To the Editor,
Advanced heart failure (HF) complicated by secondary mitral regurgitation is associated with a poor prognosis, and heart transplantation is the standard of care; however, donor scarcity requires bridge strategies.1 The MitraBridge registry2 evaluated the impact of transcatheter edge-to-edge repair (TEER) in patients considered for transplantation; however, its retrospective design and substantial loss to follow-up limit the strength of its conclusions.
The primary endpoint of our study was to assess the impact of TEER on mortality and the composite endpoint of death, need for heart transplantation or emergency left ventricular assist device placement, and index HF-related hospitalization in a cohort of patients with advanced HF and significant secondary mitral regurgitation who were evaluated for transplantation. The secondary endpoint was to compare the rate of HF-related hospitalizations before and after TEER.
We conducted a retrospective analysis of a single-center, prospective observational registry including all patients treated with TEER at a tertiary referral center in Spain. The Córdoba Research Ethics Committee approved the study, and all patients gave their prior written informed consent. We selected patients with advanced HF (defined as New York Heart Association [NYHA] functional class ≥ II, left ventricular ejection fraction ≤ 35%, at least 1 HF-related hospitalization, and age ≤ 70 years) who were assessed as potential candidates for listing on the transplant waiting list.
Kaplan–Meier curves were used to estimate overall and event-free survival, and the rate of HF-related rehospitalization was calculated per 100 patient-years.
A total of 191 patients underwent TEER from 2011 through 2023, 38 of whom met the inclusion criteria, with follow-up available until December 2024 (median, 35 months; 25th-75th percentile: 8–70). The mean age was 56 ± 12 years, and the rate of procedural success, 92%. Baseline, procedural, and follow-up characteristics are shown in table 1. A total of 17 patients died and 26 experienced the composite event during follow-up. At 24 months, the overall survival rate was 76.5%; and the event-free survival rate, 48% (figure 1). The rate of HF-related hospitalization decreased significantly from 108 to 33 per 100 patient-years (rate ratio, 0.31; 95%CI, 0.21–0.45; P < .0005) (figure 1). At last follow-up, 15 patients (40%) had died without transplantation and 5 (13%) had undergone transplantation (2 died). Of the remaining patients, 8 (21%) stayed on the waiting list, and 10 (26%) were not listed—4 due to contraindications and 6 due to clinical improvement (figure 1).
Table 1. Baseline and procedural characteristics, and follow-up events of the patients in the series
| Variables | Values |
|---|---|
| Clinical characteristics | |
| Age (years) | 56 ± 12 |
| Female sex | 7 (19) |
| Smoker | 11 (29) |
| Diabetes | 17 (45) |
| Dyslipidemia | 20 (52.6) |
| Hypertension | 14 (37) |
| Peripheral arterial disease | 2 (5) |
| Stroke | 6 (16) |
| Atrial fibrillation | 20 (52.6) |
| Anemia | 8 (21.1) |
| Chronic obstructive pulmonary disease | 7 (18.4) |
| History of cancer | 2 (5) |
| Previous percutaneous coronary intervention | 14 (37) |
| Previous coronary artery bypass graft | 4 (11) |
| ICD/CRT | 17 (45) |
| Ischemic mitral regurgitation | 18 (47) |
| STS score (points) | 2.4 [1.4–4.2] |
| NYHA functional class III–IV | 29 (76.3) |
| Number of HF-related hospitalizations per patient | 1.5 [1–3] |
| Body mass index (kg/m2) | 27 ± 4 |
| Analytical characteristics | |
| Hemoglobin (g/dL) | 14 ± 2 |
| Leukocytes/mm3 | 7551 ± 2138 |
| Platelets/mm3 | 187 833 ± 59 138 |
| Creatinine (mg/dL) | 1.2 ± 0.6 |
| eGFR < 60 mL/min | 13 (35) |
| NT-proBNP (pg/mL) | 3200 [1241–5831] |
| Echocardiographic characteristics | |
| LV ejection fraction (%) | 27 [22–31] |
| LV diastolic diameter (mm) | 71 ± 8.5 |
| LV systolic diameter (mm) | 59 ± 10 |
| Left atrium (mL/m2) | 61 [44–89] |
| Degree of mitral regurgitation | |
| Moderate–severe (III) | 2 (5.3) |
| Severe (IV) | 36 (94.7) |
| TAPSE (mm) | 16 ± 3.6 |
| Degree of tricuspid regurgitation | 1 [1–2] |
| Pulmonary artery systolic pressure (mmHg) | 47.5 [35–60] |
| Optimal medical therapy | |
| ACEI, ARB-II or ARNI | 38 (100) |
| Mineralocorticoid antagonists | 34 (92) |
| SGLT2i | 11 (29) |
| Beta-blockers | 37 (97.4) |
| High-dose diuretics | 23 (69.5) |
| Anticoagulation | 34 (92) |
| Procedural characteristics | |
| Procedural success | 35 (92) |
| Residual mitral regurgitation | |
| Mild (I) | 18 (47) |
| Mild-moderate (II) | 16 (42) |
| Moderate-severe (III) | 3 (7.9) |
| Severe (IV) | 1 (2.6) |
| Number of clips | |
| 1 | 16 (42) |
| 2 | 19 (50) |
| ≥ 3 | 3 (8) |
| Procedural time (min) | 120 [66–186] |
| Type of clip (MitraClip) | 38 (100) |
| Complications | 1 (3) |
| Follow-up | |
| Events at 24 months | |
| Patients with HF-related hospitalization | 19 (50) |
| Heart transplant | 5 (13.2) |
| Left ventricular assist device | 2 (5.3) |
| Death | 9 (23.7) |
| Events at the end of follow-up | |
| Patients with HF-related hospitalizTION | 24 (63.2) |
| Heart transplant | 5 (13.2) |
| Left ventricular assist device | 3 (7.9) |
| Death | 17 (44.7) |
|
ARB, angiotensin II receptor blockers; ARNI, angiotensin receptor–neprilysin inhibitors; ACEI, angiotensin-converting enzyme inhibitors; CRT, cardiac resynchronization therapy; eGFR, estimated glomerular filtration rate; HF, heart failure; ICD, implantable cardioverter-defibrillator; LV, left ventricle; NT-proBNP, N-terminal pro-B-type natriuretic peptide; NYHA, New York Heart Association; SGLT2i, sodium–glucose cotransporter type 2 inhibitors; TAPSE, tricuspid annular plane systolic excursion. Data express absolute values and percentages (categorical variables), and mean ± standard deviation or median [25th–75th percentiles] (continuous variables). |
|
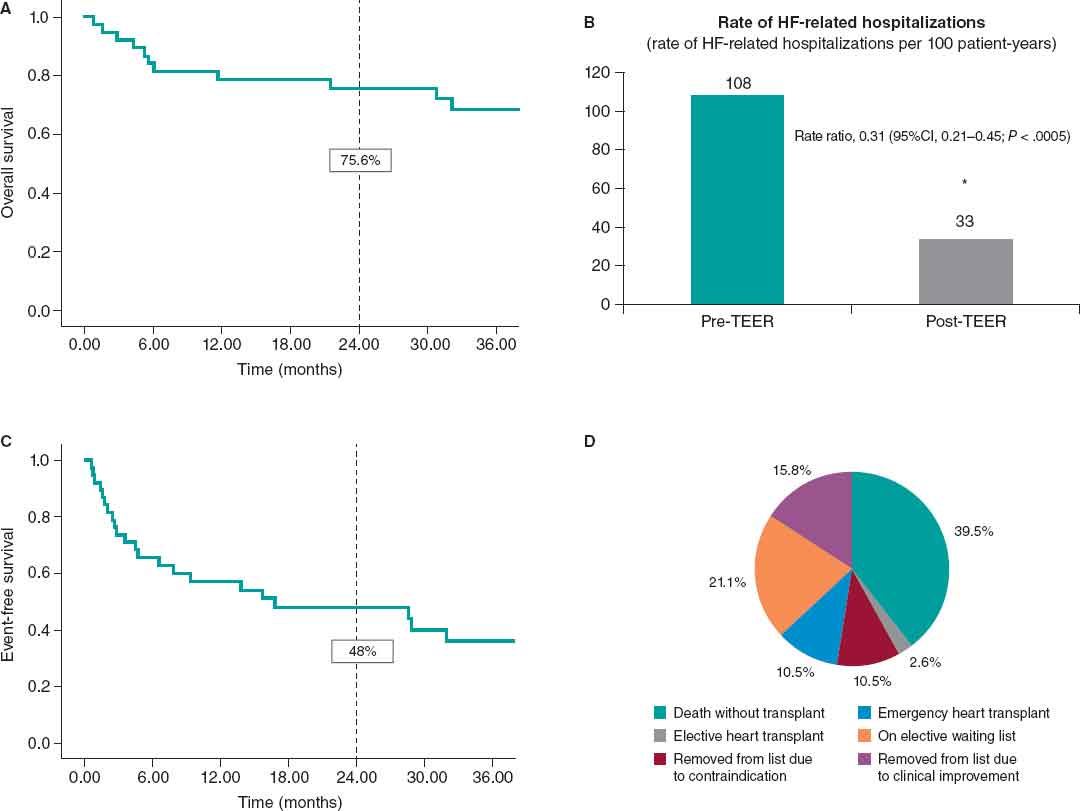
Figure 1. Overall survival (A) and event-free survival rates (C); pre- and postoperative rate of HF-related hospitalizations (B); and final status of patients in the series (D). 95%CI; 95% confidence interval; TEER, transcatheter edge-to-edge repair.
Our findings support the role of TEER as a bridge-to-transplant strategy in selected patients with fewer HF-related hospitalizations. Compared with the MitraBridge registry,2 clinical and echocardiographic profiles were similar, although fewer patients from our study were in NYHA functional class III–IV (76.3% vs 93%). In the MitraBridge registry,3 at 2 years, 27 of the 126 patients with complete follow-up had died, yielding an overall survival rate of 78.6%, which is similar to the 2-year survival rate observed in our study (75.6%), although that registry had a high loss-to-follow-up rate (17.6%). Such mortality figures are notable considering that, based on other studies,4 the 1-year overall survival rate in patients with advanced HF is approximately 75%. In our study, the event-free survival rate was very similar to that of the MitraBridge registry at 2 years3 (48% vs 47%) and that of other registries,4 supporting the reproducibility of the strategy. The reduction in HF-related hospitalizations observed after TEER was even greater in our study than in the MitraBridge registry3 (rate ratio, 0.31 vs 0.37), which may relate to the higher procedural success and lower proportion of patients in NYHA functional class III–IV in our series. Of note, 16% of our patients could be removed from the transplant waiting list because of clinical improvement, which is slightly lower than the 23% reported in MitraBridge,3 but without loss to follow-up in our series. However, the number of patients who died or required transplantation or ventricular assist device placement was substantial in the 2 series, underscoring the importance of proper patient selection.
As a strength, although 3 Spanish centers participated in the MitraBridge registry,2,3 this is, to our knowledge, the first study conducted in Spain to replicate its findings with consecutive patient inclusion and no loss to follow-up. These results support the use of TEER in patients with advanced HF not only in transplant centers but also in all centers equipped to perform the technique, as part of treatment optimization.
The main limitations of the study are its observational and retrospective design, absence of a control group, single-center nature, and small sample size.
In conclusion, TEER as a bridge to heart transplantation in patients with advanced HF and significant secondary mitral regurgitation is safe and effective, with a 2-year survival rate of 75%. Similarly, it significantly reduces HF-related hospitalizations and allows a meaningful proportion of patients to be removed from the transplant waiting list.
Randomized clinical trials are needed to confirm our findings and improve candidate selection.
DATA AVAILABILITY
Although the data supporting the findings of this study are not publicly available because of sensitivity concerns, they may be provided upon reasonable request to the corresponding author.
FUNDING
None declared.
ETHICAL CONSIDERATIONS
The study complied with the recommendations outlined in the Declaration of Helsinki and was approved by the Córdoba Research Ethics Committee. Informed consent was obtained from all participants. SAGER guidelines were followed regarding potential sex or gender bias.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCE
No artificial intelligence was used in the preparation of this article.
AUTHORS’ CONTRIBUTIONS
F. Di Cosmo and L. Barreiro Mesa contributed equally to this work. D. Mesa Rubio and M. Ruiz Ortiz conceived and validated the study. M. Ruiz Ortiz administered the project and conducted the formal analysis. M. Pan Álvarez-Ossorio and D. Mesa Rubio supervised the conduct of the study. F. Di Cosmo and L. Barreiro Mesa drafted the original manuscript. All authors contributed to research, reviewed and edited the manuscript, approved its final version, and are responsible for all aspects of the work.
CONFLICTS OF INTEREST
M. Pan Álvarez-Ossorio and D. Mesa Rubio declared to have received honoraria for sessions related to the topic of the manuscript. The remaining authors declared no conflicts of interest whatsoever.
REFERENCES
1. McDonagh T, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42:3599-3726.
2. Godino C, MunafòA, Scotti A, et al. MitraClip in secondary mitral regurgitation as a bridge to heart transplantation:1-year outcomes from the International MitraBridge Registry. J Heart Lung Transplant. 2020;39:1354-1326.
3. ManufòA, Scotti A, Estévez-Loureiro R, et al. 2-year outcomes of MitraClip as a bridge to heart transplantation:The international MitraBridge registry. Int J Cardiol. 2023;390:131-139.
4. Dunlay SM, Roger VL, Killian JM, et al. Advanced Heart Failure Epidemiology and Outcomes:A Population-Based Study. JACC Heart Fail. 2021;9:722-732










