ABSTRACT
Introduction and objectives: Manual thrombectomy (MT) during primary percutaneous coronary intervention (PCI) aims to reduce thrombus burden. Our study evaluates the outcomes and predictors of successful MT.
Methods: The Hunted registry is a retrospective, single-center cohort study including patients who underwent MT during PCI using the Hunter catheter from July 2020 through February 2022. MT success was defined as an angiographic reduction to a Thrombolysis in Myocardial Infarction (TIMI) thrombus grade of ≤ 2, with clinical follow-up for major adverse cardiovascular events.
Results: Among 750 patients with acute myocardial infarction who underwent PCI, 401 (53%) received MT. The mean age of treated patients was 62 years (80% men). MT was effective in 327 patients (81.55%). Predictors of successful MT included larger vessel diameter (P < .001), high thrombus burden (TIMI grade ≥ 4 flow; P < .001), and non-circumflex target vessels (P < .001). Device-related complications occurred in 17 patients (4.3%). At follow-up, major adverse events occurred in 8.98% of patients at 1 year and in 9.97% at 2 years.
Conclusions: In patients with ST-segment elevation myocardial infarction undergoing PCI, MT with the Hunter catheter in selected cases with high thrombus burden (TIMI grade ≥ 4 flow), non-circumflex target vessels, and vessel diameters > 2.5 mm, is a safe and effective technique with a low rate of complications.
Keywords: ST-segment elevation myocardial infarction. Percutaneous coronary intervention. Manual thrombectomy. Thrombus burden.
RESUMEN
Introducción y objetivos: La trombectomía manual (TM) en la intervención coronaria percutánea primaria (ICPp) intenta reducir la carga trombótica. Este estudio evalúa los resultados y los factores predictores de éxito de la TM.
Métodos: El registro Hunted es un estudio de cohortes retrospectivo, unicéntrico, de pacientes tratados con TM en ICPp utilizando el catéter Hunter, desde julio de 2020 hasta febrero de 2022. El éxito de la TM se definió como una disminución angiográfica a grado ≤ 2 en la escala Thrombolysis in Myocardial Infarction (TIMI), con seguimiento clínico de eventos cardiovasculares adversos mayores.
Resultados: De los 750 pacientes con infarto agudo de miocardio tratados con ICPp, en 401 (53%) se realizó TM. Los pacientes tratados tenían una edad media de 62 años y el 80% eran varones. La TM fue efectiva en 327 (81,55%) pacientes. Los predictores de TM efectiva fueron un mayor diámetro del vaso (p < 0,001), una alta carga de trombo (TIMI ≥ 4; p < 0,001) y un vaso diferente de la circunfleja (p < 0,001). Se presentaron complicaciones relacionadas con el dispositivo en 17 pacientes (4,3%). En el seguimiento, el 8,98% presentaron eventos mayores a 1 año y el 9,97% a 2 años.
Conclusiones: En los pacientes con infarto de miocardio con elevación del segmento ST sometidos a ICPp, la estrategia de TM con catéter Hunter, en casos seleccionados con alta carga trombótica (escala TIMI ≥ 4), otros vasos que no fueran la circunfleja y diámetros > 2,5 mm, es una técnica eficaz y segura con una baja tasa de complicaciones.
Palabras clave: Infarto de miocardio con elevación del segmento ST. Intervención coronaria percutánea primaria. Trombectomía manual. Carga trombótica.
Abbreviations
MACE: major adverse cardiovascular events. MT: manual thrombectomy. PCI: primary coronary intervention. STEMI: ST-segment elevation myocardial infarction. TIMI: Thrombolysis in Myocardial Infarction.
INTRODUCTION
In patients with ST-segment elevation myocardial infarction (STEMI), the treatment of choice is percutaneous coronary intervention (PCI) performed within the appropriate time window and by experienced operators. PCI has been shown to reduce mortality, reinfarction, and stroke compared with fibrinolysis.1 Among other factors, this benefit may be attributed to greater epicardial reperfusion and higher TIMI (Thrombolysis in Myocardial Infarction) flow grades and myocardial blush grades achieved with PCI in the culprit artery, all of which are known to influence survival.2,3
PCI have distinctive characteristics, including the presence of a high thrombus burden and performance in patients in a markedly thrombogenic state. To reduce the local thrombus burden in the culprit artery, manual thrombectomy (MT) has been widely used during PCI to reduce thrombus load, prevent distal embolization, and improve final myocardial perfusion.3,4 Despite its initial widespread adoption, routine use of MT in all patients undergoing PCI is no longer recommended, as randomized clinical trials have not demonstrated consistent clinical benefit.3-7
MT should be reserved for patients in whom it is most likely to provide benefit. To optimize the efficacy of PCI, the American8 and European9 clinical practice guidelines recommend MT in high-risk patients with a moderate-to-high thrombus burden who present with short ischemia times. Currently, however, there are no clearly defined criteria to precisely identify patients or thrombotic lesions that would derive the greatest benefit from MT.
The aim of our study was to evaluate the results of MT performed with the Hunter catheter (IHT–Iberhospitex SA, Barcelona, Spain), which has a high extraction capacity, in selected patients with STEMI undergoing PCI, and analyze the angiographic patterns associated with successful MT in our center.
METHODS
Study design and population
The Hunted registry is a single-center, observational, retrospective study. We included all patients diagnosed with STEMI who underwent PCI and in whom MT was performed using the Hunter thrombus aspiration catheter. This device was the first-choice catheter for MT in our center during the study period. The decision to perform MT was always left to the discretion of the operator performing the PCI, following homogeneous criteria among operators, subjectively based on angiographical evidence of a large angiographically visible thrombus. MT was not recommended in coronary vessels with a diameter < 2 mm or for the extraction of chronic thrombi or atherosclerotic plaques. The study period ranged from July 2020 through February 2022. Patients in whom MT was performed using a catheter other than the Hunter device were excluded.
The primary objective of the study was to evaluate the success of thrombus aspiration during PCI in patients with STEMI. Effective MT was defined as an angiographical reduction in thrombus burden, achieving a TIMI thrombus grade ≤ 2 (thrombus dimension < 50% of the vessel diameter). Moreover, angiographic factors associated with effective MT were assessed.
Secondary objectives included describing the clinical and angiographic characteristics of the patients and evaluating major adverse cardiovascular events (MACE) during hospitalization and follow-up.
MACE were defined as a composite endpoint of cardiovascular and noncardiovascular death, stroke, and acute myocardial infarction. Two follow-up time points were established at 1 and 2 years after PCI. Total ischemia time was defined as the interval, in minutes, between symptom onset and reperfusion, defined as passage of the intracoronary guidewire, in accordance with clinical practice guidelines.
Thrombus burden was graded according to the TIMI thrombus scale,10 which includes 5 grades: grade 1, possible thrombus; grade 2, thrombus dimension < 50% of the vessel diameter; grade 3, thrombus dimension 0.5 to 2.0 vessel diameters; grade 4, thrombus dimension > 2.0 vessel diameters; and grade 5, total vessel occlusion by thrombus. Grades 4 and 5 were considered high thrombus burden.
Successful PCI was defined as achievement of TIMI grade 3 flow with residual percent diameter stenosis < 20%, without device-related complications or intraoperative MACE. For study purposes, patients were categorized into 2 groups according to whether MT was effective or not. Furthermore, these groups were compared to identify angiographic parameters that could predict MT success.
Data for the variables included in the Hunted registry were collected using a dedicated electronic case report form. Retrospective angiographic analysis was performed exclusively by 3 operators. All measures were taken to ensure confidentiality and protection of patient health record information. The study protocol fully complied with international recommendations for clinical research outlined in the Declaration of Helsinki and was approved by the hospital Ethics and Research Committee.
Characteristics of the Hunter device and aspiration technique
The Hunter thrombus aspiration catheter is a 140 cm rapid-exchange aspiration catheter compatible with a 6-Fr guiding catheter. Its tip has a slightly conical, low-profile, atraumatic design. The effective distal aspiration area measures 0.95 mm2, and it can aspirate up to 1.92 mL per second, one of the highest capacities available. The distal segment is coated with a hydrophilic surface to facilitate device navigability.
The standard thrombectomy technique used in our center consisted of advancing the Hunter catheter to a segment proximal to the culprit lesion. Aspiration was always initiated proximal to the culprit lesion. The catheter was then slowly advanced across the lesion under continuous aspiration to reach the distal segment, while continuous filling of the syringe was observed. If filling stopped, the catheter was withdrawn until aspiration resumed or removed completely if aspiration could not be reestablished. Continuous aspiration until removal from the guiding catheter was mandatory, as was thorough subsequent flushing of the guiding catheter, to prevent embolization of residual thrombotic material.
All retrieved material from the catheter and aspiration syringe was subsequently filtered using the filters provided with the device packaging. The procedure was repeated as many times as deemed necessary by the operator until the desired reduction in thrombus burden was achieved.
Statistical analysis
Qualitative variables are expressed as frequencies and percentages, and the quantitative ones as mean and standard deviation when normally distributed, and as median and interquartile range when distribution was nonnormal.
Qualitative variables were compared using the chi-square test, with odds ratios (OR) and 95% confidence intervals (95%CI) calculated. Quantitative ones were compared using the Student t test or nonparametric tests, as appropriate.
In univariate analysis, each variable was individually assessed for its association with effective MT. Variables showing a statistically significant association were included in the multivariate analysis. Multiple regression models were used to control for potential confounders and determine the independent effect of each variable on the outcome.
Survival curves were analyzed using the Kaplan–Meier method, and survival-related parameters were evaluated using Cox proportional hazards analysis. A 2-sided P value < .05 was considered statistically significant.
Statistical analyses were performed using STATA version 15 (StataCorp, United States).
RESULTS
During the study period, a total of 750 PCI were performed in patients diagnosed with STEMI. MT using the Hunter catheter was performed in 401 patients (53.47%). The clinical characteristics of the patients, STEMI features, and PCI are shown in table 1.
Table 1. Clinical characteristics of patients and procedural variables
| Clinical characteristics | (n = 401) |
|---|---|
| Age, years | 62.38 ± 12.43 |
| Male sex | 319 (80) |
| Current/former smoker | 163 (40.65) / 35 (8.73) |
| Hypertension | 207 (51.62) |
| Dyslipidemia | 186 (46.38) |
| Diabetes mellitus | 86 (21.45) |
| Kidney failure | 7 (1.75) |
| Previous stroke | 16 (3.99) |
| Peripheral vascular disease | 8 (2.00) |
| Previous AMI | 48 (11.97) |
| Previous PCI | 50 (12.47) |
| Prior CABG | 5 (1.25) |
| Infarct location | |
| Anterior | 166 (41.50) |
| Inferior | 207 (51.75) |
| Lateral | 27 (6.75) |
| Killip-Kimball classification | |
| I | 338 (84.71) |
| II | 18 (4.51) |
| III | 8 (2.01) |
| IV | 35 (8.77) |
| Procedural variables | |
| Radial access | 385 (96.01) |
| No. of diseased vessels* | |
| 1 | 233 (58.10) |
| 2 | 111 (27.68) |
| 3 | 57 (14.21) |
| Infarct-related artery | |
| Right coronary artery | 183 (45.64) |
| Left anterior descending coronary artery | 166 (41.40) |
| Left circumflex artery | 48 (11.97) |
| Venous graft | 1 (0.25) |
| Left main coronary artery | 3 (0.75) |
| No. of stents implanted | |
| 0 | 34 (8.47) |
| 1 | 288 (71.82) |
| 2 | 60 (14.96) |
| 3 | 19 (4.74) |
| Drug-eluting stent (n = 367) | 362 (98.64) |
| Total ischemic time | |
| < 90 min | 43 (10.72) |
| 91-180 min | 167 (41.65) |
| 181-270 min | 82 (20.45) |
| 271-360 min | 42 (10.47) |
| > 360 min | 67 (16.71) |
|
AMI, acute myocardial infarction; CABG, coronary artery bypass grafting; PCI, percutaneous coronary intervention. |
|
Angiographic analysis of the culprit lesion and flow in the infarct-related artery is shown in table 2. Initial TIMI grade flow in the infarct-related artery, prior to intracoronary guidewire passage was 0 in 83% of cases. A high thrombus burden was observed in 87.5% of patients, corresponding to TIMI thrombus grades 4 or 5; 53.4% had grade 5 and 34.2% had grade 4. Only 50 patients (12.5%) had a TIMI grade < 4 flow, defined as a low thrombus burden.
Table 2. Angiographic analysis of patients treated with percutaneous coronary intervention and manual thrombectomy
| Angiographic variables | |
|---|---|
| Vessel diameter | 3.25 [3.00-3.50] |
| 2.0-2.5 mm | 61 (15.21) |
| 2.6-3.0 mm | 122 (30.42) |
| 3.1-3.5 mm | 124 (30.92) |
| 3.6-4.0 mm | 66 (16.46) |
| > 4.0 mm | 28 (6.98) |
| Lesion length, mm | 16 [15-20] |
| AHA/ACC lesion type | |
| B1 | 60 (14.96) |
| B2 | 161 (40.15) |
| C | 180 (44.89) |
| Thrombus burden grade (TIMI) | |
| 1 | 1 (0.25) |
| 2 | 5 (1.25) |
| 3 | 44 (10.97) |
| 4 | 137 (34.16) |
| 5 | 214 (53.37) |
| Pre-PCI IRA TIMI flow grade | |
| 0 | 332 (82.79) |
| 1 | 18 (4.49) |
| 2 | 24 (5.98) |
| 3 | 27 (6.74) |
| Post-PCI IRA TIMI flow grade | |
| 0 | 2 (0.50); |
| 1 | 3 (0.75); |
| 2 | 10 (2.49); |
| 3 | 386 (96.26) |
|
AHA/ACC, American Heart Association/American College of Cardiology; IRA, infarct-related artery; PCI, percutaneous coronary intervention; TIMI, Thrombolysis in Myocardial Infarction. |
|
According to the predefined criteria, effective MT was achieved in 327 of 401 patients (81.5%). Thrombectomy was considered ineffective in the 6 patients who had initial TIMI thrombus grades 1 and 2. Final post-PCI coronary flow was TIMI grade < 3 flow in 15 patients (3.74%). Overall, the PCI was successful in approximately 97% of cases. Device-related complications were recorded in 17 patients (4.24%): severe arrhythmias (ventricular fibrillation or ventricular tachycardia) occurring during reperfusion in 10 patients; severe no-reflow due to distal thrombus migration that could not be successfully treated in 4 patients; and coronary dissection after passage of the MT catheter, which was successfully treated with stenting in 3 patients. There were no cases of perioperative stroke due to migration of aspirated thrombus.
Comparative analysis of angiographic factors and ischemia time between patients with effective and noneffective MT is shown in table 3. MT was effective more frequently in patients with culprit coronary vessels > 3 mm in diameter (112 [34%] vs 12 mm [16%]; P < .001) and in those with a TIMI grade ≥ 4 thrombus burden (297 [91%] vs 54 [73%]; P < .001). Among the 61 patients with vessels < 2.5 mm, MT was ineffective in 36 (59.01%) vs 38 of 340 patients (11.2%) with vessels > 2.5 mm (P < .001). There were no statistically significant differences in ischemia time in relation to MT success.
Table 3. Comparison of angiographic and procedural characteristics between patients with effective and noneffective manual thrombectomy
| Procedural variables | Effective MT (n = 327) | Noneffective MT (n = 74) | P |
|---|---|---|---|
| Infarct-related artery | .008 | ||
| Right coronary artery | 153 (46.79) | 30 (40.54) | |
| Left anterior descending coronary artery | 140 (42.81) | 26 (35.14) | |
| Left circumflex artery | 30 (9.17) | 18 (24.32) | |
| Saphenous vein graft | 1 (0.31) | – | |
| Left main coronary artery | 3 (0.92) | – | |
| AHA/ACC classification of the culprit lesion | .004 | ||
| B1 | 51 (15.60) | 9 (12.16) | |
| B2 | 142 (43.42) | 19 (25.68) | |
| C | 134 (40.98) | 46 (62.16) | |
| Reference diameter of the culprit lesion | < .001 | ||
| 2.0 mm-2.5 mm | 25 (7.65) | 36 (48.69) | |
| 2.6 mm-3.0 mm | 101 (30.89) | 21 (28.38) | |
| 3.1 mm-3.5 mm | 112 (34.25) | 12 (16.22) | |
| 3.6 mm-4.0 mm | 64 (19.57) | 2 (2.70) | |
| > 4.0 mm | 25 (7.64) | 3 (4.10) | |
| Thrombus burden grade (TIMI) | < .001 | ||
| Low thrombus burden (TIMI < 4) | 30 (9.18) | 20 (27.03) | |
| High thrombus burden (TIMI ≥ 4) | 297 (90.82) | 54 (72.97) | |
| Pre-PCI TIMI grade flow | .031 | ||
| TIMI grade 0-1 flow | 291 (88.99) | 59 (79.73) | |
| TIMI grade 2-3 flow | 36 (11.01) | 15 (20.27) | |
| Post-PCI TIMI grade flow | .61 | ||
| TIMI grade 0-1 flow | 2 (0.61) | 3 (4.05) | |
| TIMI grade 2 flow | 8 (2.45) | 1 (1.35) | |
| TIMI grade 3 flow | 317 (96.94) | 70 (94.59) | |
| Time from symptom onset to reperfusion | .79 | ||
| ≤ 90 min | 37 (11.31) | 6 (8.11) | |
| 91-180 min | 139 (42.51) | 28 (37.84) | |
| 181-270 min | 68 (20.80) | 14 (18.92) | |
| 271-360 min | 33 (10.09) | 9 (12.16) | |
| > 360 min | 50 (15.29) | 17 (22.97) | |
| Final procedural success | 317 (96.94) | 70 (94.59) | .61 |
|
AHA/ACC, American Heart Association/American College of Cardiology; MT, manual thrombectomy; PCI, percutaneous coronary intervention; TIMI, Thrombolysis in Myocardial Infarction. |
|||
The 1- and 2-year follow-up was completed in 100% of included patients. MACE occurred in 32 patients (7.98%) at 30 days, 36 patients (8.98%) at 1 year, and 40 patients (9.97%) at 2 years (table 4). Kaplan–Meier curves for event-free survival during follow-up and cardiovascular death according to effective vs noneffective MT are shown in figure 1 and figure 2, respectively. Individual components of MACE at 1 year are shown in figure 3.
Table 4. Incidence rate of the composite endpoint of major adverse cardiovascular events during follow-up
| Cardiovascular events at follow-up | n (%) |
|---|---|
| At 30 days | 32 (7.98) |
| At 1 year | 36 (8.98) |
| At 2 years | 40 (9.97) |
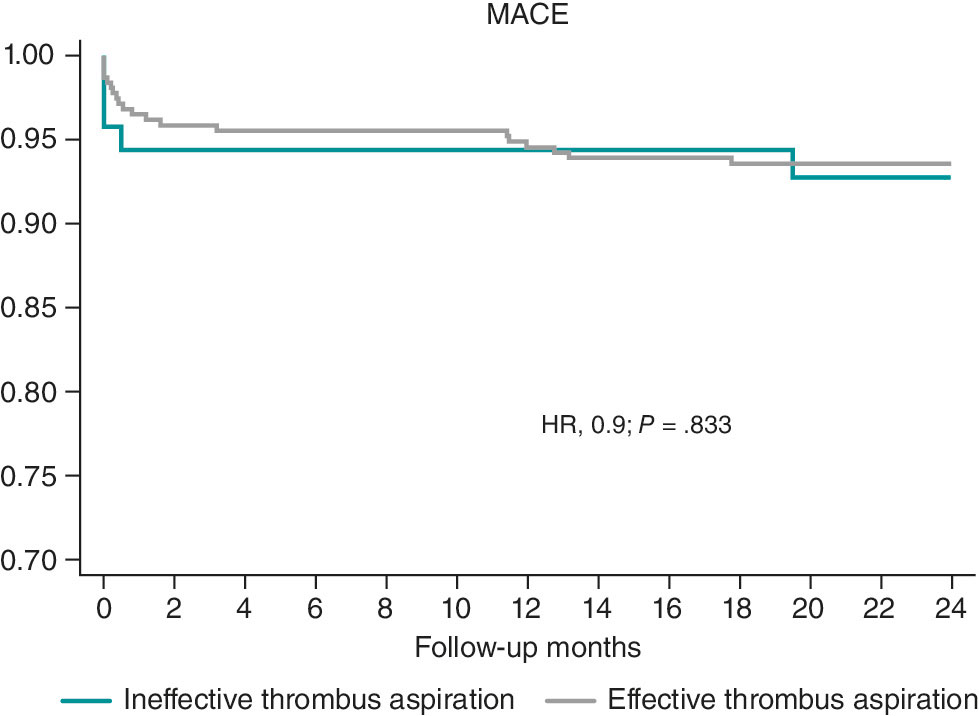
Figure 1. Kaplan–Meier curves for survival free from major adverse cardiovascular events (MACE). HR, hazard ratio.
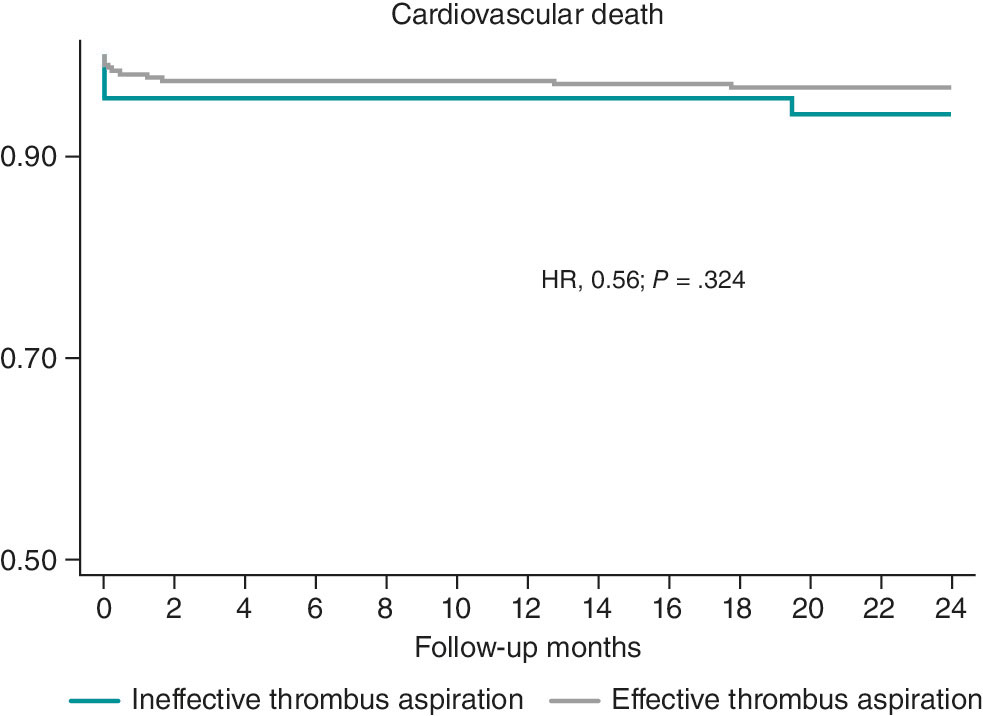
Figure 2. Kaplan–Meier survival curves for cardiovascular death. HR, hazard ratio.
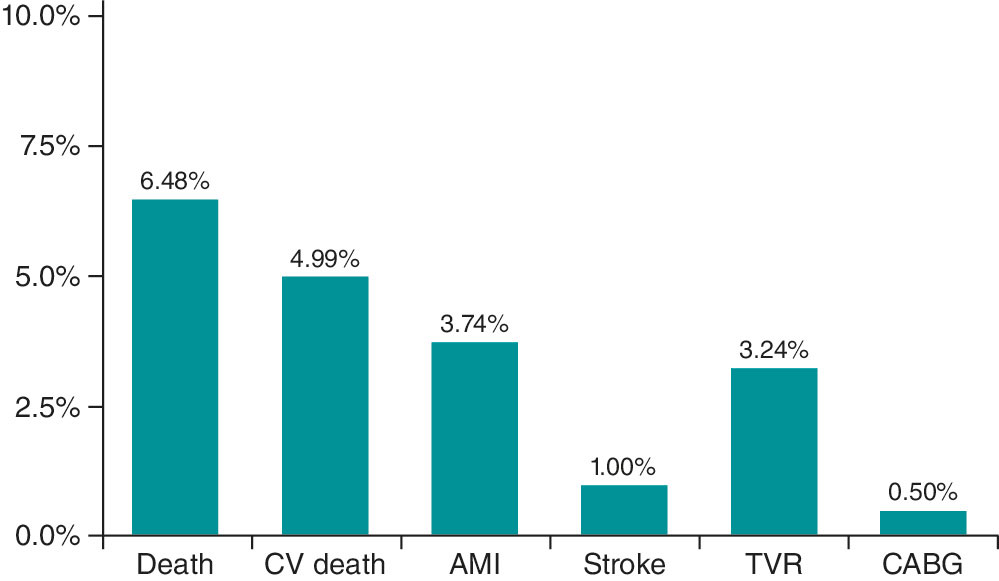
Figure 3. Individual components of major adverse cardiovascular events at the 1-year follow-up. AMI, acute myocardial infarction; CABG, coronary artery bypass grafting; CV, cardiovascular; TVR, target vessel revascularization.
DISCUSSION
In selected patients, MT using the Hunter catheter is a safe and effective strategy to reduce angiographically assessed thrombus burden during PCI.
Current clinical practice guidelines do not recommend routine MT during PCI but suggest considering it in patients with a high thrombus burden, based on individual assessment and operator experience.8,9 In our series, MT was performed in 53.5% of patients with STEMI treated with PCI, a higher proportion than reported in other countries.11-13 Only 12% of patients undergoing MT did not have a TIMI grade 4–5 thrombus burden on angiographic analysis.
In this selected population with high thrombus burden, 88% had TIMI grade ≥ 4 flow, which is similar to the 79% observed in the TOTAL trial,14 with favorable results in both cases. In contrast, only 33% of patients from the TASTE trial7 had a high thrombus burden.
A high thrombus burden appears to be a key determinant of achieving effective MT and may be associated with better clinical outcomes. In our cohort, although effective MT was achieved in 82% of cases, it was not significantly correlated with final procedural success (97% vs 95%; P = .67), likely due to the small sample size of the 2 groups. MT efficacy was higher in vessels with high thrombus burdens (TIMI grade ≥ 4 flow; P < .001), which is consistent with a meta-analysis showing less cardiovascular death in patients with STEMI undergoing PCI with MT in the high thrombus burden subgroup vs PCI alone (2.5% vs 3.2%; hazard ratio [HR], 0.81; 95%CI, 0.65–0.98; P = .03).15 These findings reinforce the concept that appropriate patient selection is crucial to benefit from MT. Moreover, the same meta-analysis reported a higher risk of stroke (0.9% vs 0.5% in the PCI-alone group),15 a complication that may be related to the TM technique used.
Strict adherence to proper technique is essential to minimize complications and maximize success. In our series, emphasis was placed on following a standardized and rigorous technique, as described in the Methods section, resulting in a low complication rate (4.3%). Many of these complications were not directly related to MT per se but rather to reperfusion, such as ventricular arrhythmias. MT-related stroke is a potential complication; in the TOTAL trial,16 the stroke rate was 0.7%, twice that observed in the PCI-alone group, whereas in the large real-world SCAAR registry, there was no increase in the incidence rate of stroke across the groups,17 which are findings more consistent with our results and possibly related to differences in MT technique.
To identify angiographic predictors of MT success, we compared the characteristics of patients with effective and noneffective MT. The former had significantly larger culprit vessel diameters; 48% of patients with noneffective MT had vessels measuring 2.5 mm. Although MT is generally discouraged in vessels < 2 mm, larger vessels may harbor greater thrombus burden and thus derive greater benefit from MT with the Hunter catheter, which has demonstrated higher in vitro aspiration capacity compared with other devices. Therefore, vessel size is a critical differentiating factor: in vessels < 2.5 mm, MT was ineffective in 59% of cases, a significantly higher proportion than the 11.2% of noneffective MT observed in larger vessels. The other major difference between groups was thrombus burden, as effective MT was achieved more frequently in patients with higher thrombus loads (TIMI grade ≥ 3 flow).15 Furthermore, this factor represents a major difference among randomized clinical trials, in which the proportion of patients with high thrombus burden varied substantially.15 More complex lesions, such as American Heart Association/American College of Cardiology type C lesions, those associated with calcification in addition to thrombus, long lesions, and left circumflex artery lesions were associated with higher rates of noneffective MT. These differences should be considered when selecting appropriate candidates for MT with the Hunter catheter, favoring patients with vessel diameters > 2.5 mm, abundant thrombus burden (TIMI grade ≥ 4 flow), and culprit arteries other than the left circumflex one.
Studies have shown that total ischemia time, which we believe may determine differences in thrombus composition,18 may influence the efficacy of thrombus aspiration.19 In our series, there were no differences between the effective and noneffective MT groups with respect to infarction duration.
When assessing whether effective MT impacted the outcome of the PCI, slightly different procedural success rates were observed: 97% for effective MT vs 95% for noneffective MT (P = .61). Statistical significance was not reached, possibly due to the small sample size. Only 4 patients experienced no-reflow that could not be resolved, with no differences across groups and without demonstrating that MT could prevent distal embolization, as suggested in former studies.17-19
Short- and long-term clinical outcomes in patients with STEMI who required MT were favorable, with a low 1-year cardiovascular death rate of 3.5%, comparable to that reported in randomized clinical trials. In the TASTE trial,7 the 30-day mortality rate was 2.4% in the MT group and 2.9% in the PCI-alone group (HR, 0.84; 95%CI, 0.70–1.01; P = .06). In the TAPAS trial,20 the 30-day all-cause mortality rate was 2.1% in the MT group vs 4.0% in the conventional PCI group, reaching statistical significance at the 1-year follow-up (P = .07). Large registries have reported mortality rates similar to those observed in our series, with 2.8% vs 3.0% in the Swedish registry21 and comparable findings in the Japanese registry.22 The overall mortality rate observed in a meta-analysis with aggregated data from published MT studies was 3.7%.15 When selecting patients with a high thrombus burden (TIMI grade ≥ 3 flow in the meta-analysis subgroup), the cardiovascular death rate was 2.5% (170 of 6872 patients) in the MT group vs 3.1% (205 of 6599 patients) in the PCI-alone group (HR, 0.8; 95%CI, 0.65–0.98; P = .03).15 Proper selection of this subgroup of patients with a high thrombus burden is, therefore, crucial to maximize the therapeutic benefit.
Limitations
As a single-center, observational, retrospective registry, this study has inherent limitations related to its design. First, because it reflects the experience of a single center—albeit with more than 15 years of experience in PCI—operator homogeneity may limit extrapolation of the results. The decision to perform MT was always left to the discretion of the operator, and no control group without MT was available for patient comparison. Because of the retrospective design of the analysis, we could not determine the cause of ineffective MT in all patients, which is why this variable could not be included in the analysis. This study should not be interpreted as an evaluation of thrombus aspiration in general, but rather as an assessment of outcomes in a selected population treated with the Hunter device; these selection criteria represent the primary contribution of this work to current scientific knowledge. The study did not incorporate systematic criteria to address sex- and gender-related variables during methodological development or result analysis. Although angiographic analysis was not performed by an independent core laboratory, it was conducted by 3 experienced analysts. In this analysis, MT success, procedural success, and baseline thrombus burden were defined using the TIMI scale.
CONCLUSIONS
In patients with STEMI undergoing PCI, selective use of MT with the Hunter catheter in cases with high thrombus burden (TIMI grade ≥ 4 flow), non-circumflex culprit vessels, and vessel diameters > 2.5 mm is a safe and effective strategy associated with a low complication rate. Further studies are needed to assess the impact of this strategy on PCI outcomes, MACE, and stroke.
FUNDING
This project was supported by IHT-Iberhospitex S.A. (Lliçà de Vall, Barcelona, Spain). As sponsor, the company collaborated in the study design but had no role in data collection, analysis, or interpretation. Manuscript preparation and the decision to submit for publication were entirely independent of the sponsor and performed by the research team.
ETHICAL CONSIDERATIONS
The study was approved by Hospital Universitari Germans Trias i Pujol Ethics Committee (Barcelona, Spain) (CEIC code: PI-22-281) and conducted in full compliance with the principles outlined in the Declaration of Helsinki. SAGER guidelines were not applied to address gender bias.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCE
No artificial intelligence tools were used in the preparation of this manuscript.
AUTHORS’ CONTRIBUTIONS
D.G. Borraz-Noriega: angiographic analysis, data review, and manuscript drafting. J.F. Andrés-Cordón: angiographic analysis, data review, and statistical analysis. E. Cañedo: data collection and clinical follow-up. F. Panchano-Castro: angiographic analysis and data review. M. Trichilo: data collection and clinical follow-up. V. Vilalta: data collection and critical manuscript review. O. Rodríguez-Leor: data collection and critical manuscript review. E. Fernández-Nofrerias: critical manuscript review. I. Santos-Pardo: critical manuscript review. X. Carrillo: study design, overall supervision, and manuscript drafting. All authors reviewed and approved the final version.
CONFLICTS OF INTEREST
None declared.
WHAT IS KNOWN ABOUT THIS TOPIC?
- Routine use of manual thrombectomy has not demonstrated clear benefit. Current clinical practice guidelines recommend individualized use in selected patients with high thrombus burden. Clear angiographic criteria for identifying patients most likely to benefit from thrombectomy are lacking.
WHAT DOES THIS STUDY ADD?
- The Hunted registry provides specific evidence on thrombectomy performed with the Hunter catheter during PCI.
- It identifies angiographic predictors of thrombectomy success (vessel diameter > 2.5 mm, TIMI ≥ 4 thrombus burden, non-circumflex coronary arteries).
- The Hunter catheter, with its larger effective aspiration area, along with proper technique, demonstrates a low complication rate and favorable clinical outcomes.
REFERENCES
1. Keeley EC, Boura JA, Grines CL, et al. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13-20.
2. Chesebro JH, Knatterud G, Roberts R, et al. Thrombolysis in Myocardial Infarction (TIMI) Trial, Phase I: A comparison between intravenous tissue plasminogen activator and intravenous streptokinase. Clinical findings through hospital discharge. Circulation. 1987;76:142-154.
3. Moens AL, Claeys MJ, Timmermans JP, et al. Myocardial ischemia/reperfusion-injury, a clinical view on a complex pathophysiological process. Int J Cardiol. 2005;100:179-190.
4. Bhindi R, Kajander OA, Jolly SS, et al. Culprit lesion thrombus burden after manual thrombectomy or percutaneous coronary intervention-alone in ST-segment elevation myocardial infarction: the OTC sub-study of the TOTAL trial. Eur Heart J. 2015;36:1892-1900.
5. Sim DS, Jeong MH, Ahn Y, et al. Korea Acute Myocardial Infarction Registry (KAMIR) Investigators. Manual thrombus aspiration during primary percutaneous coronary intervention: Impact of total ischemic time. J Cardiol. 2016;27:753-758.
6. Vlaar PJ, Svilaas T, van der Horst IC, et al. Cardiac death and reinfarction after 1 year in the Thrombus Aspiration during Percutaneous coronary intervention in Acute myocardial infarction Study (TAPAS): a 1-year follow-up study. Lancet. 2008;371:1915-1920.
7. Lagerqvist B, Fröbert O, Olivecrona GK, et al. Outcomes 1 Year after Thrombus Aspiration for Myocardial Infarction. N Engl J Med. 2014;371:1111-1120.
8. Levine GN, Bates ER, Blankenship JC, et al. ACC/AHA/SCAI Focused Update on Primary Percutaneous Coronary Intervention for Patients with ST-Elevation Myocardial Infarction: An Update of the 2011 ACCF/AHA/SCAI and the 2013 ACCF/AHA Guidelines. J Am Coll Cardiol. 2016;67:1235-1250.
9. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119-177.
10. Sianos G, Papafaklis MI, Serruys PW. Angiographic thrombus burden classification in patients with ST-segment elevation myocardial infarction treated with percutaneous coronary intervention. J Invasive Cardiol. 2010;22:6B-14B.
11. Freixa X, Jurado-Román A, Cid B, et al. Spanish cardiac catheterization and coronary intervention registry. 31st official report of the Interventional Cardiology Association of the Spanish Society of Cardiology (1990-2021). Rev Esp Cardiol. 2022;75:1040-1049.
12. Kimura K, Kimura T, Ishihisa M, et al. JCS 2018 Guideline on diagnosis and treatment of acute coronary syndrome. Circulation. 2019;83:1085-1196.
13. Qu Y-Y, Zhang X-G, Ju C-W, et al. Age-Related Utilization of Thrombus Aspiration in Patients with ST-Segment Elevation Myocardial Infarction: Findings From the Improving Care for Cardiovascular Disease in China Project. Front Cardiovasc Med. 2022;9:791007.
14. Svilaas T, Vlaar PJ, van der Horst IC, et al. Thrombus aspiration during primary percutaneous coronary intervention. N Engl J Med. 2008;358:557-567.
15. Jolly SS, James S, Džavík V, et al. Thrombus Aspiration in ST-Segment–Elevation Myocardial Infarction, An Individual Patient Meta-Analysis: Thrombectomy Trialists Collaboration. Circulation. 2017;135:143-152.
16. Jolly SS, Cairns JA, Yusuf S, et al. Randomized trial of primary PCI with or without routine manual thrombectomy. N Engl J Med. 2015;372:1389-1398.
17. Angeras O, Haraldsson I, Redfors B, et al. Impact of Thrombus Aspiration on Mortality, Stent Thrombosis, and Stroke in Patients with ST-Segment–Elevation Myocardial Infarction: A Report From the Swedish Coronary Angiography and Angioplasty Registry. J Am Heart Assoc. 2018;7:e007680.
18. Carol A, Bernet M, Curós A, et al. Thrombus age, clinical presentation, and reperfusion grade in myocardial infarction. Cardiovasc Pathol. 2014;23:126-130.
19. Sim DS, Jeong MH, Ahn Y, et al. Manual thrombus aspiration during primary percutaneous coronary intervention: Impact of total ischemic time. J Cardiol. 2017;69:428-435.
20. Vlaar PJ, Svilaas T, van der Horst IC, et al. Cardiac death and reinfarction after 1 year in the Thrombus Aspiration during Percutaneous coronary intervention in Acute myocardial infarction Study (TAPAS): a 1-year follow-up study. Lancet. 2008;371:1915-1920.
21. Fröbert, O, Lagerqvist B, Olivecrona GK, et al. Thrombus aspiration during ST-segment elevation myocardial infarction. N Engl J Med. 2013;369:1587-1597.
22. Inohara T, Kohsaka S, Yamaji K, et al. Use of Thrombus Aspiration for Patients with Acute Coronary Syndrome: Insights from the Nationwide J-PCI Registry. J Am Heart Assoc. 2022;11:e025728.










