To the Editor,
Transradial access has been popularized in percutaneous coronary interventions (PCI). However, the percutaneous management of chronic total coronary occlusions (CTO) is still predominantly via transfemoral access. This study assessed the efficacy and safety profile of a transradial access strategy in a PCI on a CTO and its impact on hospital stay.
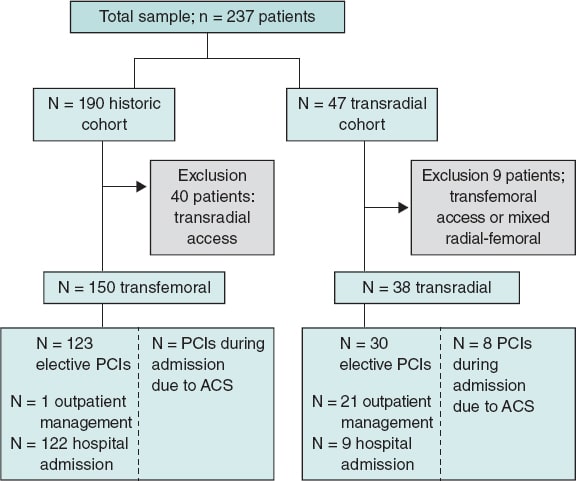
A total of 237 consecutive patients treated with PCI on their CTO were included in a single-center registry that compared the results of 2 vascular access strategies used over 2 consecutive periods of time: transfemoral between May 2013 and October 2018, and transradial from November 2018. A total of 40 patients were excluded from the analysis of the transfemoral strategy via transradial access and 9 were excluded from the transradial strategy via transfemoral or mixed radial-femoral access (figure 1). The Hospital Universitario de Salamanca clinical research ethics committee approved the study protocol and obtained the patients’ informed consent.
Figure 1. Flow chart of the patients included in the study. ACS, acute coronary syndrome; PCI, percutaneous coronary intervention.
The patients who not have any PCI related complications remained in observation at the cardiology day hospital for, at least, 6 to 8 hours. Those who remained asymptomatic and without alterations on their ECGs were discharged from the hospital the same day with outpatient control of their renal function between 48 and 72 hours after the procedure.
In patients hospitalized with acute coronary syndrome, the PCI on the CTO was delayed after completing target and other lesion revascularization with revascularization criteria. In patients treated with multiple catheterization attempts on the CTO, the characteristics of the latest procedure were analyzed. The advanced techniques used were rotablation, re-entry devices, and the CART and CART-REVERSE techniques.
Technical success was defined as the successful recanalization of the CTO with residual stenosis < 50% and TIMI (Thrombolysis in Myocardial Infarction) grade 3 flow. Procedural technical success was defined as the lack of in-hospital mayor adverse cardiovascular events: overall mortality, stroke, acute myocardial infarction, unstable angina or new revascularization. Periprocedural complications included coronary dissections and perforations, pericardial effusion, tamponade, and cardiogenic shock. In-hospital complications included contrast-induced nephropathy, vascular complications, and in-hospital mayor adverse cardiovascular events according to the guidelines. Also, mayor adverse cardiovascular events at the 30-day follow-up were registered.
To adjust the rate of technical success and total in-hospital complications due to the baseline and procedural differences seen between the patients of both strategies, a multivariate binary logistic regression analysis was conducted including variables with P values < .10 in the univariate analysis.
The results of 150 patients treated with PCI on a CTO via transfemoral access were compared to those of 38 patients treated via transradial access. Table 1 shows the patients’ baseline characteristics, procedural and event-driven data at the follow-up. No significant differences were seen on the baseline characteristic including the score obtained in the J-Chronic Total Occlusion scale.
Table 1Baseline characteristics of the patients, and procedural and event characteristics at the follow-up
| Transfemoral strategy (N = 150) | Transradial strategy (N = 38) | Total (N = 188) | P | |
|---|---|---|---|---|
| Baseline clinical and angiographic characteristics | ||||
| Age (years) | 66.8 ± 11.5 | 64.2 ± 11.1 | 66.3 ± 11.4 | .209 |
| Sex, male (N, %) | 131 (87.3) | 29 (76.3) | 160 (85.1) | .088 |
| Arterial hypertension (N, %) | 97 (68.3) | 29 (76.3) | 126 (70) | .339 |
| Diabetes mellitus (N, %) | 55 (36.7) | 14 (36.8) | 69 (36.7) | .984 |
| Dyslipidemia (N, %) | 97 (64.7) | 25 (65.8) | 122 (64.9) | .387 |
| Chronic kidney disease (N, %) | 20 (13.3) | 5 (13.2) | 25 (13.3) | .501 |
| Peripheral arteriopathy (N, %) | 26 (18.8) | 3 (8.3) | 29 (16.7) | .207 |
| LVEF (%) | 51.1 ± 13.1 | 54.1 ± 10.4 | 51.7 ± 12.7 | .139 |
| Previous coronary surgery (N, %) | 19 (12.7) | 2 (5.6) | 21 (11.3) | .377 |
| Anatomical SYNTAX score | 23.1 ± 11.5 | 22.3 ± 10.6 | 22.8 ± 11.1 | .744 |
| > 1 CTO | 25 (16.7) | 8 (21.1) | 33 (17.6) | .526 |
| Location of the CTO (N, %) | .051 | |||
| LAD | 48 (32) | 6 (15.8) | 54 (28.7) | |
| RCA | 87 (58) | 24 (63.2) | 111 (59) | |
| LCX | 15 (10) | 8 (21.1) | 23 (12.2) | |
| Previous failed PCI on CTO (N, %) | 18 (12) | 4 (10.5) | 22 (11.7) | .801 |
| J-CTO scale | 2.7 ± 0.9 | 2.5 ± 1.1 | 2.6 ± 1.0 | .466 |
| J-CTO scale > 2 (N, %) | 41 (54.7) | 18 (64.3) | 59 (57.3) | .380 |
| Characteristics of the angioplasty procedure on the CTO | ||||
| Contralateral injection (N, %) | 129 (86) | 27 (71.1) | 156 (83) | .029 |
| CTO access route (N, %) | ||||
| Antegrade | 133 (73.5) | 30 (63.8) | 163 (71.5) | .142 |
| Retrograde | 17 (9.4) | 3 (6.4) | 20 (8.8) | |
| Hybrid | 31 (17.1) | 14 (29.8) | 45 (19.7) | |
| Antegrade guide catheter (Fr) | 6.3 ± 0.5 | 6.0 ± 0.1 | 6.3 ± 0.5 | < .001 |
| Retrograde guide catheter (Fr) | 6.1 ± 0.5 | 5.9 ± 0.3 | 6.1 ± 0.4 | .002 |
| IVUS (N, %) | 8 (6.2) | 1 (2.7) | 9 (5.4) | .685 |
| PCI-CTO advanced techniques (N, %) | 36 (24) | 10 (26.3) | 46 (24.5) | .767 |
| Drug-eluting stent (N, %) | 128 (97.7) | 33 (100) | 161 (98.2) | .380 |
| Stent total length (mm) | 83.5 ± 36.5 | 82.5 ± 33.7 | 83.3 ± 35.8 | .884 |
| Contrast volume (mL) | 396.6 ± 229.7 | 280.9 ± 146.4 | 373.6 ± 220.3 | < .001 |
| Fluoroscopy time (min) | 47.0 ± 45.1 | 43.8 ± 31.9 | 46.4 ± 42.9 | .711 |
| Radiation–Kerma (Gy) | 3.5 ± 2.9 | 3.4 ± 2.9 | 3.5 ± 2.9 | .919 |
| Technical success (N, %) | 129 (86.6) | 33 (86.8) | 162 (86.6) | .893 |
| Procedural success (N, %) | 107 (71.3) | 29 (76.3) | 136 (72.3) | .540 |
| Outpatient PCI (N, %) | 1 (0.7) | 21 (55.3) | 22 (11.7) | < .001 |
| Outpatient elective PCI (N, %) | 1 (0.8) | 21 (70) | 22 (14.4) | < .001 |
| Hospital stay (days) | 3.4 ± 0.4 | 1.4 ± 0.3 | 2.0 ± 3.1 | < .001 |
| Periprocedural complications and events at the follow-up | ||||
| Total in-hospital complications (N, %) | 23 (15.3) | 5 (13.2) | 28 (14.9) | .737 |
| Periprocedural complications (N, %) | ||||
| Coronary perforations | 4 (2.7) | 2 (5.3) | 6 (3.2) | .416 |
| Coronary dissections | 1 (1.6) | 1 (2.6) | 2 (1.1) | .364 |
| Cardiac tamponade | 1 (1.6) | 2 (6.5) | 3 (3.3) | .262 |
| Cardiogenic shock | 5 (3.3) | 0 | 5 (2.7) | .585 |
| In-hospital complications (N, %) | ||||
| Postprocedural AMI | 5 (3.3) | 1 (2.6) | 6 (3.2) | .767 |
| Stroke | 1 (0.7) | 0 | 1 (0.5) | .599 |
| Contrast-induced nephropathy | 2 (1.3) | 0 | 2 (1.1) | .456 |
| Vascular complications: | 9 (6.0) | 0 | 9 (4.8) | .122 |
| Minor (N, %) | 4 (2.7) | 0 | 4 (2.1) | .309 |
| Major (N, %) | 5 (3.3) | 0 | 5 (2.7) | .254 |
| Cardiac surgery | 1 (0.7) | 0 | 1 (0.5) | .599 |
| Pericardial effusion | 4 (2.7) | 1 (2.6) | 5 (2.7) | .707 |
| In-hospital mortality | 0 | 0 | 0 | ND |
| In-hospital MACE | 6 (4) | 1 (2.6) | 7 (3.7) | .691 |
| Events at the 30-day follow-up | .292 | |||
| Early stent thrombosis (N, %) | 0 | 1 (2.6) | 1 (0.5) | |
| Unstable angina (N, %) | 1 (0.7) | 0 | 1 (0.5) | |
| MACE at the 30-day follow-up | 7 (4.7) | 2 (5.3) | 9 (4.8) | .311 |
|
AMI, acute myocardial infarction; CTO, chronic total coronary occlusion; IVUS, intravascular ultrasound; LAD, left anterior descending coronary artery; LCx, left circumflex artery; LVEF, left ventricular ejection fraction; MACE, major adverse cardiovascular events; NA, not available; PCI, percutaneous coronary intervention; RCA, right coronary artery. |
||||
The PCI on the CTO was successful in 162 patients (86.2%) from the overall sample, and in 50 patients (84.7%) with J-Chronic Total Occlusion scale scores > 2 without differences between both strategies. Transfemoral access was the most commonly used bilateral vascular access and large-caliber guide catheters and a larger volume of contrast were used without any other differences reported in relation to the intervention.
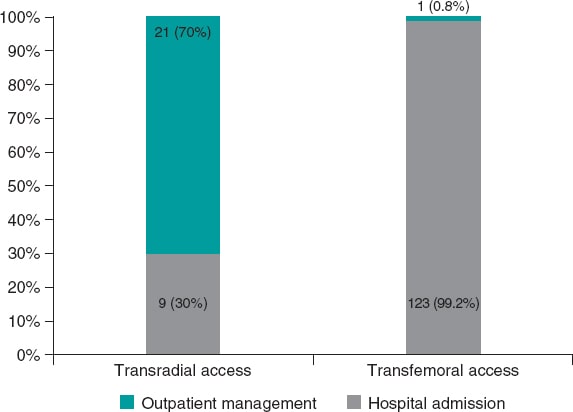
The percentage of outpatient procedures performed was higher in the transradial strategy (up to 70% of the procedures performed via transradial access in hospitalizations outside the non-acute coronary syndrome setting (figure 2). Consequently, hospital stay was shorter in patients treated via transradial access. No differences were seen in periprocedural or in-hospital complications or in the 30-day follow-up.
Figure 2. Outpatient management in select patients treated with percutaneous coronary intervention on chronic total coronary occlusions based on the vascular access used.
In the multivariate analysis, previous surgical revascularizations (odds ratio [OR] = 0.12; 95% confidence interval [95%CI], 0.02-0.87; P = .036) were the only independent predictive factor associated with lower chances of technical success in the PCI on the CTO. The past medical history of diabetes (OR = 5.71; 95%CI, 1.65-17.79; P = .006), surgical revascularization (OR = 3.96; 95%CI, 1.1513.66; P = .029) or previous failed PCI on the CTO (OR = 4.76; 95%CI, 1.46-15.51; P = .018) were independent predictors of a higher risk of total in-hospital complications. No differences were seen in the chances of technical success or risk of complications based on the access route.
Recent studies have shown that transradial access in PCIs performed on CTOs reduces bleeding and vascular complications. Also, that efficacy is similar to the one reached via transfemoral access1. However, in most of these studies, transradial access was spared for the management of less complex CTOs.
In our study, the PCIs performed on CTOs via transradial access were safe even in outpatients without episodes of contrast-induced nephropathy or late cardiac tamponade. None of the study patients developed late tamponade beyond the first 6 to 8 hours after the procedure. Similarly, transradial access reached a high rate of success comparable to the one reached via transfemoral access even in more complex lesions and with significantly shorter hospital stays. Outpatient treatment was possible in over two thirds of the patients with scheduled procedures, which is consistent with the 63.6% reported by a recent study on complex lesions where CTOs were < 5% of the total lesions.2
The impact of a transradial access strategy on hospital stay after a PCI on a CTO has not been studied yet. To this day, the factors associated with outpatient management after performing a PCI on a CTO have only been analyzed in 1 registry.3 According to this registry, same-day hospital discharges were possible in 41.6% of the patients probably thanks to the use of transfemoral access in most of the cases (90%).
In conclusion, our study provides additional evidence in favor of using transradial access to perform PCIs on CTOs as a safe and effective option to reduce the number and length of hospital stays, which may improve the management of health resources significantly.
FUNDING
No funding was received for this work.
AUTHORS' CONTRIBUTIONS
B. Trejo-Velasco: Design of the study. Collection of information. Statistical analysis and writing of the original manuscript. Graphic design and tables. A. Diego-Nieto: Conception original idea and design of the study. Methodology and statistical analysis. Original manuscript co-writing, manuscript review and correction, and project supervision. J. C. Núñez: Data collection. Methodology and research. Manuscript review. J. Herrero-Garibi: Data collection. Methodology and research. Manuscript review. I. Cruz-González: Design of the study. Data collection. Methodology and research. Review of the manuscript and supervision of the project. J. Martín-Moreiras: Conception, original idea and design of the study. Methodology and data collection. Revision and correction of the manuscript and supervision of the project.
CONFLICTS OF INTEREST
There are no conflicts of interest.
REFERENCES
1. Megaly M, Karatasakis A, Abraham B, et al. Radial Versus Femoral Access in Chronic Total Occlusion Percutaneous Coronary Intervention. A Systematic Review and Meta-Analysis. Circ Cardiovasc Interv. 2019. https://doi.org/10.1161/CIRCINTERVENTIONS.118.007778.
2. Córdoba-Soriano JG, Rivera-Juárez A, Gutiérrez-Díez A, et al. The Feasibility and Safety of Ambulatory Percutaneous Coronary Interventions in Complex Lesions. Cardiovasc Revasc Med. 2019;20:875-882.
3. Sawant AC, Seibolt L, Distler E, et al. Safety and feasibility of same-day discharge after percutaneous coronary intervention for chronic total occlusion:a single center observational cohort study. Coron Artery Dis. 2019;30:549-550.