descending coronary artery (LAD). Using a 6-Fr EBU 3.75 catheter (Medtronic, United States), the lesion was crossed, restoring distal flow, and a critically calcified plaque was identified. Predilation with semi- and noncompliant balloons achieved inadequate expansion. Although intracoronary lithotripsy was attempted, the balloon could not be advanced despite the use of a catheter extension system. RA was performed with a 1.25-mm burr, and due to persistent poor balloon expansion, it was repeated with a 1.75-mm burr. Subsequent dilation with a 3-mm cutting balloon was satisfactory. Intravascular ultrasound (IVUS) showed multiple calcium fractures. A 3.5 mm × 30-mm DES was ultimately implanted, and IVUS confirmed an optimal result.
Case No. 3 involved an 84-year-old man with anterior STEMI. Angiography revealed acute proximal occlusion of the LAD. Thrombus aspiration was performed with a 6-Fr EBU 4 catheter, which retrieved abundant thrombotic material. The lesion was unsuccessfully predilated with a 2.5-mm cutting balloon and a 2.5-mm noncompliant balloon at high pressure. RA with a 1.5-mm burr allowed adequate balloon expansion. A 3 mm × 38 mm drug-eluting stent was subsequently implanted, achieving an optimal final result without complications.
Case No. 4 was an 83-year-old man who presented with ventricular tachycardia treated with procainamide. The electrocardiogram showed anterior ST-segment elevation, and emergency PCI was indicated. Acute occlusion of the mid-LAD was identified. Using a 6-Fr EBU 3.75 catheter, the lesion was crossed with a Pilot 50 guidewire. Although IVUS was attempted, the device could not fully cross the lesion; however, concentric calcification was confirmed at the site of maximal stenosis. RA was performed with a 1.25-mm burr. During the procedure, the patient developed hypotension requiring low-dose norepinephrine infusion. After RA, dilation was achieved with cutting and noncompliant 2.5-mm balloons, followed by the successful implantation of a 2.75 mm × 15 mm DES. Norepinephrine was progressively withdrawn in the cath lab.
In all cases, flow was restored, adequate predilation achieved, and a DES successfully deployed with satisfactory angiographic results (table 1). IVUS was used in 2 of the 4 patients; notably, these were the most recent cases, reflecting increased awareness of the benefits of imaging modalities to optimize procedural outcomes in patients with coronary calcification over the past decade. The mean procedural time was 133 ± 31 minutes. At the 2-year follow-up, all 4 patients were alive, and did not require any additional interventional procedures or hospital readmissions for cardiovascular causes.
Coronary artery calcification is associated with advanced age, smoking, and chronic kidney disease, and is present in up to one-third of patients undergoing PCI.2,3 Severe calcification, defined visually or by intracoronary imaging, hinders stent implantation and expansion and increases the risk of complications.4 Newer plaque modification techniques promise improved outcomes.5 RA enables calcium fracture using a diamond-coated rotating burr, increasing arterial compliance and facilitating device passage and stent expansion.
Large RA studies have systematically excluded acute coronary syndrome, particularly STEMI, due to the higher risk of complications. The ROTATE Registry,5 which included primarily patients with non–ST-elevation acute coronary syndrome or chronic coronary disease, found comparable success rates but higher complication rates in the acute setting. The ROTA-STEMI Registry6 analyzed 104 patients with STEMI treated with RA during PCI across 12 European centers from 2002 through 2021. RA was mainly used as a bailout strategy (76.9%). Although the procedural success rate (stent implanted, TIMI grade-3 flow, and residual percent diameter stenosis < 30%) was 86.5%, the in-hospital mortality rate reached 18.3% overall, with marked differences depending on hemodynamic status (50% in shock vs 1.5% without shock). These findings support the feasibility of RA in selected cases of STEMI.
Relative contraindications for RA in STEMI include the risk of distal embolization, vasospasm, and the RA-induced prothrombotic state, which enhances platelet activation and worsens slow-flow/no-reflow.4 In our case series, the rate of technical success was 100%, with no major complications or cardiovascular events during 2-year follow-up. Although our study did not include a systematic analysis of unsuccessful primary PCI, RA seems to be a safe and effective technique for treating severely calcified lesions even in the acute STEMI setting, when performed by experienced operators.
In conclusion, multicenter clinical trials with robust design and adequate sample size are needed to specifically assess the safety and efficacy profile of plaque modification strategies in patients with STEMI and severe coronary calcification, including RA, traditionally reserved for bailout cases.
FUNDING
None declared.
ETHICAL CONSIDERATIONS
The study was approved by Hospital del Mar Research Ethics Committee. Because of its retrospective design and anonymization of data, the requirement for informed consent was waived. According to SAGER guidelines, sex and gender variables were considered.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCE
No artificial intelligence was used in the preparation of this article.
AUTHORS’ CONTRIBUTIONS
A. Prieto-Lobato drafted the manuscript and was responsible for data acquisition and analysis. H. Tizón-Marcos conceived the study and reviewed the manuscript. J.C. Betancourt and X. Armario participated in data collection. B. Vaquerizo and H. Cubero reviewed the manuscript. All authors approved the final version.
CONFLICTS OF INTEREST
None declared.
REFERENCES
1. Généreux P, Madhavan MV, Mintz GS, et al. Ischemic outcomes after coronary intervention of calcified vessels in acute coronary syndromes: pooled analysis from HORIZONS-AMI and ACUITY trials. J Am Coll Cardiol. 2014;63:1845-1854.
2. Madhavan MV, Tarigopula M, Mintz GS, et al. Coronary artery calcification: pathogenesis and prognostic implications. J Am Coll Cardiol. 2014;63: 1703-1714.
3. Barbato E, Carrié D, Dardas P, et al. European expert consensus on rotational atherectomy. EuroIntervention. 2015;11:30-36.
4. Jurado-Román A, Gómez-Menchero A, Gonzalo N, et al. Plaque modification techniques to treat calcified coronary lesions. Position paper ACI-SEC. REC Interv Cardiol. 2023;5:46-61.
5. Iannaccone M, Piazza F, Boccuzzi GG, et al. Rotational atherectomy in acute coronary syndrome: early and midterm outcomes. EuroIntervention. 2016; 12:1457-1464.
6. Hemetsberger R, Mankerious N, Muntané-Carol G, et al. In-hospital Outcomes of Rotational Atherectomy in ST-Elevation Myocardial Infarction: Results From the Multicentre ROTA-STEMI Network. Can J Cardiol. 2024; 40:1226-1233.










