We have witnessed a remarkable evolution in the field of percutaneous coronary intervention (PCI) over the past half a century, transitioning from the first cases of balloon angioplasty to bare metal stents and, most notably, to the widespread use of drug-eluting stents (DES). The advent of DES substantially reduced restenosis rates by providing a mechanical scaffold combined with sustained release of an antiproliferative drug, eg, taxanes and then rapamycin derivatives. Considering their permanent and static nature, such metallic implants are not without limitations, including the potential for delayed healing, chronic inflammation, inhibition of positive vessel remodeling, and the need for prolonged antithrombotic therapy.1,2 Following this, the concept of bioresorbable vascular scaffolds emerged, promising a temporary scaffold that would “leave nothing behind”. Nonetheless, their initial promise was hampered by late scaffold thrombosis and a high rate of target lesion failure.3 At the same time, drug-coated balloons (DCB) emerged as a “metal-free” alternative delivering an antiproliferative drug to the vessel wall without leaving a permanent implant, thus preserving vessel anatomy, function, and allowing for adaptive remodeling. Currently, DCB are established in percutaneous coronary intervention (PCI) for in-stent restenosis (ISR) and, subsequently, for small-vessel native disease. Their role in larger native coronary arteries, however, remains debated, given the limited evidence from small randomized controlled trials (RCTs) with relatively short follow-up.4
In this context, in a recent paper published in REC: Interventional Cardiology, Sorolla Romero et al. report a timely and rigorous meta-analysis of RCT comparing DCB with DES in patients with native large coronary artery disease (PROSPERO CRD42024602012).5 A total of 2961 patients (n = 1476 for DCB and n = 1485 for DES) from 7 RCT published from 2016 through 2024 were included, and, compared with DES, DCB were associated with a similar risk of the primary endpoint of target lesion revascularization, and all-cause and cardiovascular mortality, myocardial infarction, and major adverse cardiovascular events, but a > 2-fold risk of target vessel revascularization. For angiographic outcomes, although DCB caused less late lumen loss, they were associated with a smaller minimal lumen diameter at follow-up. In light of these results, we hereby hope to provide current and future perspectives on the role of DCB for treatment of native large coronary artery disease.
LESION CHARACTERISTICS
The type of lesions included in the analyzed RCT is a key determinant of the external validity of the study findings, and we outline key considerations below.
- – Across the 7 RCT, patients with high clinical and anatomical complexity were consistently excluded (table 1).6-12 Notably, patients with extensive coronary artery disease (eg, long or multiple lesions, 3-vessel disease, or those requiring multiple devices), severe calcification, left main involvement, or chronic total occlusions were not evaluated. Additional characteristics that appeared among exclusion criteria, and could instead arguably represent favorable scenarios for DCB angioplasty, are requirement for hemodialysis, bifurcations lesions requiring treatment of both branches, and severe coronary artery tortuosity. This selective enrollment underscores the contrast with recent observational studies of DCB use in native large coronary artery disease, which have examined more complex scenarios in which DES may be less effective, technically challenging to deliver, or best avoided to limit long stent segments or multiple overlapping implants (figure 1).13-15
- – The degree of inter-study variability is also of note, particularly given the disproportionate contribution of individual RCT. As appropriately highlighted by the authors, REC-CAGEFREE I7 alone accounts for approximately 75% of the total patient population, and leave-one-out analyses yield different results. Moreover, enrollment periods span 8 years (2014–2022), introducing potential variability in procedural techniques, device technology, and adjunctive pharmacotherapy. The observed prediction intervals and measures of heterogeneity further support this consideration.
- – We acknowledge the clinical variability in defining “large” coronary artery disease. This meta-analysis applied a ≥ 2.5 mm-cutoff to define large vessels, which is at the lower end of what many would consider large. In several of the included studies, patients were eligible for enrollment regardless of treated vessel diameter, with some RCT allowing lesions within reference vessel diameters as small as 2.0 mm (table 1). Subgroup analyses within individual studies provide more specific insights into patients treated with larger devices. Given the significant interaction P value in the vessel size subgroup analysis of the largest included RCT,7 it is reasonable to question whether the overall results would have been superimposable had the analysis been limited to larger vessels. These observations should be interpreted in the context of the earlier discussion on the type of lesions included. Finally, this aspect may have sex-specific relevance: although women generally have smaller coronary vessels, a vessel of a given diameter may be more proximal and supply a larger myocardial territory in women than in men, potentially amplifying its clinical significance.16
Table 1. Clinical, angiographic and procedural characteristics excluding patients from each study included in the meta-analysis
| Characteristics | Nishiyama et al.6 (CCS) N = 60 | REC-CAGEFREE I7 (45%, CCS; 55%, ACS) N = 2271 | Yu et al.8 (11%, CCS; 89%, ACS) N = 170 | REVELATION9 (STEMI) N = 120 | Wang et al.10 (STEMI) N = 184 | Gobi´c et al.11 (STEMI) N = 75 | Hao et al.12 (STEMI) N = 80 |
|---|---|---|---|---|---|---|---|
| Age, years | > 70 | > 80 | |||||
| Hemodialysis | X | ||||||
| Previous MI | X | ||||||
| Previous PCI/CABG | Within 6 months | Within 6 months | |||||
| Vessel size, mm | < 2.25 or > 4.0 | < 2.0 or > 4.0 | < 2.5 or > 4.0 | ||||
| Lesion length, mm | ≥ 25 | > 30 | |||||
| No. of DES or DCB/total DES or DCB length, mm | ≥ 3/> 60 | ||||||
| Extensive CAD | ≥ 3 lesions/vessels | X | |||||
| Severe calcification or atherectomy | X | X | X | X | |||
| Left main coronary artery | X | X | |||||
| CTO | X | X | |||||
| Bifurcation requiring treatment in both branches | X | ||||||
| Grafts | X | ||||||
| Severe coronary artery tortuosity | X | ||||||
|
ACS, acute coronary syndrome; CABG, coronary artery bypass grafting; CAD, coronary artery disease; CCS, chronic coronary syndrome; CTO, chronic total coronary occlusion; DCB, drug-coated balloon; DES, drug-eluting stent; MI, myocardial infarction; PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction. |
|||||||
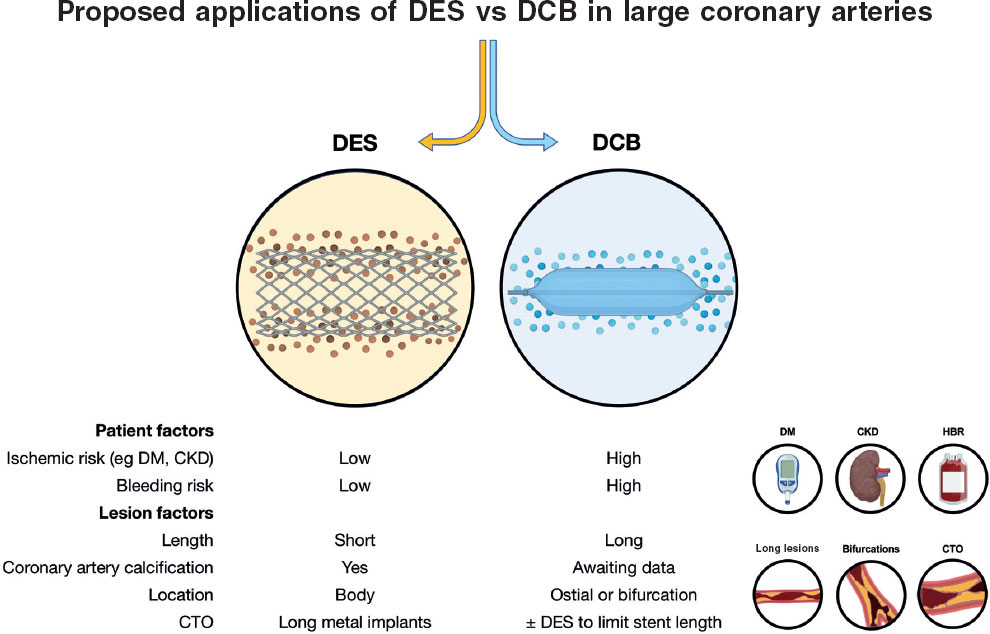
Figure 1. Patient and lesion factors to be taken into consideration when evaluating native large coronary artery disease for percutaneous coronary intervention. Presence of any one of the factors highlighted beneath DCB should lead the operator to contemplate an approach to limit the number of permanent coronary artery implants. ACS, acute coronary syndrome; CKD, chronic kidney disease; CTO, chronic total coronary occlusion; DCB, drug-coated balloon; DES, drug-eluting stent; DM, diabetes mellitus; HBR, high bleeding risk.
LESION PREPARATION
Lesion preparation is a point of significant heterogeneity among the RCT included in the meta-analysis. For example, the REVELATION trial,9 conducted on patients with ST-segment elevation myocardial infarction, permitted proceeding with DCB angioplasty with a 50% residual percent diameter stenosis after predilation, and thrombectomy if visible thrombus was present, which contrasts with the more commonly embraced ≤ 30% threshold.5 Further complicating the procedural comparison is the timing of patient randomization, as 2 studies randomized patients before assessing the outcome of lesion preparation.10,11 Moreover, the specific methods of lesion preparation varied, with 1 study supporting the use of semicompliant balloon angioplasty before DCB inflation.12 The success of DCB angioplasty depends on a dedicated procedural strategy that hinges on meticulous lesion preparation and careful postoperative assessment, a nuance often lost when comparing outcomes across various methodologies.15,17,18
DCB CHARACTERISTICS
The field is characterized by a diversity of DCB platforms, antiproliferative agents and coatings. While the included RCT largely focus on paclitaxel-coated balloons, a growing body of evidence highlights differences in vascular response, downstream effects, and pharmacokinetics across different DCB, indicating that the choice of drug and coating technology could arguably influence clinical outcomes. Sirolimus-coated balloons have recently shown promising results in various clinical settings. Moving forward, future efforts should continue to differentiate between different technologies, as their clinical performance may not be uniform.19,20 Of note, the balloon coating and mechanism of drug release are also key aspects that should be taken into consideration. The DCB technologies assessed in this meta-analysis all used paclitaxel coating but different in platform; only 3 trials evaluated the same device (DCB; SeQuent Please, B. Braun, Germany) whereas the remaining studies used distinct systems, including an ultrasound-controlled paclitaxel delivery platform.10 Finally, inflation time is important for drug delievery and this was not uniform in the studies included in the meta-analysis, with recommended DCB inflation times as low as 30 seconds.6 Recommendations among studies currently enrolling (MAGICAL SV [NCT06271590] and Prevail Global [NCT06535854]) are also slightly different, and whether this might have clinical implications is still to be elucidated.
ANGIOGRAPHIC AND CLINICAL OUTCOMES
DES implantation typically provides a larger acute gain in lumen diameter than balloon angioplasty, a concept highlighted also within the REVELATION trial,9 where the residual percent diameter stenosis to define a successful procedure was different after DCB angioplasty (< 30%) and DES implantation (< 20%). While the meta-analysis reports the endpoint late lumen loss, we recognize that this metric may not fully capture the relative efficacy of these 2 technologies. The use of endpoints, such as net lumen gain, providing a more comprehensive and meaningful comparison between these 2 fundamentally different strategies by focusing on the overall therapeutic effect on the vessel lumen, rather than just the restenotic response following the intervention, should be implemented in upcoming studies. In addition, we acknowledge the limitation in comparing the incidence rate of composite endpoints such as major adverse cardiovascular events when these include different single components across the studies. Finally, we highlight the importance for future studies to concentrate on the reporting of any target vessel thrombosis, a key safety endpoint which remained underreported in the meta-analysis. Still, a significant concern in clinical practice and a key factor impacting the wider implementation of a DCB-based strategy (COPERNICAN [NCT06353594]).
CONCLUSIONS
The meta-analysis by Sorolla Romero et al. provides a timely summary of the current evidence on the use of DCB in large native coronary arteries, and its findings provide hypothesis-generating evidence that challenges the long-standing paradigm of DES as the default choice for any lesion. This work underscores that the evolution of PCI is ongoing and invites reconsideration of therapeutic algorithms toward a more personalized approach, in which the choice between DCB and DES is guided by patient- and lesion-specific factors (figure 1). Moving forward, the focus must shift towards refining patient selection, optimizing procedural techniques, and conducting further RCT with long-term follow-up to clarify the role of DCB in this new therapeutic paradigm.
FUNDING
None declared.
CONFLICTS OF INTEREST
None declared.
REFERENCES
1. Colombo A, Leone PP. Redefining the way to perform percutaneous coronary intervention:a view in search of evidence.
2. Colombo A, Leone PP, Ploumen EH, von Birgelen C. Drug-coated balloons as a first choice for patients with de novo lesions:pros and cons.
3. Regazzoli D, Latib A, Ezhumalai B, et al. Long-term follow-up of BVS from a prospective multicenter registry:Impact of a dedicated implantation technique on clinical outcomes.
4. Camaj A, Leone PP, Colombo A, et al. Drug-Coated Balloons for the Treatment of Coronary Artery Disease:A Review.
5. Sorolla Romero JA, Novelli L, LLau Garcia J, et al. Drug-coated balloons vs drug-eluting stents for the treatment of large native coronary artery disease. Meta-analysis of randomized controlled trials.
6. Nishiyama N, Komatsu T, Kuroyanagi T, et al. Clinical value of drug-coated balloon angioplasty for de novo lesions in patients with coronary artery disease.
7. Gao C, He X, Ouyang F, et al. Drug-coated balloon angioplasty with rescue stenting versus intended stenting for the treatment of patients with de novo coronary artery lesions (REC-CAGEFREE I):an open-label, randomised, non-inferiority trial.
8. Yu X, Wang X, Ji F, et al. A Non-inferiority, Randomized Clinical Trial Comparing Paclitaxel-Coated Balloon Versus New-Generation Drug-Eluting Stents on Angiographic Outcomes for Coronary De Novo Lesions.
9. Vos NS, Fagel ND, Amoroso G, et al. Paclitaxel-Coated Balloon Angioplasty Versus Drug-Eluting Stent in Acute Myocardial Infarction:The REVELATION Randomized Trial.
10. Wang Z, Yin Y, Li J, et al. New Ultrasound-Controlled Paclitaxel Releasing Balloon vs. Asymmetric Drug-Eluting Stent in Primary ST-Segment Elevation Myocardial Infarction-A Prospective Randomized Trial.
11. Gobi´c i D, Tomuli´c V, Luli´c D, et al. Drug-Coated Balloon Versus Drug-Eluting Stent in Primary Percutaneous Coronary Intervention:A Feasibility Study.
12. Hao X, Huang D, Wang Z, Zhang J, Liu H, Lu Y. Study on the safety and effectiveness of drug-coated balloons in patients with acute myocardial infarction.
13. Leone PP, Oliva A, Regazzoli D, et al. Immediate and follow-up outcomes of drug-coated balloon angioplasty in de novo long lesions on large coronary arteries.
14. Tartaglia F, Gitto M, Leone PP, et al. Validation of complex PCI criteria in drug-coated balloon angioplasty.
15. Leone PP, Gitto M, Gao C, Sanz Sánchez J, Latib A, Colombo A. Rethinking coronary artery metal implants.
16. Leone PP, Testa L, Greco A, et al. Two-Year Clinical Outcomes in Female and Male Patients After Sirolimus-Coated Balloon Angioplasty for Coronary Artery Disease.
17. Gitto M, Leone PP, Gioia F, et al. Coronary Artery Dissection in Drug-Coated Balloon Angioplasty:Incidence, Predictors, and Clinical Outcomes.
18. Leone PP, Mangieri A, Regazzoli D, et al. Drug-Coated Balloon Angioplasty Guided by Postpercutaneous Coronary Intervention Pressure Gradient:The REDUCE-STENT Retrospective Registry.
19. Leone PP, Heang TM, Yan LC, et al. Two-year outcomes of sirolimus-coated balloon angiopla,sty for coronary artery disease:the EASTBOURNE Registry.
20. Leone PP, Calamita G, Gitto M, et al. Sirolimus- Versus Paclitaxel-Coated Balloons for Treatment of Coronary Artery Disease.










