Instead of writing a conventional editorial I have tried to respond to the question of Dr Fernando Alfonso, Associate Editor of REC: Interventional Cardiology: “where are we going?” by letting myself be interviewed by a senior interventional cardiologist from South America, Dr Rodrigo Modolo, who is currently writing his PhD thesis in Rotterdam.
QUESTION: Professor, do we need another interventional cardiology journal?
ANSWER: Rodrigo, in the United States we have, ranked by their impact factors, 3 influential interventional cardiology journals: JACC: Cardiovascular Interventions, Circulation: Cardiovascular Interventions, and Catheterization and Cardiovascular Interventions.
In Europe, EuroIntervention is the journal of the EAPCI (European Association of Percutaneous Intervention). But we have a tendency to forget that the language of the South American continent is Spanish (…and Portuguese, as Dr Modolo reminded me), and the Spanish language represents one of the 3 most widely spoken languages in the world.
Revista Española de Cardiología currently has a major impact factor and faces the challenge of creating a new subspecialty journal, REC: Interventional Cardiology. It is a challenging decision but also a great opportunity.
Q.: Do you think that interventional cardiology has reached its peak maturity?
A.: Interventional cardiology has reached the peak of its 40 years of existence and it is difficult to predict the future. The advent and adoption of balloon angioplasty with an initial success rate of 80% to 85% and a restenosis rate of 30% will not happen again, nowadays. Bare-metal stents and drug-eluting stents were and are successful stories, but, purely as examples, directional atherectomy and laser for the treatment of coronary artery disease did not survive rigorous randomized controlled trials.1,2
Q.: Prof. following Andreas Grüntzig, has there been in your view another major pioneer in the field?
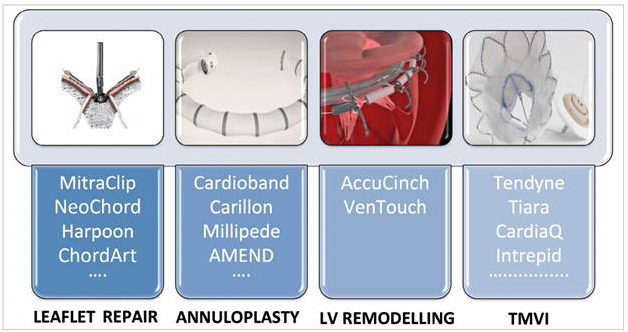
A.: After Andreas Grüntzig, the second great pioneer was Alain Cribier, who has revolutionized the field of valvular treatment. Over the last decade, interventional cardiologists have systematically “copied the technical approach, tips and tricks of the surgeons” (eg, the Alfieri edge-to-edge clip technique for mitral repair)–and will keep doing so (figure 1).3 The 20th and the early 21st century have been and will be the centuries of implantable devices (starting with the pacemaker implanted by Åke Senning, a surgeon and pioneer). Today, “drugs and surgeon” seem to be being supplanted by permanently implanted devices, due to their benefits, cost-effectiveness, and other advantages.
Figure 1. Different approaches for mitral valve interventions. Reprinted from Taramasso et. al.,3 with permission from Europa Digital & Publishing. LV, left ventricular; TMVI, transmitral valve implantation.
However, we have attempted and we keep trying to replace permanent metallic implants by a bioresorbable template to facilitate a vascular or valvular restoration therapy with cellular colonization of the template. So far we have not convinced the interventional community.4,5 But a first attempt with a novelty in interventional cardiology is frequently imperfect, facing new enemies and sometimes it is doomed to disappear.
Q.: Fernando Alfonso asked you the question: “where are we going?” Could you provide him with your personal response?
A.: How could I possibly answer the question? I will try, but let me tell you that the history of interventional cardiology has so far been unpredictable and intimately related to the history of medicine, biology, physics, and other disciplines.
Q.: Why does interventional cardiology have to be related and connected to the world of molecular biology, biomechanics, epidemiology, physics, etc?
A.: Let me answer your question by telling you my recent perception of progress in medicine at a meeting in December 2018, at the Cardiovascular Symposium of Valentín Fuster in New York. In the last session I was a speaker, sandwiched between 2 giants in medicine: Eugene Braunwald and Alain Carpentier, the surgeon who revolutionized the treatment of the mitral valve. It gave me the opportunity to dialogue with the generation that preceded my generation and to ask them (it’s my turn) the question “where are we going?”
Dr Braunwald gave a very clear and succinct answer. Number 1, the use of genomics for the early detection and prevention of disease will fully emerge in the next decades. Number 2, the predominance of noninvasive imaging (multislice computed tomography scans, positron emission tomography, magnetic resonance imaging, and a combination of these imaging techniques) will be predominant and replace conventional diagnostic cinefluoroscopy as well as many other diagnostic tests. In our weekly research discussion and as a joke, the fellows and myself frequently evoke the “Imagomics” era (a combination of imaging and genomics). Number 3, the discovery of new biomolecules and physiological principles such as PCSK9 blockers (not only monoclonal antibodies against PCSK9 but microRNA inhibitors of PCSK9 production) and others such as iSGLT2, which inhibits sodium-glucose pump reabsorption in the kidney while differently affecting the afferent and efferent vessel of the kidney glomeruli, a drug that might have major effects not only on diabetes, but also on heart failure and proteinuria. With child-like enthusiasm Dr Braunwald described that drug as the “statin of heart failure”.
When he was asked about the relationship with percutaneous intervention his response was swift. The Fourier study on monoclonal antibodies against PCSK9 has already demonstrated a 22% reduction in coronary interventions, warning us, interventional cardiologists, that a drastic change in the treatment of stable angina may be on the horizon in the next decade.6
Early detection by genomics of coronary artery disease risk factors, early demonstration by noninvasive imaging of the subclinical phenotype of the disease and early treatment by biannual injection of microRNA to block the production of PCSK may potentially “eradicate” the disease as predicted by the 2 Nobel prize laureates for their discovery of low-density lipoprotein receptors, Michael Stuart Brown and Joseph L. Goldstein in 1985 in their inaugural lecture in Stockholm.7 He added that so far there is no real device treatment for heart failure, a complex multifactorial disease, although resynchronization and mechanical bipartition of the dyskinetic aneurysmal left ventricle are partially successful.8 As far as diabetes is concerned, a late key opinion leader in interventional cardiology did benefit from an implanted insulin micropump but beyond that device there is no specific device for the “causal” treatment of diabetes (such as renal denervation) and we still have to depend on pancreas transplantation.9
For his part, Alain Carpentier has for many years been focusing on the intrathoracic artificial heart as a final mechanical treatment of heart failure. His artificial heart CARMAT (Carpentier and Matra Company) is a marvel of technology, and has been implanted in 14 patients. These 2 giants, Braunwald and Carpentier, have obviously opposite but complementary views on the topic of heart failure.
Valentín Fuster, our host at this meeting in New York, relies strongly on primordial prevention (prevention in children between 3 and 5 years), primary and secondary prevention in an attempt to alleviate the burden of coronary artery disease in the decade to come.10 More modestly, at that meeting I reviewed our work on tailor-made decision-making between percutaneous coronary intervention and coronary artery bypass graft based solely on non- invasive imaging.11-14 Clearly one of my predictions is the disappearance of diagnostic cinefluoroscopy from conventional catheterization laboratories, which in future will have to be used exclusively in an interventional suite.11-14
After SYNTAX III, the Revolution CABG trial–on the verge of starting–on the planning and execution of surgery without prior cineangiography, thus guided solely by multislice computed tomography, will be an important first-in-man trial and a proof-of-concept.
Q.: Then, what about the “unpredictability” of the evolution of interventional cardiology?
A.: Dr Modolo, let me illustrate that unpredictability by the following anecdotes. In 1974, in Frankfurt, at a meeting organized by Paul Lichten and as a young catheterization laboratory physician, I went to see the poster of a young radiologist called Andreas Grüntzig. Honestly I could not anticipate that his technique, called percutaneous transluminal balloon angioplasty, applied on a dog’s left anterior descending coronary artery ligated by a piece of catgut, would ever mark the beginning of a new clinical era just 1 year later.15
In 1986 when I tried to follow and to apply the pioneering endeavor of Jacques Puel and Ulrich Sigwart with the Wallstent, I could not anticipate that I would report in the New England Journal of Medicine in 1991 a rate of acute or chronic occlusion above 20%!16
It took me 3 years to recover from this disastrous publication; in 1994 in the New England Journal of Medicine the results of the Benestent trial17 with the balloon expandable Palmaz-Schatz were embraced swiftly by the interventional community.
I must admit that in 1999 I immediately saw the tremendous potential of rapamycin (sirolimus drug-eluting stent) when I was exposed to the experimental animal work of Robert Falotico at the headquarters of Cordis in New Jersey.18
In 2002, I implemented a policy of unrestricted use of drug-eluting stents fiercely criticized at that time, but today fully endorsed by the interventional community.19
In 2004, Alain Cribier helped me to perform our first antegrade valve replacement at the ThoraxCenter; but it took me another year to start the CoreValve program in collaboration and competition with Eberhard Grube. In both institutions, initial cases were performed either with extracorporeal membrane oxygenation or TandemHearts. These historical anecdotes show that I was not and am still not a visionary pioneer but just a fast adopter, and that the future of interventional cardiology is quite unpredictable; Rodrigo, as another example, the surge, demise and the rebirth of renal denervation. So, do not ask me to be precise in futuristic prediction.
Q.: Thus you will not answer the question of Dr. Alfonso, where are we going?
A.: I will try to answer this question but the prediction would have to be checked over the next decade.
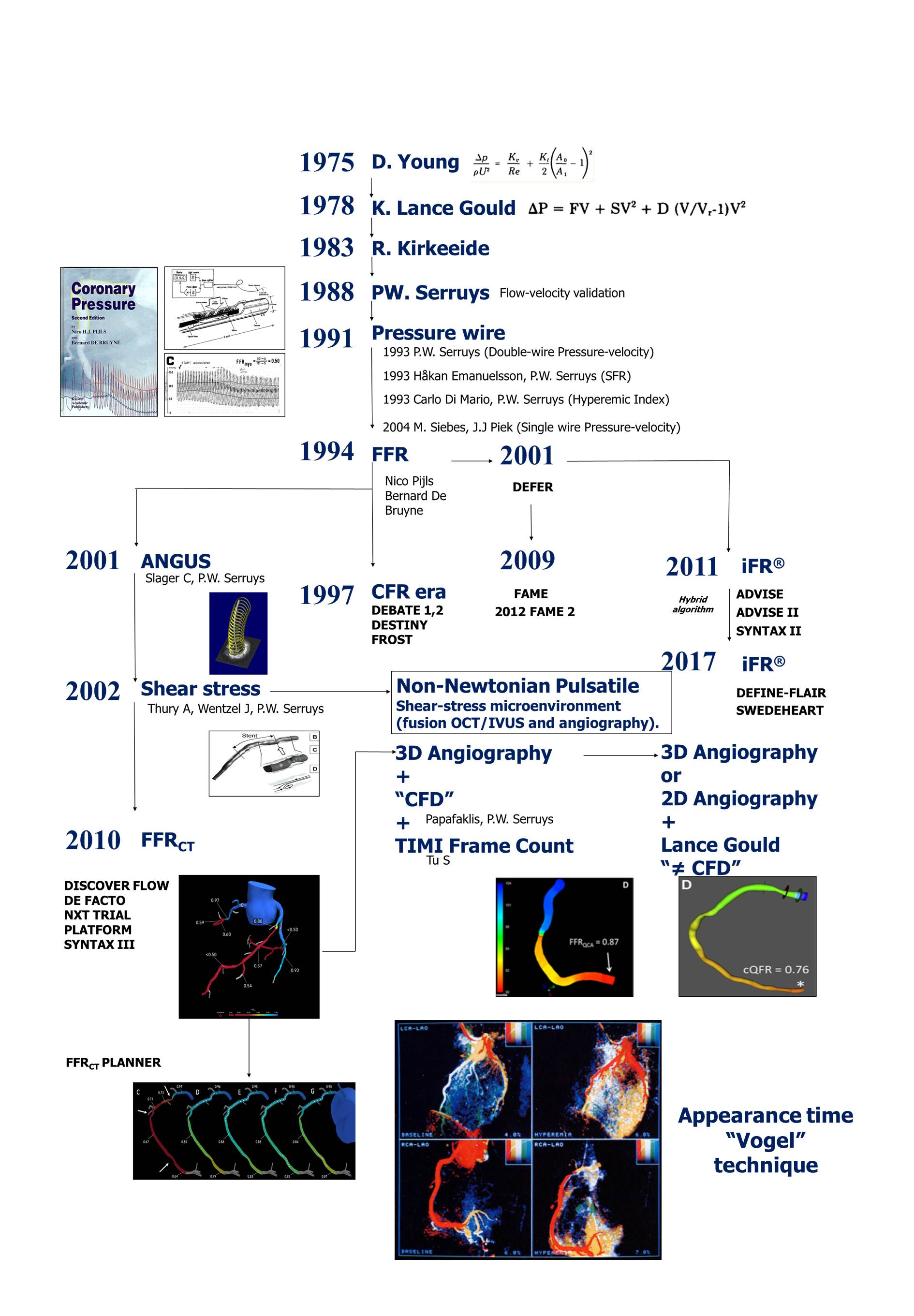
This decade is ending with a “war on stents”. All the clinical outcomes of the novel stents are in the range of 5% for target vessel failure (table 1), but 1 patient in 5 has residual angina.20 That has to be elucidated by sophisticated physiology that has to identify the epicardial stenotic lesion to be treated, for significant physiological reasons, the epicardial angiographic stenosis that should not be treated, and the presence of diseased microcirculation.21 We will have to resolve the concordance and discordance between fractional flow reserve and coronary flow reserve and find a biological treatment for the microvascular disease. Noninvasive imaging is also emerging to make the triage between the lesion that needs to be treated and those that have to be left alone (figure 2).
Table 1. Primary outcomes of recent stent trials
| Trial | Follow-up | Tested device | Number of patients | Target vessel failure | Comparator | Number of patients | Target vessel failure | Primary result |
|---|---|---|---|---|---|---|---|---|
| BIONYX | 1 year | Ultrathin-BP-SES (Orsiro) | 1243 | 4.5% | Thin-DP-ZES (Resolute Onyx) | 1245 | 4.7% | Noninferiority met |
| TARGET | 1 year | Thin-BP-SES (FIREHAWK) | 823 | 6.1% | Thin-DP-EES (Xience) | 830 | 5.9% | Noninferiority met |
| TALENT | 1 year | Ultrathin-BP-SES (Supraflex) | 720 | 4.9% | Thin-DP-EES (Xience) | 715 | 5.3% | Noninferiority met |
| ReCre8 | 1 year | Thin-PolymerFree-SES (Cre8) | 747 | 6.2%* | Thin-DP-ZES (Resolute Integrity) | 744 | 5.6%* | Noninferiority met |
Figure 2. Introduction and evolution of coronary physiology in the clinical laboratory. CFD, computational flow dynamics; FFRCT, fractional flow reserve in cardiac tomography; SFR, stenotic flow reserve.
In figure 2 I summarize the introduction and the evolution, which I have witnessed, of physiology in the clinical lab starting with the Young equation in 1975 and ending up with the quantitative flow ratio. I would not be surprised if I see a return of the so called “Vogel technique”,22 which combines the appearance time of the contrast medium in the epicardial vessel during conventional angiography and the videodensitometric assessment of the myocardial blush to assess the coronary flow reserve from cineangiography. Combined with the quantitative flow ratio, it may again become an appealing technology not requiring the use of the pressure wire, and providing the clinician with fractional flow reserve and coronary flow reserve simultaneously.
It is superfluous to describe the extraordinary explosion of structural heart treatment. Just to put history and prediction into perspective, in a keynote lecture at EuroPCR in May of 2007, I reviewed the outcomes of 677 patients with aortic stenosis treated worldwide with transcatheter aortic valve implantation. At that time, the ThoraxCenter had treated 61 patients (nearly 10% of the worldwide population with transcatheter aortic valve implantation!). Today, all 4 valves (with stenosis or regurgitation) have been treated and hundreds of thousands of patients have been treated. I have already mentioned in this interview the concept of restorative therapy aiming to replace the animal bioprosthesis fixed in glutaraldehyde. Certainly another decade will be necessary to achieve that goal. Alain Carpentier wants to put an end to the “cannibal activity” of heart transplantation.
Q.: Will interventional cardiology expand in other noncardiologic fields?
A.: In the next decade, the field of ischemic stroke treatment will have to be conquered more aggressively and become a successful story like “stent for life”. As pointed out by Petr Widimsky in a recent editorial in EuroIntervention,23 the bar for training in neurointervention for interventional cardiologists has maybe been set too high by neurointerventionists in their attempt to collaborate with interventional cardiologists. Fusion of specialized knowledge –neurointervention–and long battlefield practice of interventional cardiologists in revascularization of myocardial infarction has to be accomplished in the next decade.
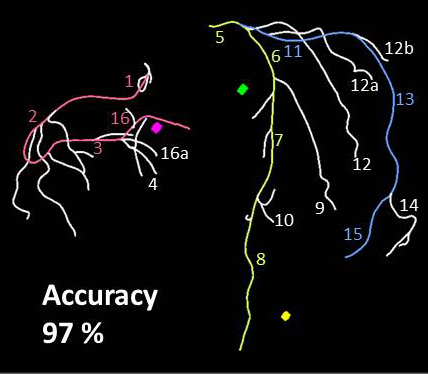
Artificial intelligence, learning machines, and big data are today common in our scientific discussions. However my personal experience is that you need a specific target. With Imperial College, we are currently focusing on a fully automatic anatomic SYNTAX score derived from multislice computed tomography (segmentation, tortuosity, length of lesion, identification of long diffuse lesion, metric evaluation of calcium… all can be mastered by the so called artificial intelligence) (figure 3).
Figure 3. Automatic segmentation of the coronary tree derived from multislice computed tomography showing an accuracy of 97%.
Finally, big data has become a reality. Just a few weeks ago on all European TV screens we saw the first results obtained from 8 million data collected on implants, thereby detecting unusual and rare complications otherwise not reported by industries or physicians.
Finally, 2 very important clinical fields, as I mentioned earlier, diabetes and heart failure remain outside and beyond our device approach (so far…). In the previous decade, there was the tremendous hype that myogenesis would be a fast solution to this endemic cardiovascular entity.24 Bipartition of the dyskinetic aneurysmatic ventricle is only a very specific approach, close to a niche, and on the horizon there is at this point of time nothing very promising. Basic science will have to make major discoveries before we, interventional cardiologists, get seriously involved in the field of myocardial repair. But as usual we will be surprised by the ingen-iousness of the human mind. To end on an optimistic note, renal denervation almost died a few years ago as a consequence of rig-orously controlled trials with sham,25,26 but this year there was clearly a rebirth or renaissance of renal denervation with 2 new positive trials using a sham arm as a comparator.27,28
In the next decade, the wealth of knowledge stemming from the use of genomics, big data, and artificial intelligence will deeply affect our lives as human beings, physicians, and interventional cardiologists. More than ever, the new journal will have to guide us through the enormous flow of information.
CONFLICTS OF INTEREST
The authors declare no conflict of interest for the present editorial.
REFERENCES
1. Appelman YE, Piek JJ, Strikwerda S, et al. Randomised trial of excimer laser angioplasty versus balloon angioplasty for treatment of obstructive coronary artery disease. Lancet. 1996;347:79-84.
2. Topol EJ, Leya F, Pinkerton CA, et al. A comparison of directional atherectomy with coronary angioplasty in patients with coronary artery disease. The CAVEAT Study Group. N Engl J Med. 1993;329:221-227.
3. Taramasso M, Feldman T, Maisano F. Transcatheter mitral valve repair:review of the clinical evidence. EuroIntervention. 2018;14:AB91-AB100.
4. Wykrzykowska JJ, Onuma Y, Serruys PW. Vascular restoration therapy:the fourth revolution in interventional cardiology and the ultimate “rosy“prophecy. EuroIntervention. 2009;5(Suppl F):F7-8.
5. Pyxaras SA, Wijns W. Polymeric bioresorbable coronary scaffolds:the hype is over, but the dream lives on. EuroIntervention. 2018;13:1506-1509.
6. Sabatine MS, Giugliano RP, Keech AC, et al.;Committee FS and Investigators. Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease. N Engl J Med. 2017;376:1713-1722.
7. The Nobel Prize. Michael S. Brown's Nobel Lecture. Available at:https://www.nobelprize.org/prizes/medicine/1985/brown/lecture/. Accessed 6 Jan 2019.
8. Thomas M, Nienaber CA, Ince H, Erglis A, Vukcevic V, Schafer U, Ferreira RC, Hardt S, Verheye S, Gama Ribeiro V, Sugeng L, Tamburino C. Percutaneous ventricular restoration (PVR) therapy using the Parachute device in 100 subjects with ischaemic dilated heart failure:one-year primary endpoint results of PARACHUTE III, a European trial. EuroIntervention. 2015;11:710-717.
9. Carpentier A, Patterson BW, Uffelman KD, et al. The effect of systemic versus portal insulin delivery in pancreas transplantation on insulin action and VLDL metabolism. Diabetes. 2001;50:1402-1413.
10. Fernandez-Friera L, Fuster V, Lopez-Melgar B, et al. Normal LDL-Cholesterol Levels Are Associated With Subclinical Atherosclerosis in the Absence of Risk Factors. J Am Coll Cardiol. 2017;70:2979-2991.
11. Modolo R, Collet C, Onuma Y, Serruys PW. SYNTAX II and SYNTAX III trials:what is the take home message for surgeons?Ann Cardiothorac Surg. 2018;7:470-482.
12. Collet C, Onuma Y, Andreini D, et al. Coronary computed tomography angiography for heart team decision-making in multivessel coronary artery disease. Eur Heart J. 2018;39:3689-3698.
13. Collet C, Miyazaki Y, Ryan N, et al. Fractional Flow Reserve Derived From Computed Tomographic Angiography in Patients With Multivessel CAD. J Am Coll Cardiol. 2018;71:2756-2769.
14. Norgaard BL, Leipsic J, Achenbach S. Coronary CT Angiography to Guide Treatment Decision Making:Lessons From the SYNTAX II Trial. J Am Coll Cardiol. 2018;71:2770-2772.
15. Gruntzig A. Transluminal dilatation of coronary-artery stenosis. Lancet. 1978;1:263.
16. Serruys PW, Strauss BH, Beatt KJ, et al. Angiographic follow-up after placement of a self-expanding coronary-artery stent. N Engl J Med. 1991;324:13-17.
17. Serruys PW, de Jaegere P, Kiemeneij F, et al. A comparison of balloon-expandable-stent implantation with balloon angioplasty in patients with coronary artery disease. Benestent Study Group. N Engl J Med. 1994;331:489-495.
18. Rensing BJ, Vos J, Smits PC, et al. Coronary restenosis elimination with a sirolimus eluting stent:first European human experience with 6-month angiographic and intravascular ultrasonic follow-up. Eur Heart J. 2001;22:2125-2130.
19. Lemos PA, Serruys PW, Sousa JE. Drug-eluting stents:cost versus clinical benefit. Circulation. 2003;107:3003-3007.
20. Stone GW, Ellis SG, Gori T, et al. Blinded outcomes and angina assessment of coronary bioresorbable scaffolds:30-day and 1-year results from the ABSORB IV randomised trial. Lancet. 2018;392:1530-1540.
21. Echavarria-Pinto M, Collet C, Escaned J, Piek JJ, Serruys PW. State of the art:pressure wire and coronary functional assessment. EuroIntervention. 2017;13:666-679.
22. Vogel R, LeFree M, Bates E, et al. Application of digital techniques to selective coronary arteriography:use of myocardial contrast appearance time to measure coronary flow reserve. Am Heart J. 1984;107:153-164.
23. Widimsky P. When will acute stroke interventions be as widely available as primary PCI?EuroIntervention. 2017;13:1269-1272.
24. Smits PC, van Geuns RJ, Poldermans D, et al. Catheter-based intramyocardial injection of autologous skeletal myoblasts as a primary treatment of ischemic heart failure:clinical experience with six-month follow-up. J Am Coll Cardiol. 2003;42:2063-9.
25. Bhatt DL, Kandzari DE, O'Neill WW, et al. A controlled trial of renal denervation for resistant hypertension. N Engl J Med. 2014;370:1393-1401.
26. Ritter AM, de Faria AP, Fontana V, Modolo R, Moreno H. Does Renal Denervation Fit All Resistant Hypertension?The Role of Genetics. J Clin Hypertens (Greenwich). 2016;18:161-162.
27. Azizi M, Schmieder RE, Mahfoud F, et al. Endovascular ultrasound renal denervation to treat hypertension (RADIANCE-HTN SOLO):a multicentre, international, single-blind, randomised, sham-controlled trial. Lancet. 2018;391:2335-2345.
28. Kandzari DE, Bohm M, Mahfoud F, et al. Effect of renal denervation on blood pressure in the presence of antihypertensive drugs:6-month efficacy and safety results from the SPYRAL HTN-ON MED proof-of-concept randomised trial. Lancet. 2018;391:2346-2355.