ABSTRACT
Primary percutaneous coronary intervention (pPCI) is the best modality of reperfusion in ST segment elevation in acute myocardial infarction (STEMI). Its application requires networked assistance systems whose implementation requires significant organizational and logistical changes. In comparison with other scenarios of urgent action, a series of aspects are specific to the pPCI programs. They require immediate, clearly pre-established strategies, carried out by highly skilled professionals who attend to a high volume of highly complex patients. The lack of homogeneity in the creation and development of reperfusion programs in Spain has led to great differences in their implementation. If the pPCI programs are not carried out under adequate conditions, their sustainability can be complex. The present document, agreed between different scientific societies, aims to analyze the current situation in Spain of the network care programs for STEMI, identify their limitations and deficiencies, assess their vulnerability and establish a series of recommendations to ensure their sustainability.
Keywords: ST-segment elevation acute myocardial infarction. Primary percutaneous coronary intervention. Requirements. Medical emergency systems. Program sustainability.
RESUMEN
El intervencionismo coronario percutáneo primario (ICPp) es la mejor forma de reperfusión en el infarto agudo de miocardio con elevación del segmento ST (IAMCEST). Su aplicación requiere sistemas asistenciales en red cuya implementación exige cambios organizativos y logísticos importantes. En comparación con otros escenarios de actuación urgente, una serie de aspectos son específicos de los programas de ICPp. Requieren de estrategias inmediatas claramente preestablecidas, realizadas por profesionales muy expertos y que atienden a un elevado volumen de pacientes de alta complejidad. La falta de homogeneidad en la creación y desarrollo de los programas de reperfusión en España hallevado a grandes diferencias en su implantación. Si los programas de ICPp no se efectúan en condiciones adecuadas su sostenibilidad puede ser compleja. El presente documento, consensuado entre diferentes sociedades científicas, tiene por objetivos analizar la situación actual en España de los programas de atención en red al IAMCEST, identificar sus limitaciones y deficiencias, evaluar su vulnerabilidad y establecer una serie de recomendaciones para asegurar su sostenibilidad.
Palabras clave: Infarto agudo de miocardio con elevación del segmento ST. Intervencionismo coronario percutáneo primario. Requisitos. Sistemas de emergencias médicas. Sostenibilidad de los programas.
Abbreviations: AACC: autonomous communities. STEMI: ST-segment elevation acute myocardial infarction. PPCI: primary percutaneous coronary intervention. SEC: Spanish Society of Cardiology. MES: medical emergency system. CICU: cardiac intensive care unit.
INTRODUCTION
Ischemic heart disease is still the leading cause of mortality worldwide and it amounts to up to 20% of the overall deaths in Europe.1 The ST-segment elevation acute myocardial infarction (STEMI) is one of the most relevant forms of presentation. Early reperfusion is the most effective way to reduce morbimortality in STEMI. It was soon confirmed that fibrinolysis could not reestablish the patency of the coronary artery found in up to 20%-45% of patients2 with a 5%-10% acute coronary re-occlusion after successful fibrinolysis and a rate of late occlusion close to 30%.3 Primary angioplasty or more precisely, primary percutaneous coronary intervention (pPCI) did obtain significantly higher success rates in reperfusion above 90%,4 which is associated with a 30% relative reduction in mortality rate at 30 days and a lower risk of reinfarction and stroke.5 For this reason, pPCI became the gold standard treatment for the management of STEMI. However, the benefit of pPCI over fibrinolysis is only evident when performed at adequate centers by experienced teams (infarction centers) and within the first 120 minutes after the first medical contact.6
The pPCI not only is more effective and safer compared to fibrinolysis but recent studies show that it is cost-effective from the socioeconomic point of view, regardless of the initial high cost of its logistical and technological implementation.7,8 In a study conducted in the United States,9 reperfusion through pPCI was associated with lower hospital costs initially compensated with the higher personnel costs (on call 24/7); however, when used in large volumes of patients, the pPCI was much more cost-effective. This higher cost-effectiveness is the product of eliminating the cost of fibrinolysis, the lower incidence of ischemic and hemorrhagic complications, the lower need for coronary angiographies and ischemia detection imaging modalities, the shorter initial hospital stay due to readmissions, and patients’ early return to professional life.
In an attempt to offer the best reperfusion strategy to the highest number of patients and within the recommended timeframes, several scientific societies recommended the creation of STEMI care network systems in the community and regional settings to provide the fastest possible healthcare to these patients.6 However, the implementation of these reperfusion networks requires important organizational and logistical changes. And this is a complex situation in Spain since the allocation of resources from the different healthcare administrations of the 17 autonomous communities (AACC) is decentralized and, therefore, budgets are managed independently. The organization and implementation of the healthcare system is also decentralized in this system. This leads to the heterogeneous provision of services. The way pPCI networks work and the results obtained from these networks are highly influenced by several factors such as geography, the number of pPCI-capable centers, referral times, the availability of adequate resources, infrastructure, and the characteristics of healthcare systems per se.10 Similarly, the heterogeneity of the financial situation and the structures of the different healthcare systems have led to great inequalities in the ways these networks have been organized; differences noticeable not only among different countries, but also among different geographical areas within the same country.10-13 All these aspects translate into challenges and threats when it comes to the optimal implementation of STEMI care systems in Spain and they should be studied and analyzed in search of proposals and solutions that meet their needs.
This document has been agreed by different scientific societies (table 1) with the following goals in mind:
Table 1. Scientific societies, working groups, and representatives that have participated and signed the consensus document
| Representative | Society |
|---|---|
| Ángel Cequier | Spanish Society of Cardiology (SEC) |
| Armando Pérez de Prado | Working Group on Hemodynamics and Interventional Cardiology of the SEC |
| Ana Belén Cid | Working Group on Hemodynamics and Interventional Cardiology of the SEC |
| Javier Martín-Moreiras | Working Group on Hemodynamics and Interventional Cardiology of the SEC |
| Oriol Rodríguez-Leor | Working Group on Hemodynamics and Interventional Cardiology of the SEC |
| José Ramón Rumoroso | Working Group on Hemodynamics and Interventional Cardiology of the SEC |
| Ana Serrador | Working Group on Hemodynamics and Interventional Cardiology of the SEC |
| Raúl Moreno | Working Group on Hemodynamics and Interventional Cardiology of the SEC |
| Sergio Raposeiras | Working Group on Ischemic Heart Disease and Acute Cardiac Care of the SEC |
| Albert Ariza | Working Group on Ischemic Heart Disease and Acute Cardiac Care of the SEC |
| Esteban López de Sá | Working Group on Ischemic Heart Disease and Acute Cardiac Care of the SEC |
| Andrés Íñiguez | SEC |
| José Luis López Sendón | SEC |
| Francisco Javier Delgado | Spanish Association of Nursing in Cardiology |
| Rocío Gil Pérez | Spanish Association of Nursing in Cardiology |
| José Julio Jiménez- Alegre | Spanish Society of Emergency Medicine |
| Manuel José Vázquez | Spanish Society of Emergency Medicine |
| José Manuel Flores | Spanish Society of Emergency Medicine |
| Héctor Bueno | SEC |
| Manuel Anguita | SEC |
Analyze the actual situation of reperfusion-based STEMI care programs in Spain.
Identify the limitations and deficiencies of such programs.
Assess their vulnerabilities and sustainability. Establish a series of recommendations on the needs for personnel, infrastructures and incentives required for their optimization.
Achieve agreed consensus from the different scientific societies involved in the management and treatment of patients with STEMI.
Establish a combined national registry of all the actual pPCI programs.
ORGANIZATION OF HEALTHCARE NETWORKS FOR THE MANAGEMENT OF REPERFUSION IN SPAIN
Initial experiences and progress made by healthcare networks
The first experiences with structured programs of reperfusion with pPCI for the management of patients with STEMI in Spain date back to 2000 to 2001 in the Community of Navarre and the Region of Murcia, respectively where all patients were referred to a single reference center.14 The first multicenter program started in Galicia back in 2005. A series of centralized pPCI programs were defined then where geographical location-based isochrones were categorized, the healthcare centers where patients should be referred to were identified, and the healthcare and transfer resources needed were described. From early on, it was evident that these networks determined an increase in the number of STEMI patients treated with the best reperfusion therapy available at the time.15
Back in the year 2008, the AACC of Murcia, Navarre, Galicia, and the Balearic Islands had already implemented network structures that, at that time, meant that 12.8% of the Spanish national territory was covered. That same year, the Stent for Life initiative was born, a European project implemented by the European Association of Percutaneous Cardiovascular Interventions, and designed by interventional cardiologists, health Administration officials, patients, and healthcare industry providers. The goal of this initiative was to stimulate and facilitate the implementation of healthcare networks that would allow any STEMI patient to have access, in the least amount of time possible, to reperfusion therapy through pPCI. Spain started collaborating in this program back in 2009 in an attempt to identify regions with implementation deficiencies and to promote the elimination of barriers responsible for delays in the healthcare process. The project was based on prior experiences in the development of new projects. Also, it was decided to create and maintain reliable activity registries with campaigns aimed at training the population and making health authorities more sensitive to this issue.16 Nowadays, this initiative is called Stent, Save a Life and it has been brought to other continents to promote the development of healthcare networks in developing counties.
In 2009, Catalonia established its own pPCI and 3 years later, in 2012 Asturias, Cantabria, and Castile-La Mancha followed. Then, it would be the turn for Madrid, Valencia, Aragon, La Rioja, and the Basque Country. All these AACC have active regional programs generically known as Infarction Code. These changes in the reperfusion strategies reduced significantly the rates of thrombolysis, while the percentage of patients treated with pPCI increased gradually with an increase of territory coverage and number of interventions performed accross the country10,17 which is consistent with what was already happening in other European countries.18
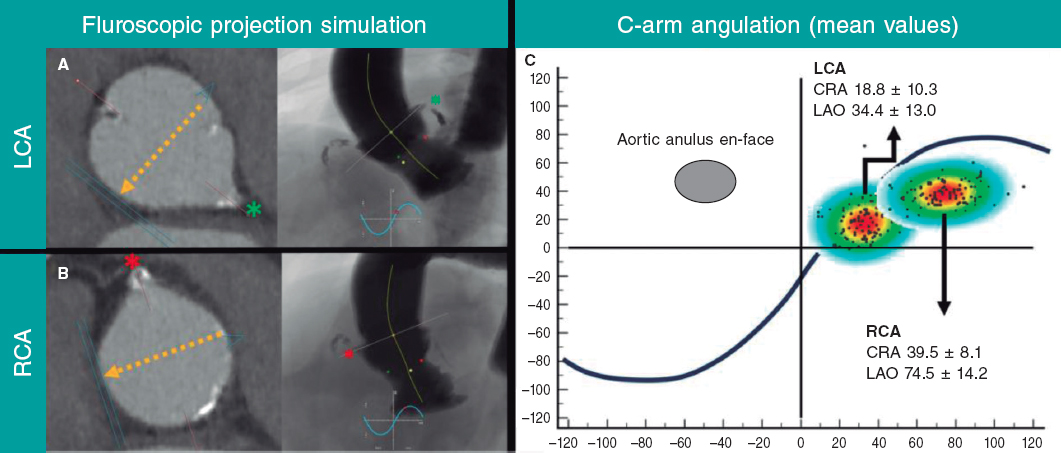
Numerous experiences have been reported that exemplify the benefits of implementing STEMI care networks, both in the European19 and domestic settings.20 One study10 analyzed the connection between the implementation of reperfusion networks for the management of STEMI in AACC, the regional rate of pPCI and hospital mortality. Throughout the entire period studied, there was a higher rate of pPCIs in all AACC (54.5% in 2012 vs 21.6% in 2003) (figure 1). It was confirmed that crude mortality rate was higher in non-reperfused patients (17.3%) compared to patients who had undergone pPCIs (4.8%) or fibrinolysis (8.6%; P < .001), with a lower risk-adjusted standardized mortality ratio (of 10.2% in 2003 and 6.8% in 2012; P < .001). In sum, the implementation of reperfusion networks was associated with a 50% increase in the rate of pPCIs and a 14% reduction in mortality rate (figure 2).
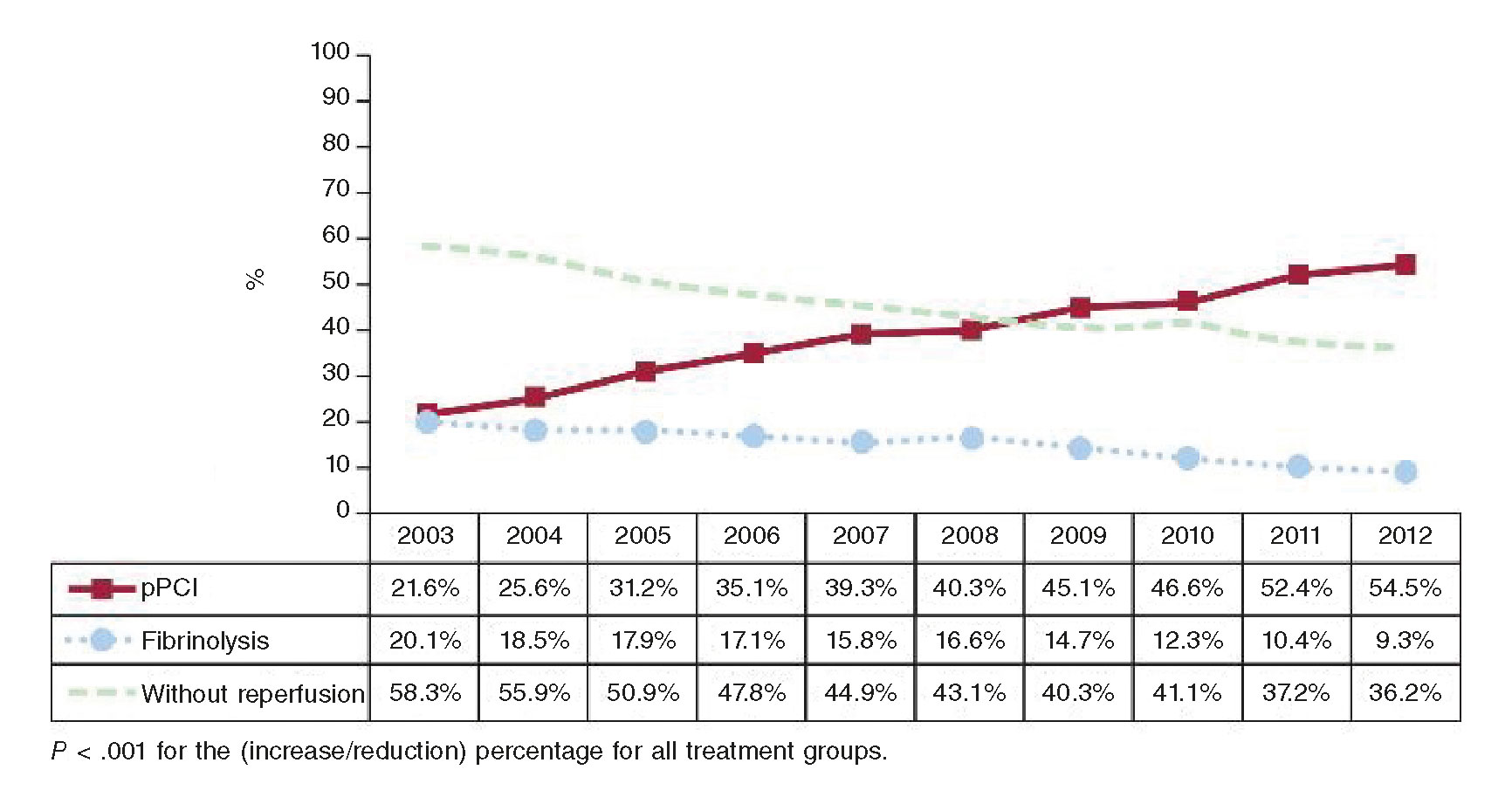
Figure 1. Changes in reperfusion strategies for the management of ST-segment elevation acute myocardial infarction in the Spanish health public system between 2003 and 2012. The evolution of reperfusion strategies can be seen over the entire study period. The percentage of patients treated with primary percutaneous coronary interventions (pPCI) increased gradually and simultaneously with moderate drops in the rate of thrombolysis. (Reproduced with permission from Cequier et al.10)
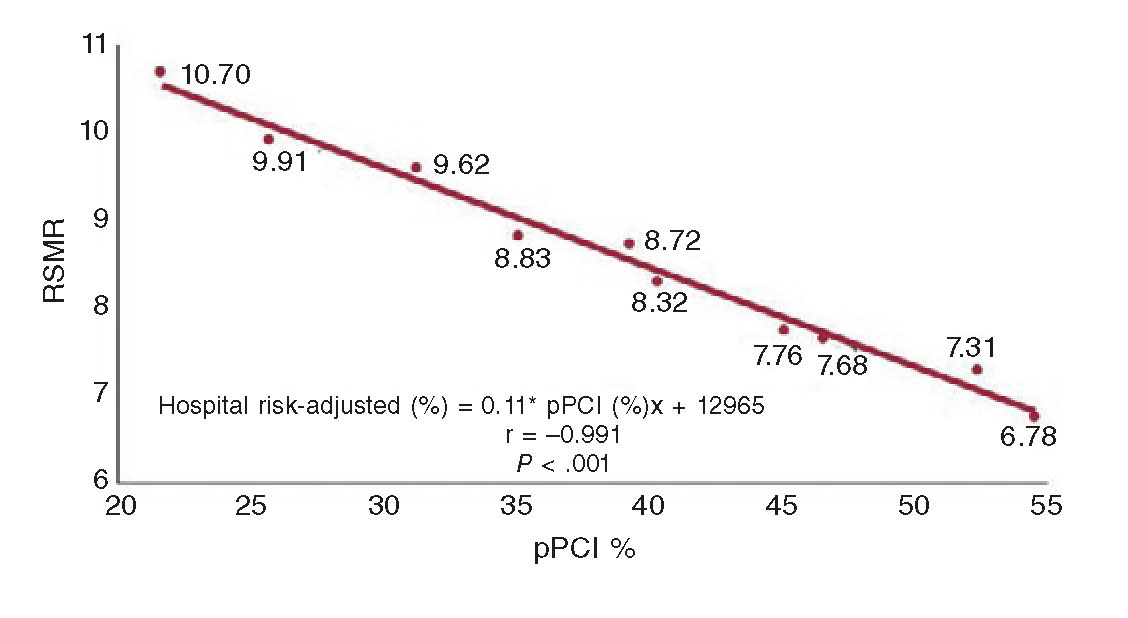
Figure 2. Correlation between the rates of primary percutaneous coronary interventions (pPCI) and mortality in the management of patients with ST-segment elevation acute myocardial infarction in the Spanish health public system between 2003 and 2012. There was a significant correlation between the rates of pPCI and mortality over the entire study period. RSMR, risk-standardized mortality rate. (Reproduced with permission from Cequier et al.10)
Reperfusion networks in Spain: current situation
Situation of the pPCI networks
Over the last few months, we have been able to provide coverage to the entire Spanish territory through regional healthcare net- works for the management of STEMI patients. In some cases, these pPCI programs do not have fully structured regional networks and depend on local circuits limited to a certain number of hospitals. Taking all these aspects into consideration, the number of per population-pPCIs has changed dramatically in our country, with a reduced number of patients treated with pPCI in AACC that did not have complete and structured programs before17 (figure 3). Consequently, the lack of homogeneity in the creation and development of the different reperfusion programs in the different AACC has brought many differences to these programs, some of them created exclusively by healthcare providers themselves with almost no institutional support. Also, other programs have seen the involvement of the Administration with detailed analyses of subdivisions, logistics, and infrastructure, and the provision of all necessary resources. This has originated a significant heterogeneity in the structure and organization of the different programs and in the assessment of different quality indicators and results. The information available shows that establishing a systematic and organized pPCI program makes a very favorable impact on prognosis compared to having unstructured pPCI programs without a preestablished transfer logistics20 (figure 4). Since there is not such a thing as a national pPCI registry, we do not know what the real volume of activity is in these programs or under what quality standards they have been implemented. Recent initiatives started by the Spanish Society of Cardiology (SEC) aim at promoting healthcare and evaluating the results of STEMI care (SEC-CALIDAD).21
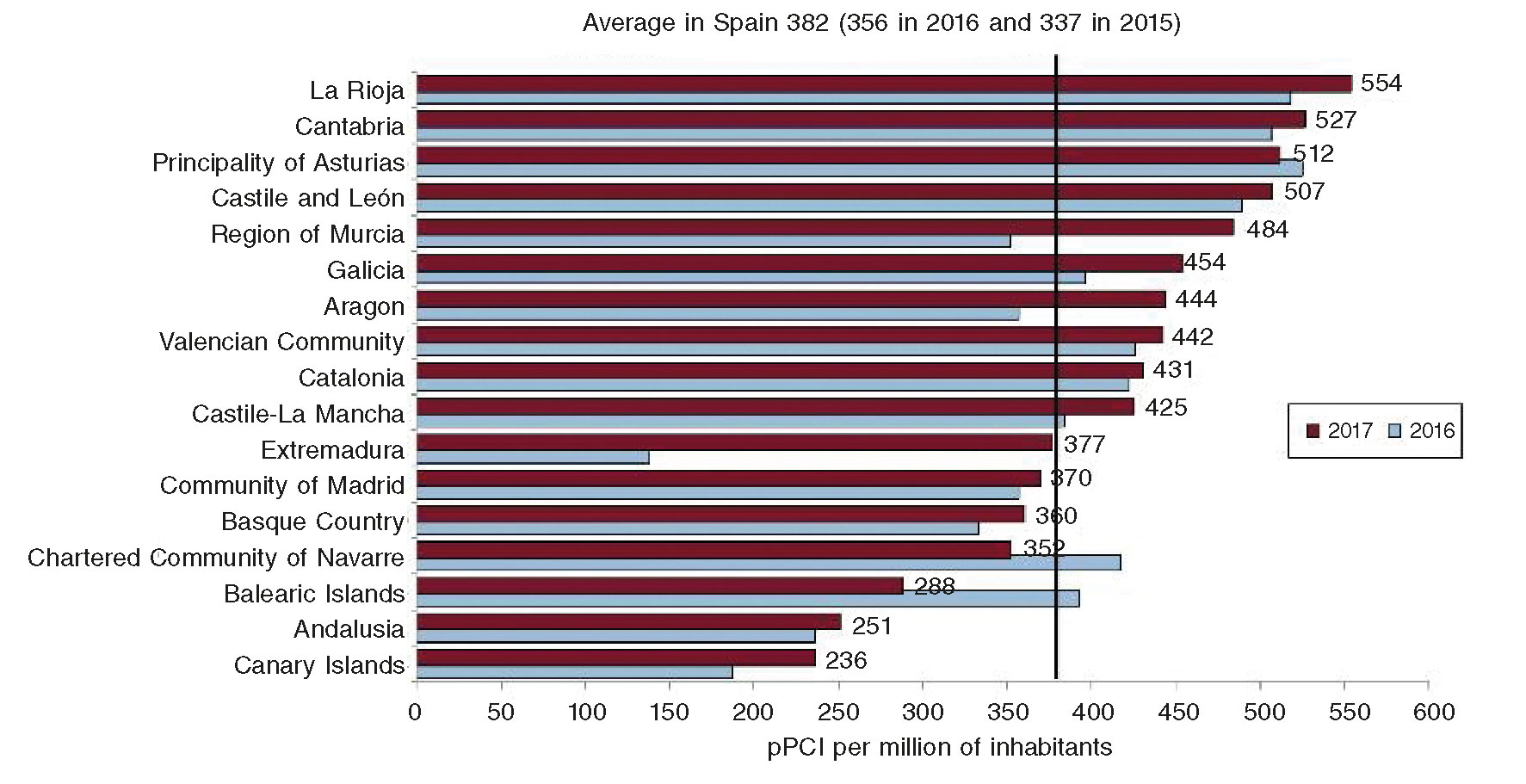
Figure 3. Primary percutaneous coronary interventions (pPCI) per million of inhabitants over the years 2016 and 2017 in all Spanish autonomous communities. Those communities without fully structured network programs (Andalusia, Canary Islands, and Extremadura back in 2016) show the lowest number of patients with ST-segment elevation acute myocardial infarction treated with pPCI (Reproduced with permission from Cid Álvarez et al.17)
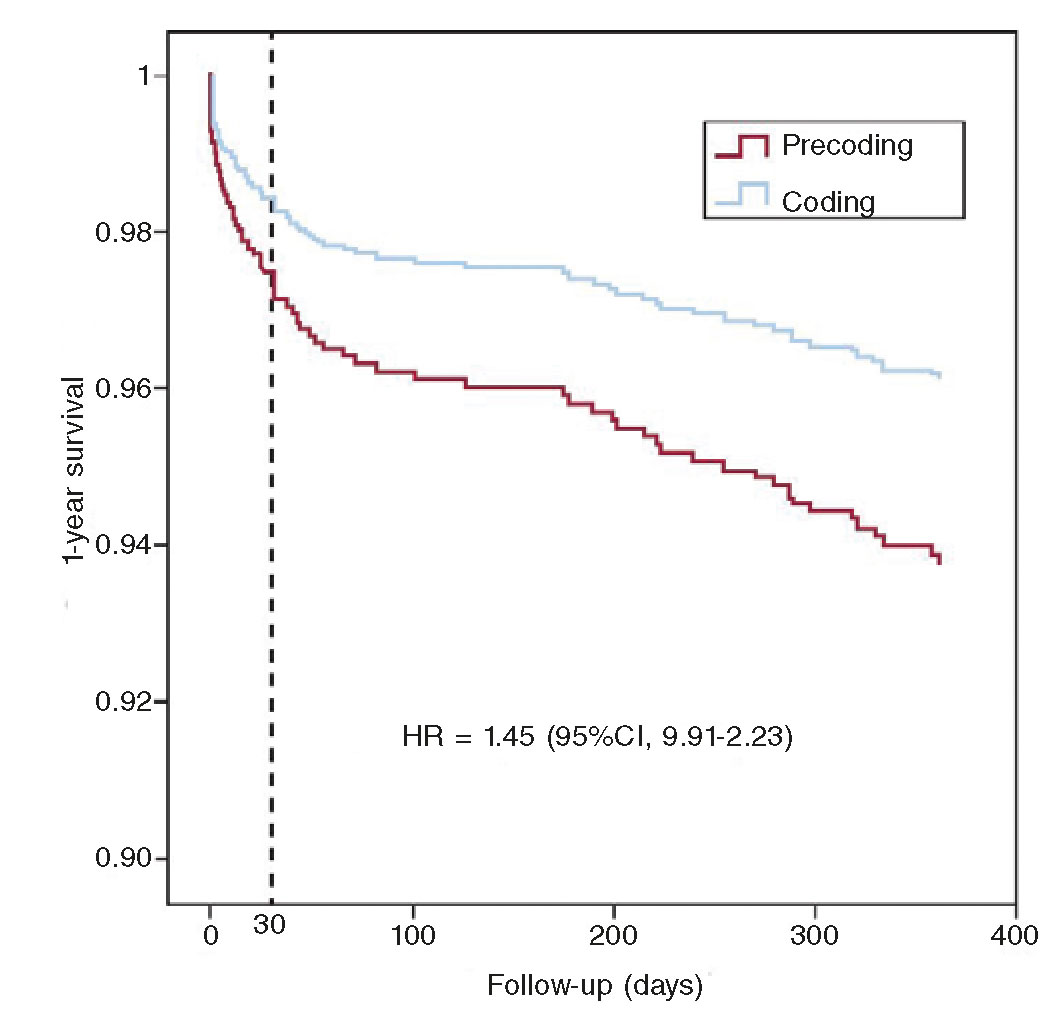
Figure 4. Prognostic impact of patients from a primary percutaneous coronary intervention (pPCI) program in a subdivided region before (precoding) and after (coding) the implementation of pre-established intervention and transfer logistics measures with regional hospitals and emergency medical services. There is a significant improvement of survival rate over the first year after implementation. (Reproduced with permission from Gómez- Hospital et al.20)
Situation of healthcare providers conducting pPCIs
In an effort to obtain information on how the actual pPCI programs work in Spain, in May 2018 the Working Group on Hemodynamics and Interventional Cardiology of the SEC conducted a survey among all its members called Needs and requirements of primary angioplasty program: a professional survey (O. Rodríguez-Leor, personal information). The questionnaire collected information on the activity of the programs already running in all the centers and on the degree of satisfaction of the personnel involved. Out of the 390 interventional cardiologists surveyed, 172 (44%) filled in the questionnaire. The mean age of respondents was 45 ± 8 years old (interquartile range: 39-50 years) and they all had over 9 ± 6 years of experienced managing primary angioplasty programs. The centers performed an average 292 procedures per year (200-410). All AACC were represented in this survey.
A very important aspect was that 45% of the respondents were not getting any breaks after night code activations. In almost half of the cases of those who actually got a break, they did not have access to their resting hours the next day because these hours had to be adjusted to the actual logistics needs or volume of activity of their department (figure 5). Another remarkable aspect is that over 50% of the respondents said their intention was to stop doing night calls whenever they were eligible due to their age (figure 6A). On the other hand, a high percentage of respondents (85%) said that the management of patients had room for improvement within their actual programs (figure 6B).
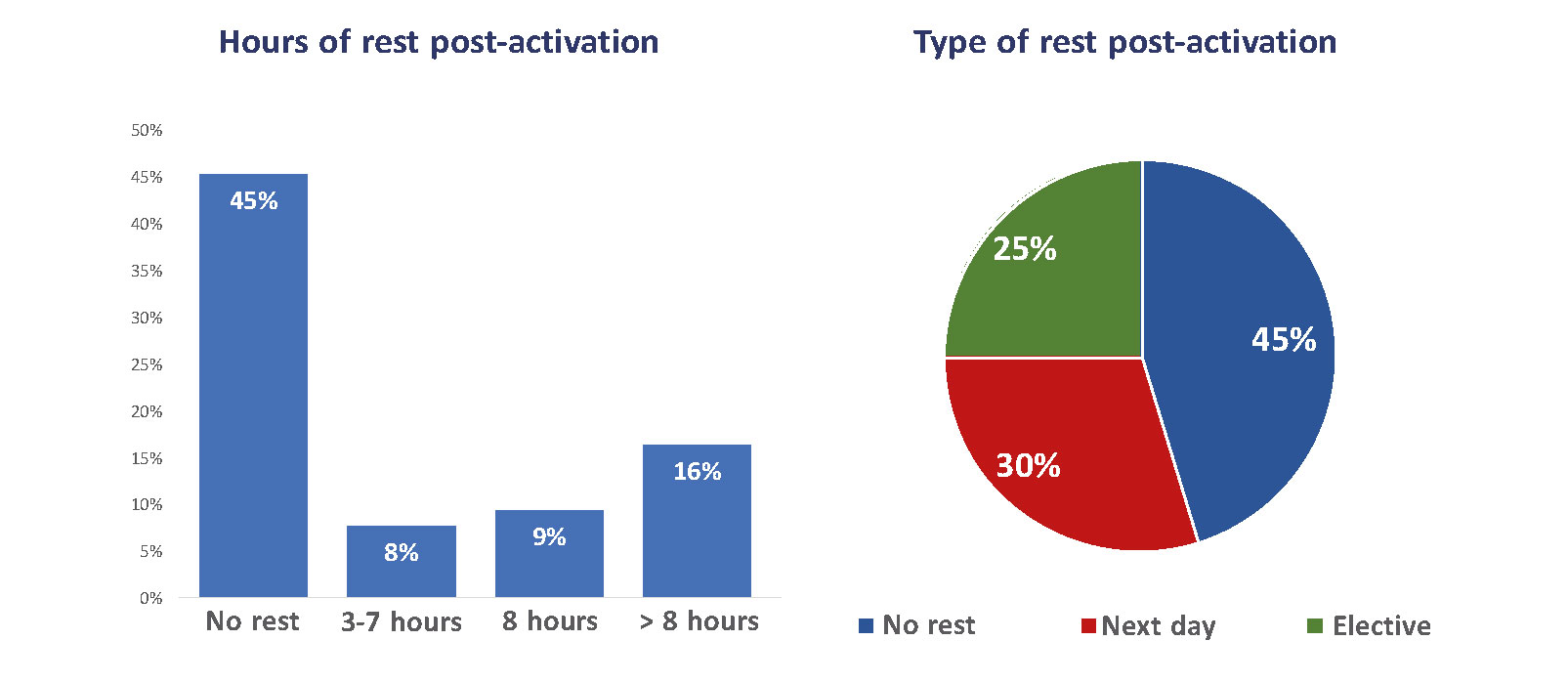
Figure 5. Hourly schedules and types of rest after being activated to perform primary percutaneous coronary interventions during night shift. Only 25% take a break of at least 8 hours after performing this procedure. Forty-five percent immediately move on to their routine clinical practice the next day with no downtime. (Data gathered from a survey conducted among members of the Working Group on Hemodynamics and Interventional Cardiology of the Spanish Society of Cardiology.)
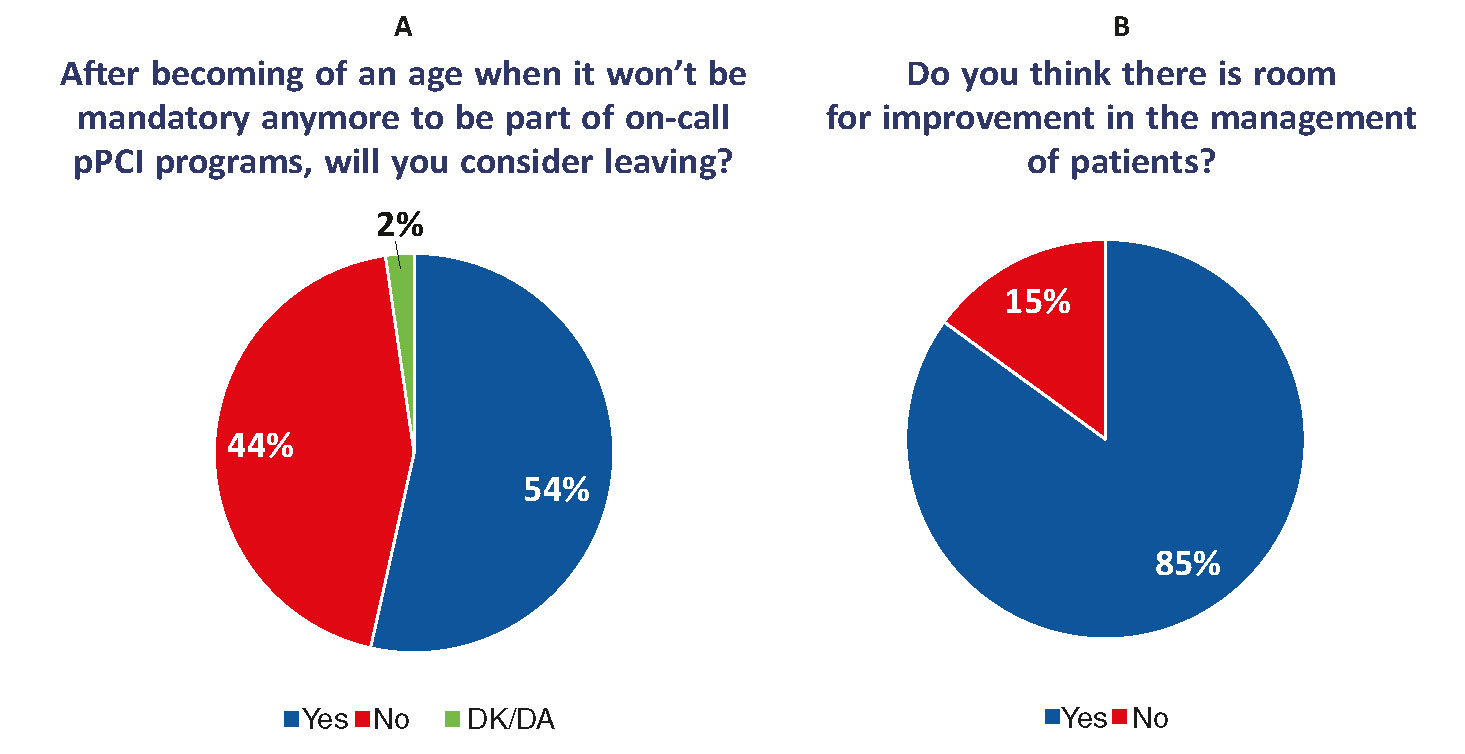
Figure 6. A: Willingness to remain available or leave the on-call primary percutaneous coronary intervention (pPCI) programs after no longer being mandatory due to age. Fifty-four percent of respondents will leave these programs. B: Answers to the question of whether respondents thought that there was room for improvement for the management of patients with ST-segment elevation acute myocardial infarctions within pPCI programs. Eighty-five percent said that there was room for improvement. (Data gathered from a survey conducted among members of the Working Group on Hemodynamics and Interventional Cardiology of the Spanish Society of Cardiology.) DK/DA, did not know/did not answer.
Back in 2012-2013, another survey was conducted among the nurses of 52 centers that showed that in 64% of the cases, those who had been on call did not have any time to rest, and only 7% had access to some sort of rest over the next 12 hours (V. Rodríguez, personal information). Eighty-four percent of respondents did not get any time in lieu.
The results from these surveys should make us think of the future threats and risks of the actual models of human resources in certain pPCI programs.
SPECIFICITIES OF pPCI PROGRAMS
The particular characteristics and specific requirements of pPCI programs can put them in a scenario of vulnerability that will gradually make it very difficult to keep their sustainability if these programs are not implemented under the right conditions from the point of view of structure, organization, human resources, and equipment.
One of the key aspects of pPCI is the immediacy of the healthcare provided. In STEMI patients there is a direct correlation between the time the artery has remained occluded and early and long-term morbimortality. The occluded artery should be opened as soon as possible, which is why the time elapsed since the patient is first assisted until the artery is opened is a critical factor to determine the effectiveness of the procedure and results.22,23 Although time limit when it comes to selecting the optimal reperfusion strategy (pPCI vs fibrinolysis) is 120 minutes, the recommendations of the clinical practice guidelines established by the European Society of Cardiology have become more and more demanding. They indicate that the maximum amount of time that should elapse since the diagnosis of STEMI is established until angioplasty guidewire crossing should not exceed 60 minutes in patients admitted to pPCI-capable centers, and should not exceed 90 minutes in patients transferred from other centers.6 A pPCI program should guarantee achieving diagnoses immediately, conducting urgent transfers and interventional procedures in a short span of time. The implementation of a pPCI program requires close collaboration of all teams involved in the healthcare system (primary care, regional hospitals, emergency rooms, emergency systems and transfers, and infarction centers).
Compared to other urgent care settings, even high-risk settings, there is a series of aspects exclusive and specific to pPCI programs:
They require immediate healthcare that should be perfectly coordinated among the different levels of healthcare with clearly preestablished strategies and logistics and conducted by experienced teams. The teams involved should be on call 24/7, and ready to act as swiftly as possible when required, without a preestablished schedule, and in less than a 60-90-minute timeframe after activation.
The transfer of patients to the corresponding infarction centers should have top priority over all other types of emergencies or procedures.
Patients have a high mortality risk and they usually need complex healthcare actions, so an adequate infrastructure is required.
The volume of STEMI patients with an indication for pPCI is very high.
The following features define the landmarks for a healthcare network system to be successful in the management of STEMI patients:
Establish a clear-cut definition of the corresponding geographical regions.
Have a written, agreed, and common protocol available for all healthcare providers involved.
Make sure that the transfer of patients is conducted by accredited professionals with a well-established level of competence and on adequately equipped-means of transportation (ambulances or helicopters), that is, through the appropriate systems of medical emergencies.
Facilitate immediate transfers to pPCI-capable centers. In cases where diagnosis is achieved out of the infarction center setting, the transfer to the hospital should be direct, without stops or re-evaluations in non-pPCI capable hospitals.
Upon arrival at the infarction center, the patient should be immediately transferred to the cath. lab and without any prior stops at the ER.
If a patient is initially assisted at a non-pPCI capable center, he should be evaluated in a monitored area by experienced personnel. If the patient is to be transferred to an infarction center to undergo the pPCI, then the time elapsed from diagnosis until the patient leaves the center should not exceed 30 minutes.
REQUIREMENTS AND NEEDS FOR THE RIGHT DEVELOPMENT OF pPCI HEALTHCARE NETWORKS
Subdivisions. Geographical regions
Spain is the fourth largest country in Euope, yet its population density is lower than most Western European countries, with a very irregular territorial distribution. This circumstance, especially in healthcare network systems makes it difficult to provide similar health coverage in the entire territory. In order to solve this problem, it is important to subdivide healthcare into geographical regions where healthcare to patients can be provided effective and homogeneously. Although certain recommendations have already been established by the European Society of Cardiology on what the reference population should be per cath. lab, its implementation in the pPCI setting is much more complex. Initially, a subdivision based on time isochrones is required so access to pPCI is guaranteed from the different healthcare providers to the largest amount of patients possible with transfer times within the timeframes recommended by the clinical practice guidelines, but only towards adequately equippedinfarction centers capable of performing a minimal number of pPCIs each year.24 The geographical barriers among different AACC should not be an obstacle for transfer logistics, since patients with an indication for pPCI should be transferred to the closest infarction center. Prior administrative agreements signed by the AACC involved should be taken into consideration. Patients who live in remote areas or who due to logistics or climate issues cannot undergo pPCI within the timeframe recommended should be treated as soon as possible with fibrinolysis and then transferred to infarction centers so that the pharmaco-invasive strategy can be initiated.25,26
Logistics-related aspects. Communications systems
To achieve these goals, logistics requires a 100% committment from all healthcare providers involved, particlularly from the transfer systems. It is important to have agile communication systems from a centralized structure (emergency coordination centers) capable of promptly notifying the infarction centers on the arrival of a patient, the transfer estimate time, and the patient’s clinical state so that the receiving center can adapt its daily activity to the arrival of an unexpected urgent procedure.24 Some programs include patients’ clinical description and electrocardiogram results before activation, thereby reducing the amount of diagnostic mistakes. On rare occasions, when several patients need to be transferred to the same center at the same time, or when the receiving center is busy with uncancellable activities, patients should be transferred to other close-by infarction center capable of providing the healthcare required.
Medical emergency systems
Medical emergency systems (MES) with doctors aboard the ambulance are a reality in Spain; however, the decentralization and transfer of health competences to the different AACC has generated different healthcare models. In the pPCI programs, MESs should be easily accessed over the phone through emergency coordination centers capable of triaging the urgent care requested. This request for help can come from private households, the street, or primary hospital or care centers. Afterwards, MESs activate the units that provide initial care and, if required, the transfer of the patient to the infarction center. Emergency coordination centers should have STEMI categorized as a time-dependent condition that requires priority care to achieve better results.24 Within the pPCI program setting, emergency coordination centers should meet a series of prerequisites and have:
A system capable of taking calls that will not collapse.
A computer system capable of recording the time of call, preliminary medical examination, type of resources allocated, the time these resources were allocated, activation time of the healthcare unit, arrival time to the place help was requested from, and timeframes of initial transfer and final arrival at destination.
A multidisciplinary team including phone dispatchers, nurses, doctors, and technicians trained in the management of telephone calls.
A periodic quality re-assessment protocol of the different components of the care provided.
The care provided to STEMI patients should be initiated by the first medical team available with the aim to examine the patient and interpret the electrocardiogram in less than 10 minutes. If diagnosis is confirmed, the corresponding healthcare protocol should be activated, and the patient transferred to a pPCI-capable center. A complete transfer of information on the patient’s clinical situation among the healthcare unit, the emergency coordination center, and the destination hospital is crucial. This approach should also be used with patients initially assisted in non-pPCI capable centers.6,24
The initial transfer of these patients should happen in MES mobile units with teams including physician, nurse and paramedics trained and accredited according the level of competence established. The receiving hospital should know what the estimated time of arrival should be able to organize the care to be provided (on business hours) or to activate the treating hemodynamics team (off business hours). The patient should be transferred directly to the cath. lab without stopping at the ER.6,24
It is essential that the MES team writes down a complete medical report including the aforementioned timeframes, the initial assessment, the interpretation of electrocardiograms, the medication administered, the patient’s progression, and any other complications that may arise. These teams should conduct periodic quality assessments of the healthcare provided to detect possible ways to improve this process. A system for the periodic exchange of information between the MESs and the hospitals treating the patients transferred should be established to analyze the quality and observance of the plans of action previously agreed on. There should always be MES resources available based on the established population ratios.
Infrastructure and equipment
The pPCI-capable interventional cardiology units and the cardiology services and centers where these units are headquartered should meet structural, functional, and organizational requisites to guarantee safety, quality, and efficiency conditions to perform such procedures. The following quality standards and accreditation criteria for reference units on the performance of pPCIs procedures27 and the standards and criteria that regulate the entire STEMI process have been recently agreed upon and published by the SEC (SEC-EXCELENTE):21
The receiving pPCI unit should have a protocol agreed by the hospital board of directors.
This unit should design and implement a training program including continuous practical training for its staff.
The pPCI reference units should guarantee non-stop 24/7 all year round full medical coverage. Units with 12-hour-day programs are acceptable but not recommended and only if the MES coordination system incorporates clear-cut criteria on the transfer of STEMI patients based on hourly availability.
As well as the standard equipment including ventilators, the cath lab should also have circulatory support systems, intra- aortic balloon counter-pulsation systems, electro-catheters, external pulse generator units, and a fully equiped crash cart to be able to perform advanced resuscitation maneuvers in the context of a patient with STEMI and its possible complications.
The hospital where the pPCI unit is headquartered should have the following services available:
– It is advisable to have a cardiac intensive care unit (CICU) or general intensive care unit (ICU) available capable of providing level-2 and level-3-care according to the standards established by the Acute Cardiovascular Care Association28 and meeting the standards recommended for this type of units.29
– Cardiac surgical services. In units that do not offer this service within the same hospital, a formal agreement signed with a nearby cardiac surgical service should be available for the quick transfer (< 60 minutes) of patients who may require urgent heart surgery.30
– Hematology and blood bank service or unit.
– Diagnostic imaging service including computed tomography scan capabilities.
– Cardiologist on call on location.
Regarding CICUs, the care of patients after undergoing pPCI should be consistent with the structure and functioning of each hospital. It is advisable that the centers of pPCI receiving units have a cardiology unit-dependant CICU. The decision to hospitalize a patient should be based on the level of care required by each patient (table 2).
Table 2. Levels of care
| Level | Description of the need for healthcare |
|---|---|
| 0 | Patients whose needs can be met through normal ward care in an acute hospital |
| 1 | Patients at risk of their condition deteriorating, or those recently relocated from higher levels of care, whose needs can be met on an acute ward with additional advice and support from the critical care team |
| 2 | Patients requiring closer observation or intervention including support for a single failing organ system or post-operative care and those ‘stepping down’ from higher levels of care |
| 3 | Patients requiring advanced respiratory support alone or monitoring and support for two or more organ systems. This level includes all complex patients requiring support for multi-organ failure |
CICUs with level-2 and level-3 care should:
Have a medical and nursing responsible.
Keep a physician in charge of the unit on call and on location 24 hours/day.
Maintain the ratio of 1-2 nurses per patients requiring level-3-care and 1-3 nurses per patients requiring level-2-care.
Be fully equipped with material that meet the standards established by the clinical guidelines designed by the SEC.
Have at least two beds for every 100 000 inhabitants within the area of influence the pPCI program specifies for receiving units, and no less than six beds.
Units with level-1-care should have a nurse/patient ratio > 1:6, have the necessary equipment and material available, and meet the standards designed by the European clinical practice guidelines.6 The amount of beds recommended is nine beds for every 100 000 inhabitants within the scope of influence of the pPCI program, but it can be smaller if there is a referral program to send the patients back to their reference hospital. The amount of beds required for level-1-care is and conventional hospitalization (level-0-care) is reduced accordingly.
Human resources
The interventional cardiology units included in the pPCI network should have a 24/7, all year round service on call.6 The team on call should include:
Interventional cardiologists: during the procedure, together with the interventional cardiologist, the presence of a second physician responsible for the patient’s clinical stability is required. It is advisable that the team of a pPCI program includes at least four cardiologists accredited by the Working Group on Hemodynamics and Interventional Cardiology of the SEC.6 To achieve and maintain the training required for the management of STEMI, 30 pPCIs need to be performed per year and per operator.31 Small-volume centers should be included into wider infarction care networks.32,33
Graduate nurses: two graduate nurses trained in direct procedural care with sufficient knowledge of the equipment and material at hand are required. It is advisable that nursing staff be part of the unit and accredited in the field of hemodynamics based on defined criteria. Although the presence of an additional specialist is advisable, he should not replace the nurses in any of their fields of expertise. The participation of an assistant nurse trained in pPCI procedures is also advisable.
After activation, the time of arrival of the hemodynamics team should not exceed 30 minutes. The necessary measures to work within this timeframe should be implemented.
Post-procedural transfers. Early discharge
The transfer of patients once the pPCI has been performed is not uniform and is influenced by several aspects. Depending on the infrastructures, the personnel available, the availability of beds, the initial location of the patient after the pPCI, his clinical stability, and the level of complexity of the receiving hospital, the strategies for the management of patients post-pPCI can vary significantly. There are centers that accept and hospitalize all patients after the pPCI; others, however, keep them under observation for 12-24 hours prior to transferring them, and there are centers that transfer all patients as long as they remain stable after the pPCI.
Taking into consideration the pPCI setting and its possible complications, it is advisable that patients remain under strict observation the 12-24 hours following the procedure, preferably at the infarction center. Depending on the degree of clinical stability and the characteristics of the receiving center, patients can be transferred to their reference hospitals or remain hospitalized under observation or complete the necessary additional treatments that may be required. The models established for the transfer of patients to other centers are determined by the patient’s clinical characteristic, the applicable regional protocols, and the resources available. Patients whose procedure has had optimal results, who have undergone an adequate clinical evaluation, have no signs or symptoms compatible with persistent ischemia, do not show any traces of arrhythmia, remain hemodynamically stable, do not require vasoactive or mechanical support, and without a new revascularization scheduled are eligible for early transfers. Although some MESs already implement them, the widespread use of risk stratification indices and scores to allocate the most adequate resource for the transfer of these patients, and the systematic assessment of these indices and scores is strongly advisable.
Several studies have shown that after a successful pPCI in low-risk patients who were completely revascularized, a significant percentage of patients can be discharged from hospital to their home two or three days after the procedure. Patients eligible for early discharge after STEMI can be identified using risk scores such as the PAMI-II criteria (Second Primary Angioplasty in Myocardial Infarction), the Zwolle risk score, etc.6
Additional prerequisites of pPCI programs
The units that are part of a pPCI network should meet a series of additional requisites:
Be able to perform over 400 conventional pPCIs per year and over 75 conventional pPCIs per interventional cardiologist per year.34
Have an organizational and functions manual available that includes the actual clinical practice guidelines for the management of acute myocardial infarctions approved by SEC and procedural guidelines adapted to the unit setting.
Make available specific informed consent forms to patients and their families, explaining the characteristics of the diagnostic and therapeutic process to be performed.
Implement a specific mechanism to assess the pPCI program with indicators of process (especially timeframes) and results including complications.
Carry out a formalized process to improve the safety and quality provided to patientS and also keep a record of adverse events.
Together with the cardiology service, these units should be incorporated into a system that compares quality optimal practices (benchmarking), process indicators (especially timeframes), severity scores, complexity, and results to eventually to make comparisons with the other pPCI units.
PPCI units and the cardiology services should hold periodic meetings to systematically analyse any safety incidents that may have occurred in the unit and, especially, to establish the corresponding prevention measures.
Both should provide detailed information of all patients in order to constitute the STEMI National Registry of the Working Group on Hemodynamics and Interventional Cardiology of the SEC, quantify the activity that goes on in the Registry and for code insertion purposes, in the Basic Minimum Data and the RECALCAR Registry.
VULNERABILITIES OF THE ACTUAL pPCI PROGRAMS
Some pPCI programs were initially developed with partial or incomplete prior analyses, limited official support, and poor resources. The progressive expansion of pPCI programs and their widespread use in most STEMI patients have allowed to identify a series of deficiencies and shortfalls that may make them vulnerable and eventually jeopardize their own sustainability.
Impact on daily activity and volume-based care
According to the 2017 registry run by the Working Group on Hemodynamics and Interventional Cardiology, pPCIs amount to almost 30% of all interventional procedures performed in the cath lab.17 Data from different studies35,37 show that between 55% and 70% of all pPCI procedures are performed during off business hours (nights and weekends); however, the remaining 30%-45% procedures on STEMI patients are performed during business hours. The arrival of this large and unexpected volume of urgent and non-scheduled patients to the cath lab disturbs the scheduled daily activity of the unit since the patients require the fastest possible care these cath lab can provide. Depending on the level of adequacy that each center can establish to anticipate this, the routine activity of these cath labs may change, and cases may be suspended (ie, in-patients, cath lab scheduled patients or patients from other centers) and the usual working hours extended to avoid cancellations. Thus, optimizing the STEMI treatment may deteriorate the care that should be provided to other patients with serious heart conditions.
Psychological, legal, and economic implications in healthcare providers
The lack of appropriate sizing of the personnel involved in pPCI programs may be the reason behind two important issues: the development of psychosocial issues and the emergence of situations with legal implications. Dealing with large volumes of pPCIs during night shift requires an adequate number of healthcare providers to take on the unit activity scheduled for the next day. Both the design and makeup of the personnel of infarction centers should take this matter into serious consideration. Without an appropriate sizing of the personnel involved, staff will often have to perform elective procedures deprived of sleep and without the adequate resting time. These procedures have been associated with a higher number of suboptimal results,38 which may have legal consequences for the healthcare providers due to civil liability insurance limitations. If the pPCI procedures are performed during the night shift, an 8-hour resting period after the procedure seems like a reasonable amount of time before the staff goes back to their daily routine.
Also due to the fast action required the peculiarities of pPCI for the management of STEMI often puts a lot of stress on the healthcare providers, because of the complexity of the procedure, and the risk of complications for the patients, all of it due to the procedure per se or due to morbimortality. The variability of schedules, the required urgent action, and the immediate availability of the personnel involved determine a very particular type of “availability”. This may contribute to the higher incidence of the so-called burnout syndrome, depression and anxiety among the staff under high healthcare and emotional pressure as experienced in the cath lab.39 Added to this, there is the high incidence of trauma problems interventional cardiologists suffer39 and, in the long run and with a stochastic component, the possibility of developping certain types of neoplasms.40
In this context it should be mentioned that many pPCI programs in Spain are not categorized as individual specialty programs. Therefore, the financial retributions to these healthcare providers are no different from the retributions of other providers dealing with urgent interventions of lower complexity less frequently, in low or no risk patients and that can often be scheduled several hours in advance. All these aspects are perceived by interventional cardiologists as a mismatch that goes against their best interest. In Spain this is specifically seen in transplant programs and is probably one of the reasons that explains the level of excellence that these programs have achieved in this country.
Ignoring all these aspects can be detrimental to the teams and could in fact lead to situations of discouragement among the staff working in some of these programs. This may have negative repercussions in the level of excellence required by pPCI programs, especially taking into consideration the special profile of the patients involved. Recent data indicate that because of this many highly-experienced healthcare providers (who also happen to be those who do better) will leave these programs as soon as they are entitled due to their age. Also, in order to legally request leaving these mandatory programs, they may claim physical or psychological issues, which would be totally justified and easy to accomplish. All of this puts pPCI programs in a situation of great vulnerability.
PROPOSALS TO ENSURE THE SUSTAINABILITY OF pPCI PROGRAMS
Perfectly established subdivisions to reduce any possible delays
The national territory should be subdivided based on the nearness of hospital centers in order to make sure that the management of STEMI patients happens with the lowest possible delays. This subdivision should entertain concepts such as distance and transfer times to infarction centers. Isochrones should identify distance-related delays to these centers and delays affecting the state of communications. Patients who live in distant neighborhoods or with logistics issues should not undergo pPCI procedures within the intervals recommended; instead, they should be treated immediately with fibrinolysis, and then transferred to the corresponding cardiac center.6
Consensus strategies to reduce transfer times
Regardless of the initial level of care when the diagnosis of STEMI is achieved and when the system is activated (whether from private households, the street, primary care center or regional hospital), protocols for the transfer of patients to pPCI centers should be established. Each pPCI center should agree with the MESs and their corresponding reference hospitals on the best possible strategy to reduce the intervals of treatment. The adequate sizing of these may also be necessary to guarantee the level of care required. Agile communication systems with a centralized structure (emergency coordination center), are key if we want to establish the logistics of the entire process.
The MES emergency coordination center should prioritize the transfer of STEMI patients. Communication with the tertiary hospital through internal phone lines should be established to inform on the estimated transfer timeframe and the patient’s clinical state so that the receiving center can adapt its scheduled daily activity to the arrival of this unexpected emergent procedure. All these timeframes should be recorded prospectively to make the corresponding analysis of any delays that may have occurred during the transfer and be able to identify potential room for improvement. These protocols should be reviewed periodically on a result assessment basis.
Adequacy of pPCI-capable infarction centers
The degree of adequacy will depend on the number of pPCIs performed. The scope and benefit of the pPCI to a significant number of STEMI patients requires specific measures that should take into consideration a series of aspects that make it a particularly complex procedure. PPCI centers should be structured, organized, and properly sized to be able to handle significant increases in the number of urgent procedures. These programs should also include the transfer of patients through the entire intrahospital pathway. Several additional resources are necessary with different factors in each and every one of them:
Ensure the presence of a second physician while the pPCI is being performed.
The nursing staff should have the experience required while the pPCI is being performed. Depending on the patient’s clinical situation, additional nurses trained in cardiology care may be needed so that the interventional cardiology team can be solely committed to achieving reperfusion.
Prepare specific areas with personnel trained on the initial care of STEMI patients while they are waiting for the procedure to be performed and once it has been performed, and also additional beds in the cardiac intensive care unit depending on the volume of pPCIs to be performed.
Have large enough teams available to take on additional unscheduled urgent tasks depending on the volume of tasks to be performed.
Establish strategies to return pPCI patients to their reference hospitals in the hours following the procedure. This scenario should be protocolized based on the procedural results obtained, the patient’s clinical situation, and the characteristics of the receiving center. This approach is mandatory in centers with high pPCI volumes.
Priority phone availability versus physical presence
Physical presence of hemodynamics teams to perform pPCIs at the very hospital is an option that has always been entertained, but it is an actual reality in very few hospitals worldwide. The timeframe between activation and the opening of the artery using the appropriate strategy of phone location should not exceed 60 minutes and different studies have found no differences at all when it comes to delays in the provision of adequate care and results regardless of whether the team that performs the intervention is physically stationed at the center or is available through the phone. Additionally, considering an adequate number of interventional cardiologists per center, accredited nurses, and the remaining personnel involved in the program, the activities scheduled for the next day could be compromised if the team on call is physically stationed at the hospital, not if it is available through the phone.
Recognition and the right incentives
It is advisable to give pPCI programs a special status by taking into consideration that we are dealing with professionals with a high level of training who neeed to be available at all time, have an immediate capacity of reaction, and be available on different schedules and all at stressful settings due to the complexity of the procedures performed and the risk involved when managing this type of patients. A similar example of this is the special consideration given today to heart transplant programs.
Mandatory audited registry with periodic comparative analyses
It is essential to keep a mandatory prospective registry that includes patients’ baseline characteristics, those of the infarct, the time elapsed between symptom onset and revascularization, the procedural characteristics and the results obtained, and the patient’s clinical progression until he is discharged from the hospital (including reference centers when transferring patients during the acute phase). Both intervention times and results should be monitored periodically in every center and compared to other centers in order to guarantee the quality of the services provided and, if necessary, make the necessary adjustments. Keeping track of all this through a nationwide, verifiable, and independent registry with public data available of all the existing pPCI programs with results by sectors and centers should be mandatory in our country.
There is this pressing need to know the results of the programs implemented in different AACC. Mortality in STEMI is highly dependent on the quality of care received and comparing results among different countries, AACC and hospitals is not only a need but also an obligation that the Administration and the scientific societies should observe to keep healthcare providers and the population duly informed.
CONFLICTS OF INTEREST
R. Moreno is an Associate Editor of REC: Interventional Cardiology.
REFERENCES
1. Townsend N, Wilson L, Bhatnagar P, Wickramasinghe K, Rayner M, Nichols M. Cardiovascular disease in Europe:epidemiological update 2016. Eur Heart J. 2016;37:3232-3245.
2. Grines CL. Should thrombolysis or primary angioplasty be the treatment of choice for acute myocardial infarction?Primary angioplasty —the strategy of choice. N Engl J Med. 1996;335:1313-1316.
3. GUSTO Angiographic Investigators. The effects of tissue plasminogen activator, streptokinase, or both on coronary-artery patency, ventricular function, and survival after acute myocardial infarction. N Engl J Med. 1993;329:1615-1622.
4. GUSTO Angiographic Investigators. An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction. N Engl J Med. 1993;329:673-682.
5. Keeley EC, Boura JA, Grines CL. Comparison of primary and facilitated percutaneous coronary interventions for ST-elevation myocardial infarction:quantitative review of randomised trials. Lancet. 2006;367:579-588.
6. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation:The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119-177.
7. Aasa M, Henriksson M, Dellborg M, et al. Cost and health outcome of primary percutaneous coronary intervention versus thrombolysis in acute ST-segment elevation myocardial infarction —Results of the Swedish Early Decision reperfusion Study (SWEDES) trial. Am Heart J. 2010;160:322-328.
8. Wailoo A, Goodacre S, Sampson F, et al. Primary angioplasty versus thrombolysis for acute ST-elevation myocardial infarction:an economic analysis of the National Infarct Angioplasty project. Heart. 2010;96:668-672.
9. Stone GW, Grines CL, Rothbaum D, et al. Analysis of the relative costs and effectiveness of primary angioplasty versus tissue-type plasminogen activator:the Primary Angioplasty in Myocardial Infarction (PAMI) trial. The PAMI Trial Investigators. J Am Coll Cardiol. 1997;29:901-907.
10. Cequier A, Ariza-Sole A, Elola FJ, et al. Impact on Mortality of Different Network Systems in the Treatment of ST-segment Elevation Acute Myo-cardial Infarction. The Spanish Experience. Rev Esp Cardiol. 2017;70:155-161.
11. Alter DA, Austin PC, Tu JV, Canadian Cardiovascular Outcomes Research T. Community factors, hospital characteristics and inter-regional outcome variations following acute myocardial infarction in Canada. Can J Cardiol. 2005;21:247-255.
12. Bertomeu V, Cequier A, Bernal JL, et al. In-hospital mortality due to acute myocardial infarction. Relevance of type of hospital and care provided. RECALCAR study. Rev Esp Cardiol. 2013;66:935-942.
13. Laskey W, Spence N, Zhao X, et al. Regional differences in quality of care and outcomes for the treatment of acute coronary syndromes:an analysis from the get with the guidelines coronary artery disease program. Crit Pathw Cardiol. 2010;9:1-7.
14. Carrillo P, Lopez-Palop R, Pinar E, et al. Program of Coronary Angioplasty in Acute Myocardial Infarction in the Region of Murcia (Spain):APRIMUR Registry. Rev Esp Cardiol. 2002;55:587-596.
15. Widimsky P, Wijns W, Fajadet J, et al. Reperfusion therapy for ST elevation acute myocardial infarction in Europe:description of the current situation in 30 countries. Eur Heart J. 2010;31:943-957.
16. Feldman MF, Goicolea J, Macaya C. The Aims of the Stent-for-Life Initiative in Spain in 2010-2013. Rev Esp Cardiol. 2011;11(Supl):6-8.
17. Cid Álvarez AB, Rodríguez Leor O, Moreno R, Pérez de Prado A. Spanish Cardiac Catheterization and Coronary Intervention Registry. 27th Official Report of the Spanish Society of Cardiology Working Group on Cardiac Catheterization and Interventional Cardiology (1990-2017). Rev Esp Cardiol. 2018;71:1036-1046.
18. Kristensen SD, Laut KG, Fajadet J, et al. Reperfusion therapy for ST elevation acute myocardial infarction 2010/2011:current status in 37 ESC countries. Eur Heart J. 2014;35:1957-1970.
19. Schiele F, Hochadel M, Tubaro M, et al. Reperfusion strategy in Europe:temporal trends in performance measures for reperfusion therapy in ST-elevation myocardial infarction. Eur Heart J. 2010;31:2614-2624.
20. Gómez-Hospital JA, Dallaglio PD, Sanchez-Salado JC, et al. Impact on delay times and characteristics of patients undergoing primary percutaneous coronary intervention in the southern metropolitan area of Barcelona after implementation of the infarction code program. Rev Esp Cardiol. 2012;65:911-918.
21. Rodríguez-Padial L, Bertomeu V, Elola FJ, et al. Quality Improvement Strategy of the Spanish Society of Cardiology:The RECALCAR Registry. J Am Coll Cardiol. 2016;68:1140-1142.
22. Lambert L, Brown K, Segal E, Brophy J, Rodes-Cabau J, Bogaty P. Association between timeliness of reperfusion therapy and clinical outcomes in ST-elevation myocardial infarction. JAMA. 2010;303:2148-2155.
23. Tarantini G, Razzolini R, Napodano M, Bilato C, Ramondo A, Iliceto S. Acceptable reperfusion delay to prefer primary angioplasty over fibrin-specific thrombolytic therapy is affected (mainly) by the patient's mortality risk:1 h does not fit all. Eur Heart J. 2010;31:676-683.
24. Cequier A, Maristany J. Angioplàstia primària. Estrategies per a la seva aplicacióa diferents àmbits sanitaris. Rev Soc Catalana Cardiol. 2005;5:290-297.
25. Cantor WJ, Fitchett D, Borgundvaag B, et al. Routine early angioplasty after fibrinolysis for acute myocardial infarction. N Engl J Med. 2009;360:2705-2718.
26. Sinnaeve PR, Armstrong PW, Gershlick AH, et al. ST-segment-elevation myocardial infarction patients randomized to a pharmaco-invasive strategy or primary percutaneous coronary intervention:Strategic Reperfusion Early After Myocardial Infarction (STREAM) 1-year mortality follow-up. Circulation. 2014;130:1139-1145.
27. López-Sendón J, González-Juanatey JR, Pinto F, et al. Quality Markers in Cardiology. Main Markers to Measure Quality of Results (Outcomes) and Quality Measures Related to Better Results in Clinical Practice (Performance Metrics). INCARDIO (Indicadores de Calidad en Unidades Asistenciales del Area del Corazon):A SEC/SECTCV Consensus Position Paper. Rev Esp Cardiol. 2015;68:976-995.
28. Bonnefoy-Cudraz E, Bueno H, Casella G, et al. Editor's Choice —Acute Cardiovascular Care Association Position Paper on Intensive Cardiovascular Care Units:An update on their definition, structure, organisation and function. Eur Heart J Acute Cardiovasc Care. 2018;7:80-95.
29. Palanca I, Elola FJ, Bernal JL, Paniagua JL. Unidad de cuidados intensivos. Estándares y recomendaciones. Agencia de Calidad del SNS. Madrid:Mi-nisterio de Sanidad y Política Social;2009.
30. Dehmer GJ, Blankenship JC, Cilingiroglu M, et al. SCAI/ACC/AHA Expert Consensus Document:2014 update on percutaneous coronary intervention without on-site surgical backup. J Am Coll Cardiol. 2014;63:2624-2641.
31. Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention:a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation. 2011;124:e574-651.
32. Tubaro M, Danchin N, Goldstein P, et al. Pre-hospital treatment of STEMI patients. A scientific statement of the Working Group Acute Cardiac Care of the European Society of Cardiology. Rev Esp Cardiol. 2012;65:60-70.
33. Nuñez Gil IJ, Fernández-Ortiz A, Escaned J, et al. Long term experience with a novel interventional cardiology network model:Learned lessons. J Hos Administ. 2016;5:87-94.
34. Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40:87-165.
35. Dharma S, Dakota I, Sukmawan R, Andriantoro H, Siswanto BB, Rao SV. Two-year mortality of primary angioplasty for acute myocardial infarction during regular working hours versus off-hours. Cardiovasc Revasc Med. 2018;19:826-830.
36. Graham MM, Ghali WA, Southern DA, Traboulsi M, Knudtson ML;APPROACH Investigators. Outcomes of after-hours versus regular working hours primary percutaneous coronary intervention for acute myocardial infarction. BMJ Qual Saf. 2011;20:60-67.
37. Siudak Z, Rakowski T, Dziewierz A, et al. Primary percutaneous coronary intervention during on- vs off-hours in patients with ST-elevation myocardial infarction. Results from EUROTRANSFER Registry. Kardiol Pol. 2011;69:1017-1022.
38. Sandoval Y, Lobo AS, Somers VK, et al. Sleep deprivation in interventional cardiology:Implications for patient care and physician-health. Catheter Cardiovasc Interv. 2018;91:905-910.
39. Klein LW, Miller DL, Balter S, et al. Occupational health hazards in the interventional laboratory:Time for a safer environment. Catheter Cardiovasc Interv. 2009;73:432-438.
40. Roguin A, Goldstein J, Bar O, Goldstein JA. Brain and neck tumors among physicians performing interventional procedures. Am J Cardiol. 2013;111:1368-1372.
* Corresponding author: Àrea Malaties del Cor, Planta 19, Hospital Universitari de Bellvitge, Feixa Llarga s/n, 08907 L’Hospitalet de Llobregat, Barcelona, Spain.
E-mail address: acequier@bellvitgehospital.cat (Á. Cequier).