HOW WOULD I APPROACH IT?
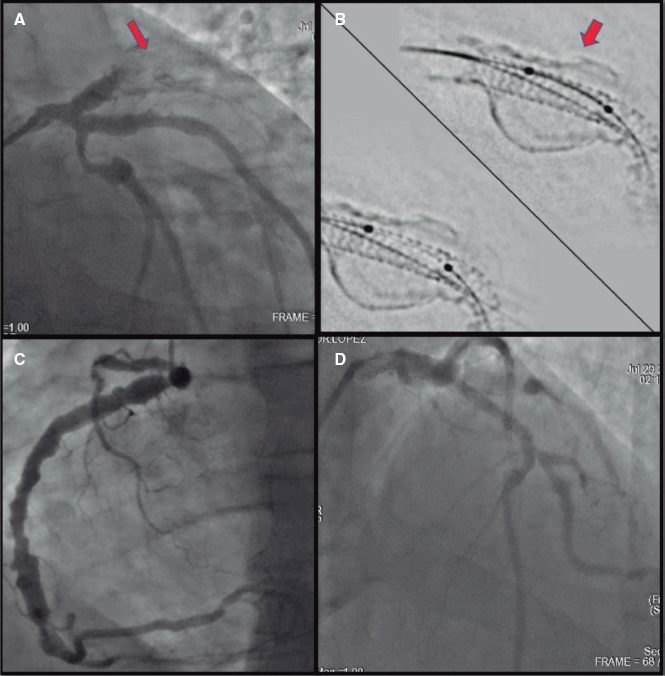
We are facing a challenging situation here both from the clinical–a patient with an acute coronary syndrome with hemodynamic impairment– and technical point of view –the procedure became complicated due to the accidental displacement of the stent from the coronary ostium towards the aorta–.
This is not something rare or due to any technical mistakes, we simply encountered a complication that can occur when treating ostial lesions in 15% of the cases. Even so the best thing to do here is to think about how it could have been prevented.
The management of ostial lesions is effective and safe but there are difficulties too. What we have here are plaques with more fibrosis and calcification that can lead to the infra-expansion and further restenosis or thrombosis of the stent.
Also, it makes arterial catheterization more difficult, there is this possibility of blood pressure drops when inserting the catheter, issues with the positioning and release of the stent and, as it was the case here, even inadequate results.
In order to have some guarantees in the management of these lesions we need to choose a guiding catheter capable of providing good support, prepare the lesions with predilatation or use rotational atherectomy devices, and ultimately be very precise when positioning the stent. In this sense, it is advisable to implant it in the aorta with a 1 mm protrusion to make sure that the entire plaque has been covered.
This last step became complicated, yet different maneuvers have been described in the medical literature to avoid stent displacement. The first thing to do is to identify which is the ideal position here by using different views; then, we are supposed to keep firm and constant pressure over the stent during implantation. Leaving a second guidewire as a marker of the aorta can be helpful here. Also, the same intracoronary guidewire can be used to immobilize the stent in the position we want through ventricular pacing through the angioplasty guidewire.1
The use of guiding catheter extension devices has been suggested here to improve the positioning of the stent during implantation.
With this idea in mind, we can try to stabilize it by using the buddy balloon anchor stent technique.
Szabo described one technique that used a second guidewire in the aorta to anchor the stent to the ostium by passing its proximal edge through the last cell of the stent. It is a relatively complex technique, success rate is between 78% and 90%, and there are risks involved (stent displacement, guidewire crossing, damage to the stent, etc.)
Several devices have been designed with this idea in mind such as the FLASH Ostial System, (Cardinal Health, California, United States) that uses one distal balloon angioplasty plus another proximal anchoring balloon for proximal stent edge apposition to the aorta or the Cappella system, (Cappella Medical Devices, Ireland), that includes a self-expandable stent to provide optimal ostial coverage, although in the case of hard fibrocalcific plaques it does not have enough radial power. The Ostial PRO system (Merit Medical Systems) helps in the ostial positioning of the stent by placing nitinol legs against the aortic wall to avoid implantations that may be too distal. However, none of these systems is used routinely for the management of ostial lesions and although these techniques can be used occasionally, the planning and careful performance of the procedure by an experienced interventional cardiologist should are still the treatment of choice as it was the case with our patient.
The fact of the matter is that, despite of everything, we found ourselves with an under-expanded stent that was displaced towards the aorta and implanted outside the coronary ostium. This excessive protrusion can originate thrombi, anticipate a future risk of embolization, and most assuredly complicate access to the coronary in new procedures.
Several options can help us to solve this problem:
• Stent removal:
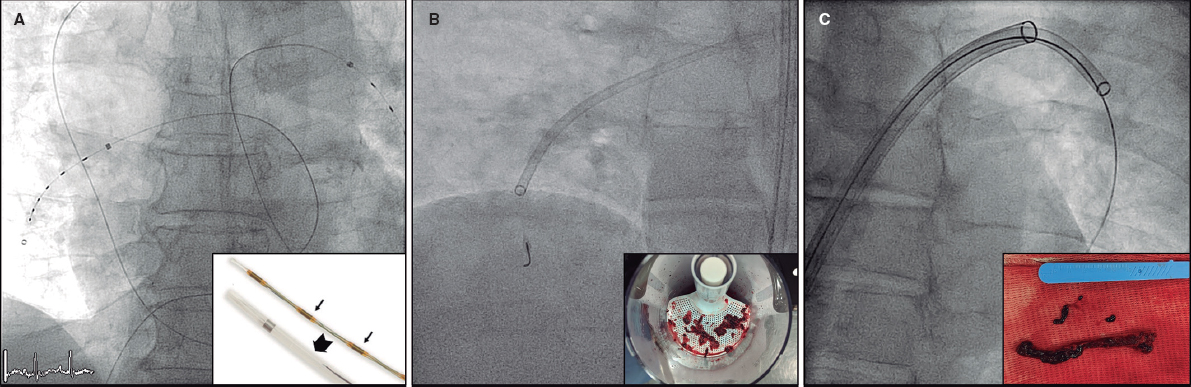
By having a guidewire through the under-expanded stent and protruding into the aorta, the first maneuver here would be to advance the balloon through the stent in order to dilate the coronary artery proximal segment to guarantee its patency. Then the partially inflated balloon is smoothly removed up to the distal edge of the under-expanded stent, the stent is displaced towards the aorta and, if removed, it is advanced towards the guiding catheter. If the stent is partially implanted in the vessel wall, this maneuver won’t probably by successful. Another option here would be to use the loop snare technique to capture the proximal edge of the stent that is protruding into the aorta. Some of the cases published2,3 describe stent “explants” performed using this technique in ostial lesions with stents displaced towards the aorta. However, there is a risk of endothelial damage, dissection, and perforation with this maneuver. Also, after capturing the stent with the loop snare, the movement of traction to attempt the stent retrieval would probably lead to losing the intracoronary guidewire with the corresponding risk of vessel occlusion.
• Stent “modification”:
In order to avoid the risks involved in this retrieval maneuver, we could also solve this complication by inserting a second intracoronary guidewire through the same guiding catheter or, if an alternative vascular access is possible, by using another guiding catheter to allow optimal coaxiality such as the Amplatz Right guidewire. We would have to orient the catheter to pass the new intracoronary guidewire through one cell of the stent segment that protrudes into the aorta and very close to the coronary ostium. Here we would need to advance a 1.5 or 2 mm balloon to open the struts in the stent and then proceed to dilate using gradually larger balloons until we would be able to open our way and deploy a new stent to cover the diseased area of the proximal coronary artery and the under-expanded distal segment of the first stent. Finally, we would have to over-dilate the proximal edge at a high pressure by using a long enough noncompliant balloon to guarantee the crushing of the stent that is protruding into the aorta and its apposition to the aortic wall. The very few cases published on this regard describing this maneuver for the management of stents with excessive aortic protrusion have shown favorable outcomes.
Although a good prior strategy and preparation of the lesion are essential to prevent complications from happening, unexpected sudden situations can trigger all sorts of complications. The interventional cardiologist’s experience, expertise, and caution are crucial to solve these complications.
REFERENCES
1. Lasa G, Larman M, Gaviria K, et al. Inmovilización del stent coronario durante la angioplastia mediante estimulación ventricular transcoronaria con guía terapéutica. Rev Esp Cardiol. 2009;62:288-292.
2. Meisel SR, DiLeo J, Rajakaruna M, et al. A Technique to Retrieve Stents Dislodged in the Coronary Artery Followed by Fixation in the Iliac Artery by Means of Balloon Angioplasty and Peripheral Stent Deployment. Catheterization Cardiovasc Interv. 2000;49:77-81.
3. Curran PJ, Currier J, Tobis J. Percutaneous Snare Retrieval of a Partially Embedded Wallstent. Catheterization Cardiovasc Interv. 2004;61:400-402.
Corresponding author: Servicio de Cardiología, Hospital Clínico Universitario Virgen de la Arrixaca, Carretera Madrid-Cartagena s/n, 30120 El Palmar, Murcia, Spain.
E-mail-address: epbhva@yahoo.es (E. Pinar Bermúdez).