A 77-year-old man with a history of severe in-stent restenosis (ISR) of the left anterior descending (LAD) and left circumflex (LCx) arteries, treated with coronary artery bypass grafting 4 years earlier, presented with acute chest pain, right bundle branch block, and anterolateral ST-segment elevation (figure 1A). His blood pressure was 90/60 mmHg, and echocardiography demonstrated severely impaired left ventricular function without mechanical complications.
Emergency angiography revealed a chronic total occlusion in the LAD (figure 1B, arrow), severe ISR in the LCx (figure 1C, arrow), and an occluded native right posterior descending artery. The graft to this artery was patent but diseased, and there was no antegrade flow in the left internal mammary artery (LIMA)–LAD graft (figure 1D; video 1). An intra-aortic balloon pump was inserted, and the LIMA–LAD graft was successfully wired with a workhorse guidewire. IVUS of the proximal to mid LIMA confirmed intraluminal position without evidence of dissection or graft disease (figure 1E).
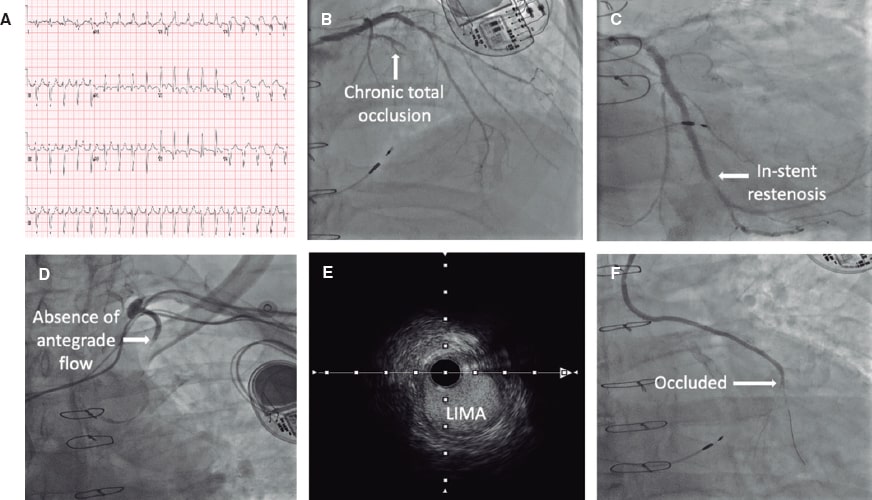
Figure 1.
Afterwards, a Thrombuster II (Kaneka Corp., Japan) aspiration device was advanced into the mid LIMA. Contrast injection revealed an occlusion at the LIMA–LAD anastomosis (figure 1F, arrow). Although thrombectomy restored flow, severe stenosis persisted at the anastomosis site. Balloon angioplasty was performed, followed by the deployment of a 2.0 mm × 30 mm Prevail (Medtronic, United States) drug-coated balloon (DCB) across the graft and native LAD (figure 2A, arrow). Final angiography demonstrated excellent runoff (figure 2B; video 2), ST-segment resolution, and hemodynamic improvement.
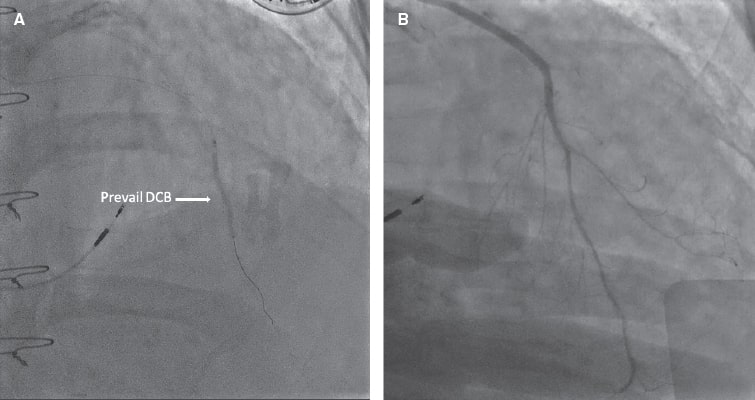
Figure 2.
Although LIMA grafts have excellent long-term patency, acute occlusion is rare but serious. In this case, acute native LAD plaque rupture distal to the LIMA anastomosis was a likely cause. Thrombectomy with DCB angioplasty enabled a scaffold-free revascularization strategy while preserving the integrity of the graft, illustrating a novel approach to acute LIMA–LAD graft occlusion.
FUNDING
None declared.
ETHICAL CONSIDERATIONS
Because this is an isolated case report, most SAGER guidelines recommendations are not applicable. The patient’s age and gender have been specified. As this is a case report rather than a research study, no further considerations were required. Informed consent for diagnostic tests and for publication of the case was obtained.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCE
Artificial intelligence was not used.
AUTHORS’ CONTRIBUTIONS
S. C. H. Wong and B. V. Khialani drafted the initial version of the manuscript and selected and edited the images that would later be used. All authors collaborated in the manuscript critical review and approved its final version.
CONFLICTS OF INTEREST
None declared.
SUPPLEMENTARY DATA
Vídeo 1. Chun Hui Wong S. DOI: 10.24875/RECICE.M25000545
Vídeo 2. Chun Hui Wong S. DOI: 10.24875/RECICE.M25000545










