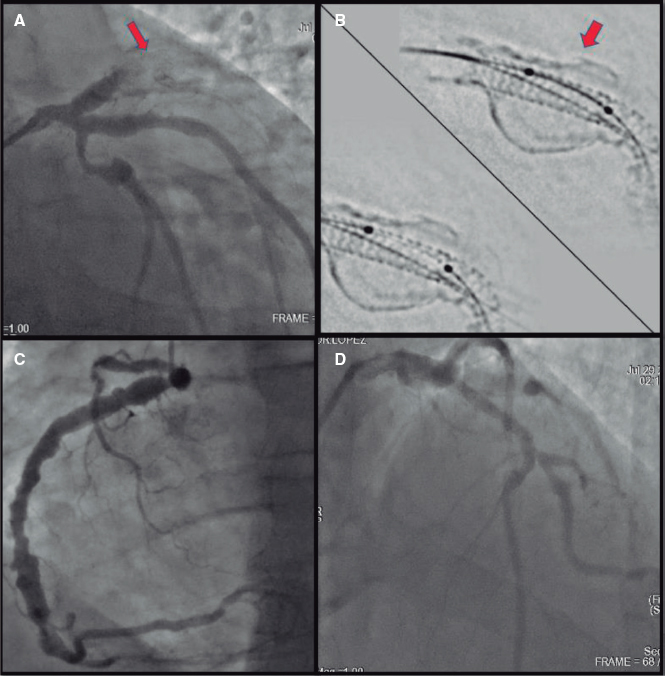
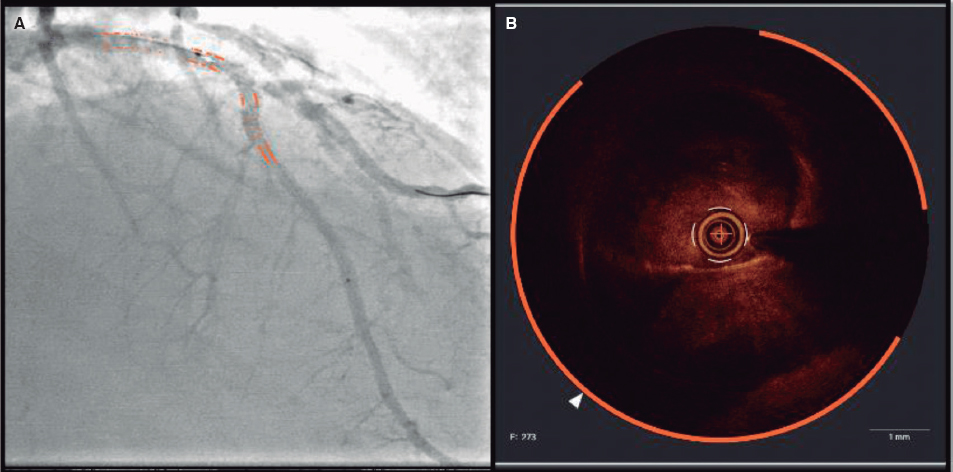
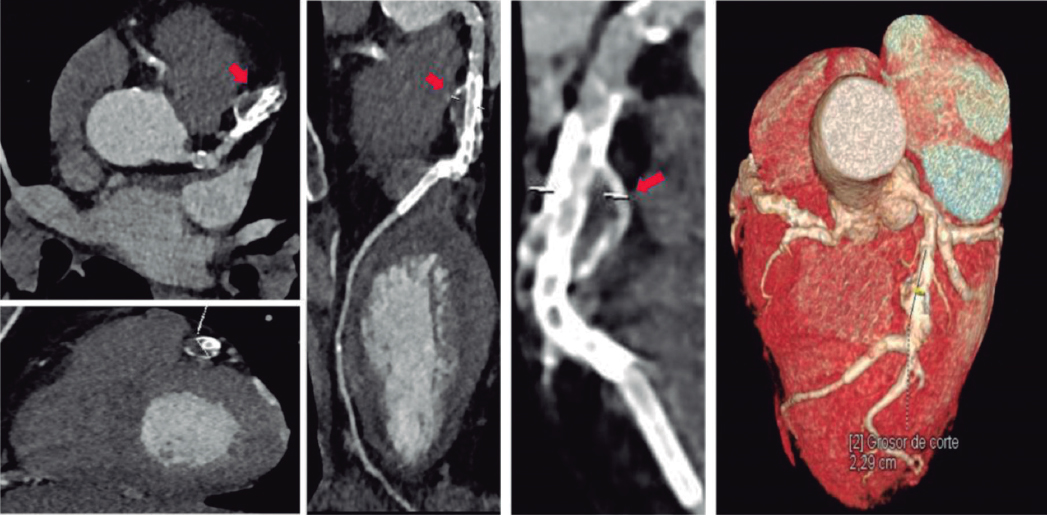
A 53-year-old male smoker with hypertension and a family history of dyslipidemia and early ischemic heart disease in family members was diagnosed with anterior ST-segment elevation acute coronary syndrome (STEACS) in 2017. He was treated with a 4 mm × 18 mm everolimus-eluting stent implanted in the proximal left anterior descending coronary artery and 2 overlapping distal stents. The procedure was uneventful, and the remaining arteries showed ectasia with diffuse atheromatous disease. An echocardiogram revealed the presence of mild left ventricular systolic dysfunction. The patient was readmitted after experiencing a new anterior STEACS due to very late thrombosis of the previous stent in the proximal left anterior descending coronary artery, where an external calcified image was found around the stent (figure 1A,B: arrows). The study was completed with optical coherence tomography (figure 2A,B), which revealed the presence of abundant thrombotic content, and stent malapposition, without visualization of the surrounding arterial wall, indicating a large thrombosed and calcified aneurysm. Thrombus aspiration and a drug-coated balloon were used, along with glycoprotein IIb-IIIa inhibitors, resulting in final TIMI grade 3 flow. Computed tomography (figure 3: arrows) performed during admission confirmed the presence of a 24 mm coronary aneurysm with a thrombosed sac. The patient progressed favorably and was discharged from the hospital.
Figure 1.
Figure 2.
Figure 3.
Coronary aneurysms are a rare finding whose incidence ranges from 0.1% to 4.9%. The etiology can be atherosclerotic, congenital, or inflammatory. In our case, atherosclerotic etiology was suspected. However, it could have been intensified by an everolimus-related toxic effect due to hypersensitivity following stenting. This effect is less likely since it was not found in other treated segments, and ectasia was present in the remaining arteries (figure 1C-D; videos 1-2 of the supplementary data). Treatment consisted of indefinite dual antiplatelet therapy after confirming the absence of lack of endothelialization across the aneurysm neck.
FUNDING
None declared.
ETHICAL CONSIDERATIONS
The patient’s prior written informed consent was obtained, and possible sex and gender variables were taken into account following SAGER guidelines.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCE
No artificial intelligence tools were used in the preparation of this manuscript.
AUTHORS’ CONTRIBUTIONS
All authors contributed to the drafting of the article. A.T. Ariza-Mosquera, and F. Sabatel-Pérez wrote the text. F. Sabatel-Pérez, M. López-Pérez, and T. Gil-Jiménez were involved in the review and supervision process. G. Moreno Terribas and J. Caballero-Borrego critically revised the manuscript.
CONFLICTS OF INTEREST
None declared.
SUPPLEMENTARY DATA
Vídeo 1. Ariza-Mosquera AT. DOI: 10.24875/RECICE.M23000422
Vídeo 2. Ariza-Mosquera AT. DOI: 10.24875/RECICE.M23000422