An 80-year-old man with maintenance hemodialysis presented with exertional angina. Coronary angiography demonstrated a subtotal occlusion with severe calcification (figure 1A, yellow line) of the right coronary artery. After predilation with a 1.5-mm balloon, optical frequency domain imaging (OFDI; Terumo, Japan) identified layered plaque (LP) (figure 1B, arrow), honeycomb-like structures (HLS) (figure 1C, arrowheads), and a calcified nodule (CN) with a thick calcified plate (figure 1D, asterisk and arrowheads). Because LP and HLS may contain organized thrombi, conventional rotational atherectomy (RA) could disrupt these vulnerable structures, resulting in distal embolization and no-reflow. Therefore, we performed selective orbital atherectomy (OA) using the Diamondback 360 system (Abbott Vascular, United States). A 1.25-mm crown was advanced toward the distal calcified segment without use of the glide-assist mode. OA was performed using a controlled pullback technique, focusing selectively on the calcified lesion while preserving adjacent vulnerable structures. Afterward, the treated segment was dilated with a 2.5-mm scoring balloon. OFDI confirmed no severe damage to the LP (figure 1E) or HLS (figure 1F), with successful calcified nodule debulking (figure 1G, dotted line). No distal embolization or no-reflow occurred. Two drug-eluting stents were implanted, followed by postdilatation with a 3.5-mm high-pressure balloon. Final OFDI (figure 1H-J) and angiography (figure 1K) confirmed excellent stent expansion. Informed consent was obtained.
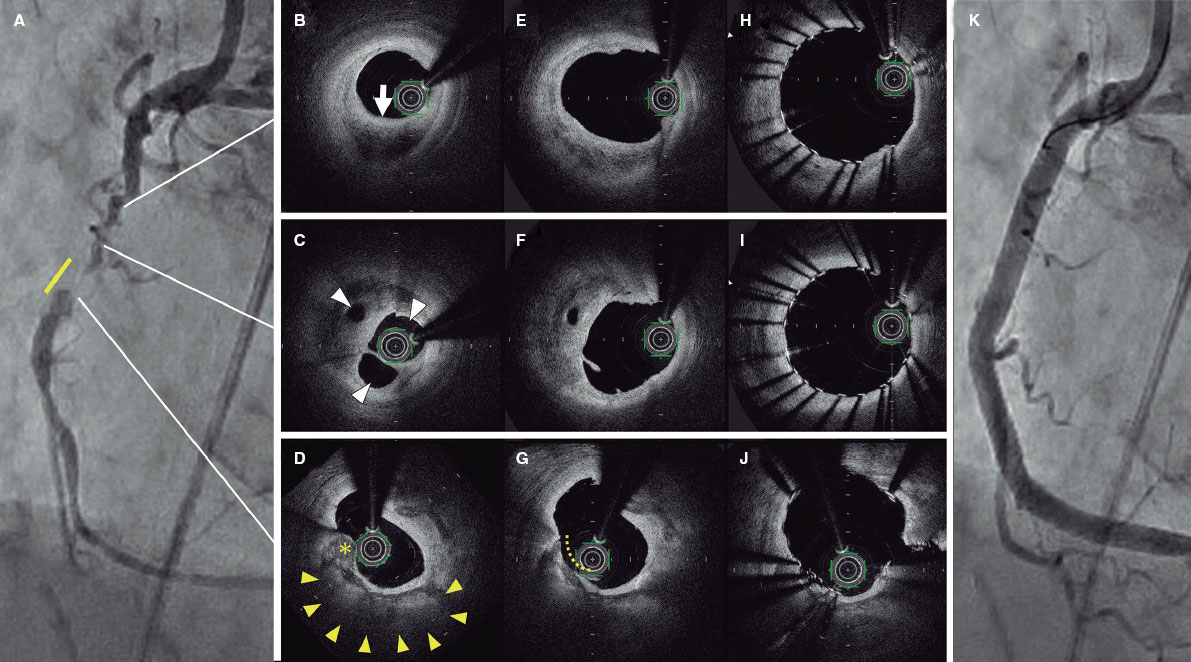
Figure 1.
When treating calcified lesions, the choice between RA and OA can be challenging. This case demonstrates the unique advantages of OA, which allows selective debulking using a controlled pullback technique that targets only the calcified lesion while carefully avoiding the adjacent vulnerable areas.
FUNDING
None declared.
ETHICAL CONSIDERATIONS
Informed consent was obtained from the patient for tests and publication of this case. Because this is a single case report, most SAGER guideline recommendations do not apply. The patient’s gender (man) has been specified. However, as this is a case report rather than a research study, further considerations were deemed unnecessary.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCE
No artificial intelligence has been used in the preparation of this article.
AUTHORS’ CONTRIBUTIONS
S. Koga drafted the initial version of the manuscript and selected and edited the images that would later be used. M. Kunimoto and K. Isoda collaborated in the manuscript critical review and approved its final version.
CONFLICTS OF INTEREST
None declared.










