ABSTRACT
The current COVID-19 outbreak is forcing healthcare workers to continuously reconsider the proper indications for cardiac catheterization. Human and material resources optimization, infection prevention for patients and healthcare workers, and transfer times force a rethink of the previously established protocols. This article is a consensus statement of the Interventional Cardiology Association and the Ischemic Heart Disease Association of the Spanish Society of Cardiology, and aims to provide information to healthcare workers on the indications of diagnostic or therapeutic cardiac catheterization during the current COVID-19 pandemic.
Myocardial infarction. Interventional cardiology. Angioplasty. Infection Prevention. COVID-19. Coronavirus. Pandemic.
RESUMEN
El brote actual de COVID-19 está obligando a los profesionales sanitarios a replantear de forma continua las indicaciones de cateterismo cardiaco. La optimización de recursos materiales y humanos, la prevención de contagios a profesionales y pacientes, así como la gestión de los tiempos de traslado, hace totalmente necesario reformular los protocolos previamente establecidos. El presente texto es un documento de consenso de la Asociación de Cardiología Intervencionista y la Asociación de Cardiopatía Isquémica y Cuidados Agudos Cardiovasculares de la Sociedad Española de Cardiología que pretende dar información al personal sanitario sobre las indicaciones de cateterismo diagnóstico o terapéutico durante la pandemia actual de COVID-19.
Infarto. Cardiología intervencionista. Angioplastia. Infección. Prevención. COVID-19. Pandemia.
INTRODUCTION
The current outbreak of COVID-19 has caused all healthcare providers have to rethink the indications for cardiac catheterization on an ongoing basis. The optimization of material and human resources, the prevention of contagions to healthcare providers and patients, and management during patient transfers makes it absolutely necessary to reformulate the protocols previously established. This consensus document has been agreed by the Spanish Society of Cardiology Working Group on Cardiac Catheterization and Interventional Cardiology (ACI-SEC) and the Spanish Society of Cardiology Working Group on Ischemic Heart Disease and Acute Cardiovascular Care. It includes indications to perform cardiac catheterizations under the current situation. It is difficult to foresee the evolution of this pandemic and its health impact, which will probably force us to readjust this document based on the particular situation and dynamic of each center. It is important to emphasize that when the actual situation is over, we recommend going back to the indications included in the clinical practice guidelines published by the European Society of Cardiology.1
In order to perform cardiac catheterizations our advice is to follow the recommendations on prevention and management included in the consensus document published by the ACI-SEC and the Heart Rhythm Association of the Spanish Society of Cardiology.2
ELECTIVE PROCEDURES
Indication for elective procedures in the catheterization laboratory should be based on individual assessments of the risk of contagion/benefit from the intervention ratio. In the current situation postponing all elective procedures seems the most reasonable thing to do to minimize the possibility of contagion of disease-free patients (and people they may have been in contact with) in a setting of high prevalence of COVID-19 infection such as hospitals. Similarly, performing right catheterizations during this pandemic is ill-advised.
If the cath lab has enough material and human resources, the non-emergent catheterizations of already hospitalized patients without suspicion of COVID-19 or COVID-19-negative patients may be an option to promote early discharges (ie, a study to characterize dilated cardiomyopathy in a patient admitted with an index episode of heart failure).
NON-ST-SEGMENT ELEVATION ACUTE CORONARY SYNDROME
Differential diagnosis
A key element to be taken into consideration when indicating a cardiac catheterization in a patient with acute coronary syndrome (ACS) is the high prevalence of heart disease in patients admitted due to COVID-19,3 the significantly high troponin levels (8% to 12% higher) seen in confirmed cases of COVID-19 but without ACS yet,4 and the possibility that myocarditis complicates the COVID-19 infection.5 This highlights the importance of clinical judgement before establishing a diagnosis of ACS/acute myocardial infarction. In general, in patients hospitalized due to COVID-19 infection who experience high cardiac enzyme levels of coronary origin and remain asymptomatic we recommend following a conservative approach. Coronary angiography should be spared for cases of high suspicion of high-risk ACS, medical treatment-resistant recurrent ischemia, and when the patient’s vital prognosis following the infection anticipates good prognosis.
NON-ST-SEGMENT ELEVATION ACUTE CORONARY SYNDROME
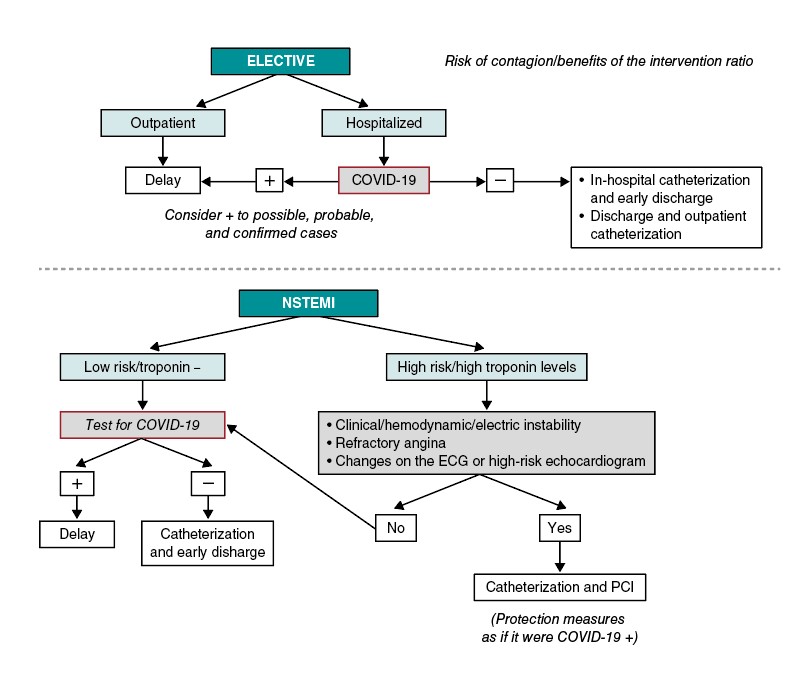
Figure 1 1 shows the approach suggested for patients with non-ST-segment elevation acute coronary syndrome (NSTEACS). In patients hospitalized due to NSTEACS with suspicion of COVID-19 we recommend running the diagnostic test before performing the cardiac catheterization to assess the risk/benefit ratio of the procedure. The current clinical guidelines on revascularization recommend an early invasive strategy (less than 24 h) in patients with at least 1 criterion of high risk and in less than 72 h in patients with at least 1 criterion of intermediate risk.6. In most of the patients with NSTEACS this interval should be enough to confirm or discard the infection. The procedure should be postponed if the patient’s clinical situation allows it in cases where the diagnostic test is not available yet. On the contrary, in patients with NSTEACS but with persistent ischemia or high-risk criteria like recurrent angina, diffuse ST-segment changes suggestive of left main coronary artery or ventricular dysfunction performing the catheterization within the first 2 hours may be an option, taking the necessary protective measures to avoid transmitting the infection.
Figure 1. Algorithm for the management of elective patients and non-ST-segment elevation myocardial infarction (NSTEMI). ECG, electrocardiogram; PCI, percutaneous coronary intervention.
Patients negative for COVID-19 undergoing the procedure should be discharged early from the hospital.
In patients admitted to centers without a cath. lab. who need to be transferred, it is advisable, if possible, to follow a conservative approach and early discharge except for high-risk criteria or poor disease progression.
In selected patients with acute myocardial infarction—especially type 2 7— the conservative approach is the one recommended initially.
Revascularization in NSTEACS and multivessel disease
In patients with NSTEACS and multivessel disease and an indication for complete revascularization who remain hospitalized in centers where surgeries have been postponed, we recommend performing it within the same procedure to reduce hospital stay and avoid having to perform another procedure in the cath. lab.
ST-SEGMENT ELEVATION MYOCARDIAL INFARCTION
The reperfusion treatment during the management of ST-segment elevation myocardial infarction (STEMI) of < 12 hour-duration since symptom onset should be primary percutaneous coronary intervention (pPCI) because it reduces the rates of mortality, reinfarction, stroke,1 and mechanical complications compared to fibrinolysis. Also, a significant percentage of patients undergoing pPCI can be discharged early and don’t require further invasive examinations which simplifies the management of these patients. This reduces the hospital stay and avoids collapsing the entire healthcare system. Nevertheless, during the COVID-19 pandemic the following key points should be taken into consideration:
- Due to the current care overload sustained by the ERs of our healthcare system, transfer times can take longer than usual in many cases.
- The transfer of patients with suspicion or confirmation of COVID-19 should take place safely and with infection under control. Also, after the transfer the ambulance should be properly disinfected. Therefore, the logistics required to guarantee safe transfers can also delay the entire process.
- Despite the preventive measures implemented to avoid transmitting the infection, the transfer of patients with an active infection for COVID-19 to a different center can infect the healthcare providers and, most important of all, other patients hospitalized and who are especially vulnerable to the disease.
- In patients already diagnosed with COVID-19 and in poor clinical state (especially patients hospitalized in intensive care units) with STEACS, repefusion treatment may yield no clinical benefits.
Reperfusion strategy
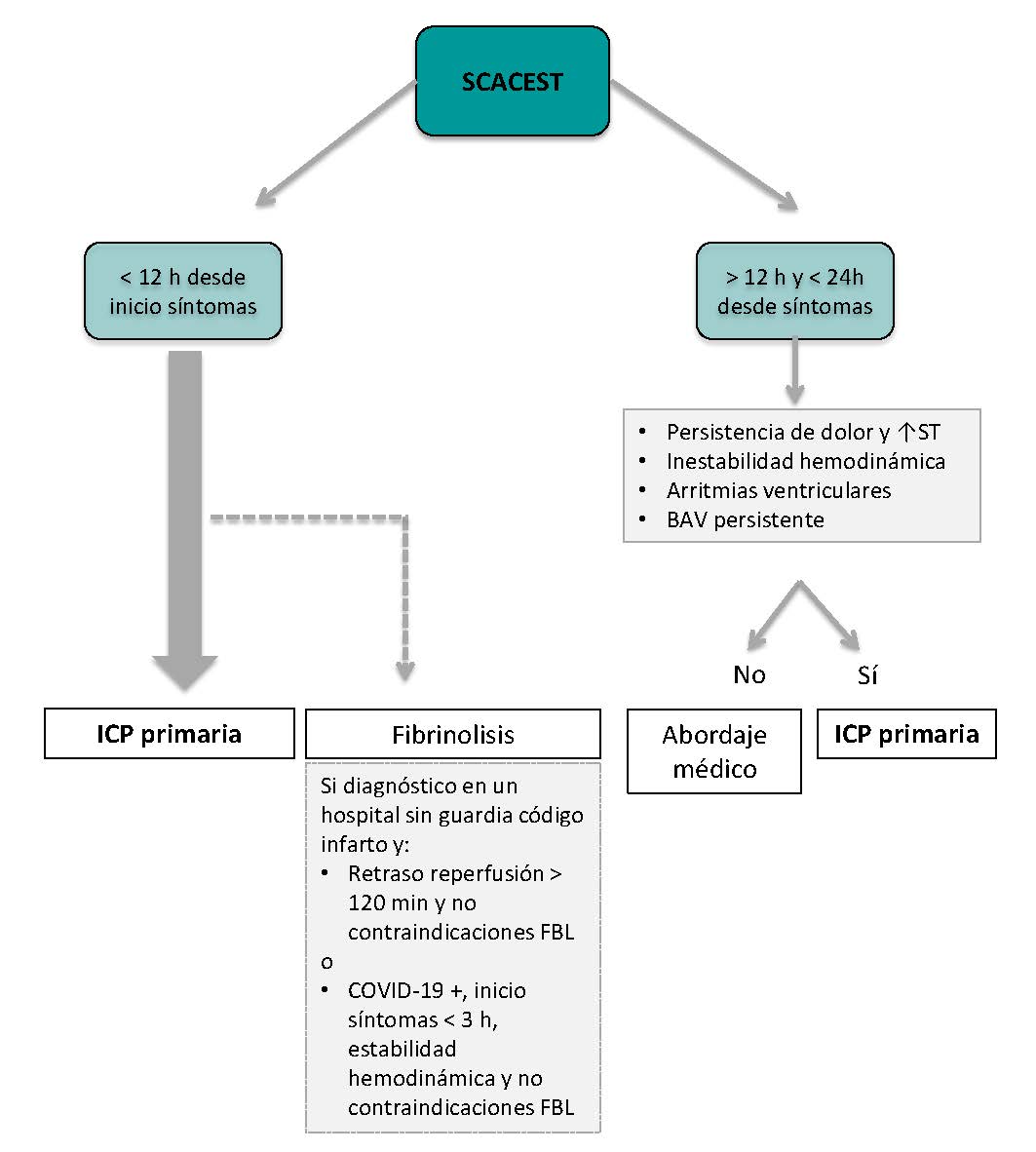
Figure 2 shows the management of STEMI. The ACI-SEC and the Spanish Society of Cardiology Working Group on Ischemic Heart Disease and Acute Cardiovascular Care recommend that the percutaneous coronary intervention should be the reperfusion strategy of choice in most cases. Fibrinolysis should be spared for cases diagnosed in non-PCI capable centers that meet one of the following requirements:
Figure 2. Algorithm for the management of patients with ST-segment elevation myocardial infarction (STEMI). AVB, atrioventricular block; FBL, fibrinolysis; PCI, percutaneous coronary intervention.
- Estimated time to the pPCI > 120 min.
- Patients who have tested positive to COVID-19 with poor clinical state that makes transfer difficult.
- Patients who have tested positive to COVID-19 with low hemorrhagic risk and symptoms of less than 3 hour-duration.
In cases where fibrinolysis may be an option, the lack of contraindications and the administration of the drug in less than 10 min from diagnosis should be guaranteed.1 Then, depending on the patient’s clinical state and the availability of beds in the ICU of the destination hospital, transfer to a center with cath. lab. capabilities may be considered. The rule of thumb here is to avoid transferring patients with confirmed reperfusion and good disease progression.
After the percutaneous coronary intervention, it is recommended that each patient be taken to their referring centers. However, the patients’ clinical situation and bed availability of each center should be individualized in each case.
Other considerations
As a general rule we recommend leaving the number of centers that are part of the infarction code program untouched. Although demand from out-of-hospital emergency medical services may change significantly during the COVID-19 pandemic, a hospitalized patient may have an indication for an urgent cardiac catheterization. In the current situation, transferring this patient to a different center may be more problematic than performing the procedure at the center where the patient is already hospitalized. Our recommendation here is that no PCI capable center should avoid treating infarctions.
Other clinical considerations:
- The diagnosis of STEMI in patients with complete left bundle-branch block is still complex to this day despite the use of different electrocardiographic criteria.8 Therefore, in patients with suspicion or confirmation of COVID-19 who require transfer for reperfusion we recommend agreeing on the diagnosis as much as possible to avoid unnecessary transfers.
- The management of patients with recovered sudden death without overt electrocardiographic criteria of STEMI is still controversial. Although a recent randomized clinical trial showed that these patients don’t benefit from an immediate coronary angiography,9 it is still being performed in most centers. However, due to their clinical situation—if infected—these patients are extremely prone to secreting microdroplets and infecting the healthcare providers. At the same time they are very vulnerable to infection if they are not already infected. For this reason, immediate PCIs are ill-advised in these patients.
- In patients with STEMI without cardiogenic shock and multivessel disease the overall recommendation is to perform a complete revascularization.10 However, in the current situation, we believe that the management of STEMI should be as simple as possible. In this sense, we believe that in most of these patients the management of non-culprit lesions should be postponed until the outbreak of COVID-19 is over. On the other hand, in patients with a clear need for complete revascularization at admission, we recommend the study of all lesions within the same procedure during the acute phase.
CARDIOGENIC SHOCK
In situations of acute coronary syndrome related cardiogenic shock, cardiac catheterization is indicated. The management of critically ill patients is especially complex because intubation, aspiration, and CPR maneuvers can prompt respiratory secretions in the form of aerosols and increase the exposure of the healthcare providers. All critically ill patients should be treated as patients with COVID-19.
The following key points should be taken into oconsideration:
- As in the rest of patients with cardiogenic shock, only the culprit vessel should be revascularized.11
- If intubation is necessary and possible, it should be performed before entering the cath. lab. and in the best conditions possible to comply with all COVID-19 prevention recommendations.
- Connection to a ventilator —a closed system— is recommended prior to manual ventilation with an ambu-bag. If ventilation with manual resuscitation is necessary, the use of high-efficiency particulate air (HEPA) filters between the tube and the bag is recommended.
- The extracorporeal membrane oxygenation (ECMO) machine used by the heart team should be purged at all times before the arrival of patients to reduce the possibility of infection and speed up the whole process. In patients with COVID-19 with cardiogenic shock, ECMO can be used as the first-line therapy compared to other devices like the Impella ventricular support system or the intra-aortic balloon pump counterpulsation.
STRUCTURAL HEART INTERVENTIONS
In general, all structural heart interventions should be postponed until the pandemic is under control. We should remember that most of these procedures require several days at the hospital, but at the same time the ICU/coronary unit beds may become necessary for patients with COVID-19. Also, in some cases structural heart interventions are performed under general anesthesia and intubation or on transesophageal echocardiography monitoring. All of them high-risk situations for the infection of patients and healthcare providers. On the other hand, patients undergoing structural heart interventions are often old and therefore especially susceptible to nosocomial infection due to COVID-19.
Other urgent procedures like aortic valvuloplasty or transcatheter aortic valve implantation in patients with angina at rest, recurrent syncope or refractory heart failure can be performed.
DRUGS
Regarding the drugs commonly used at the catheterization laboratory such as antithrombotic therapies, the recommendations are basically the same regardless of whether the patient has been infected with COVID-19 or not.
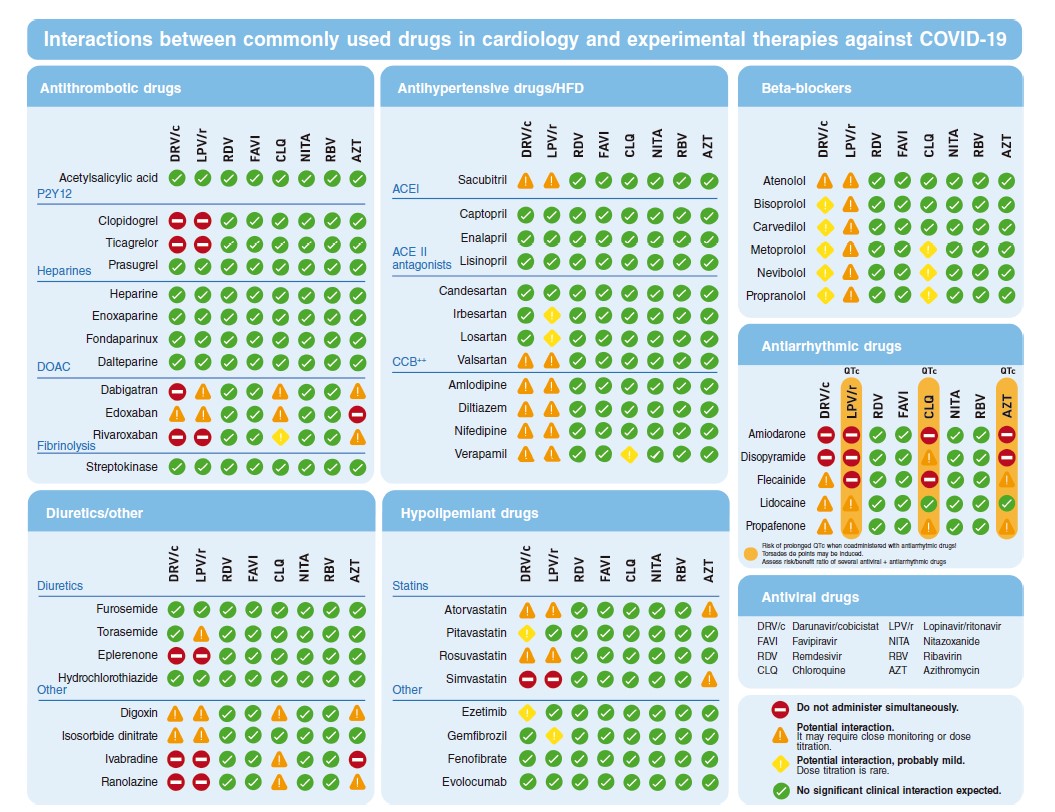
The medication to treat patients with COVID-19 may interact with the most common drugs currently used at the cath lab.12
Figure 3 shows the most commonly used drugs in cardiology both in the context of ACS and stable coronary artery disease.
Figure 3. Possible interactions between the most commonly used drugs in cardiology and the possible treatments used against COVID-19. ACE II, angiotensin-converting enzyme antagonists; ACEI, angiotensin-converting enzyme inhibitors; CCB, calcium channel blockers; DOAC, direct-acting oral anticoagulants; HFD, heart failure drugs.
Antiplatelet therapy
- Adiro: no evidence of significant interactions.
- Oral P2Y12 platelet receptor antagonits: prioritize prasugrel. Concomitant treatment with lopinavir/ritonavir or darunavir/cobicistat increases the effect of ticagrelor and can reduce the effect of clopidogrel.
- Cangrelor: no evidence of significant interactions.
- Tirofiban: no evidence of significant interactions.
Anticoagulant drugs
- Unfractionated heparin: no evidence of significant interactions.
- Bivalirudin: no evidence of significant interactions.
- Enoxaparin: no evidence of significant interactions.
- Fondaparinux: no evidence of significant interactions.
Analgesics/sedatives
- Fentanyl/morphine: potential interactions; prioritize morphine.
- Midazolam: it should not be administered orally. It can be IV administered with special caution.
Inotropes and vasopressors
- Adrenaline: no evidence of significant interactions.
- Dobutamine: no evidence of significant interactions.
- Noradrenaline: no evidence of significant interactions.
- Dopamine: no evidence of significant interactions.
Other
- Nitroglycerin: no evidence of significant interactions.
- Verapamil: potential interactions. Administer and use with special caution and close monitoring.
- Furosemide: no evidence of significant interactions.
CONCLUSIONS
The current outbreak of COVID-19 has made us rethink the invasive approach to ischemic and structural heart disease. The recommendation of the Spanish Society of Cardiology Working Groups on Cardiac Catheterization and Interventional Cardiology and Ischemic Heart Disease and Acute Cardiovascular Care is to postpone all non-emergent procedures to avoid the infection of patients and healthcare providers and minimize the collapse of the healthcare system. However, the percutaneous coronary intervention should still be used for the management of ST-segment elevation myocardial infarction unless prescribed otherwise.
CONFLICTS OF INTEREST
The authors have declared no conflicts of interest regarding this manuscript. R. Moreno is associate editor of REC: Interventional Cardiology. The journal's editorial procedure to ensure impartial handling of the manuscript has been followed.
EDITOR'S NOTE
This manuscript has undergone an especially rapid internal review by the editorial team due to the strong interest indisseminating the information among the scientific community. The editors thank Permanyer Publications for their collaboration and commitment to the prompt publication of this document.
REFERENCES
1. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119-177.
2. Romaguera R, Gonzalez-Cruz I, Ojeda S, et al. Consensus document of the Interventional Cardiology and Heart Rhythm Associations of the Spanish Society of Cardiology on the management of invasive cardiac procedure rooms during the COVID-19 coronavirus outbreak. REC Interv Cardiol. 2020.https://doi.org/10.24875/RECICE.M20000116.
3. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507-513.
4. Lippi G, Lavie CJ, Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): Evidence from a meta-analysis. Prog Cardiovasc Dis. 2020. https://doi.org/10.1016/j.pcad.2020.03.001.
5. Hu H, Ma F, Wei X, et al. Coronavirus fulminant myocarditis saved with glucocorticoid and human immunoglobulin. Eur Heart J. 2020. https://doi.org/10.1093/eurheartj/ehaa190.
6. Roffi M, Patrono C, Collet JP, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016;37:267-315.
7. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J. 2019;40:237-269.
8. Di Marco A, Anguera I, Rodriguez M, et al. Assessment of Smith Algorithms for the Diagnosis of Acute Myocardial Infarction in the Presence of Left Bundle Branch Block. Rev Esp Cardiol. 2017;70:559-566.
9. Lemkes JS, Janssens GN, van der Hoeven NW, et al. Coronary Angiography after Cardiac Arrest without ST-Segment Elevation. N Engl J Med. 2019;380:1397-1407.
10. Mehta SR, Wood DA, Storey RF, et al. Complete Revascularization with Multivessel PCI for Myocardial Infarction. N Engl J Med. 2019;381:1411-1421.
11. Thiele H, Akin I, Sandri M, et al. One-Year Outcomes after PCI Strategies in Cardiogenic Shock. N Engl J Med. 2018;379:1699-1710.
12. University of Liverpool. Interactions with Experimental COVID-19 Therapies. Disponible en: https://www.Covid19-druginteractions.org. Consultado 17 Mar 2020.