ABSTRACT
Introduction and objectives: The STENTYS Xposition S stent (STENTYS S.A, Paris, France) is the only self-apposing sirolimus- eluting stent available in the market. The stent features make it useful to treat challenging lesions with proximal-distal different vessel diameter, ectasia, high thrombus burden, bifurcation lesions including the left main coronary artery or vein grafts. We describe our own experience with the use of this stent and evaluate its efficacy and safety profile.
Methods: We included all consecutive patients treated with the STENTYS Xposition S from January 2018 to October 2019. All coronary lesions were quantified using QCA (quantitative coronary angiography).
Results: A total of 62 lesions in 50 patients were treated with the STENTYS Xposition S. The median age of the patients was 66 years (49-92). The most common clinical presentation was ST-segment elevation acute coronary syndrome in 23 patients (46%). Ectasia and significant vessel diameter variance were the most common scenario in 72.6% of cases and bifurcation in the remaining 27.4% (2 of them in the left main coronary artery). Pre-dilatation was performed in 32 lesions (51.6%) and post-dilatation in 37 (59.7%). Angiographic success was achieved in all patients except for 1. At the median 373-day follow-up (256-439), 1 patient had an acute myocardial infarction 3 months after the percutaneous intervention and 1 patient died due to cardiac failure during admission. There were no cases of definitive stent thrombosis or target lesion revascularization.
Conclusions: The STENTYS Xposition S self-apposing stent showed good angiographic and clinical outcomes in our real-world experience.
Keywords: Self-apposing stent. Coronary lesion. Major adverse cardiovascular events.
RESUMEN
Introducción y objetivos: El stent STENTYS Xposition S (STENTYS S.A., París, Francia) es el único stent autoexpandible liberador de sirolimus disponible en el mercado. Sus características hacen que resulte útil en lesiones que presentan gran diferencia del diámetro del vaso proximal-distal, ectasia, alta carga de trombo o que se encuentren en bifurcaciones e injertos venosos. Describimos nuestra experiencia con el uso de este tipo de stent, evaluando su seguridad y eficacia.
Métodos: Se incluyeron todos los pacientes consecutivos tratados con STENTYS desde enero de 2018 hasta octubre de 2019. Todas las lesiones coronarias fueron cuantificadas por angiografía coronaria cuantitativa.
Resultados: Se trataron con STENTYS Xposition S 62 lesiones en 50 pacientes. La mediana de edad de los pacientes fue de 66 años (49-92). La clínica de presentación más frecuente fue el síndrome coronario agudo con elevación del segmento ST en 23 pacientes (46%). La ectasia coronaria y la gran diferencia en los diámetros proximal y distal a la lesión fue la indicación más frecuente para el uso de este tipo de stent, en el 72,6% de los casos, seguida del intervencionismo sobre bifurcación en el 27,4% de los pacientes (2 de ellos en el tronco coronario izquierdo). Se realizó predilatación en 32 lesiones (51,6%) y posdilatación en 37 (59,7%). Se logró el éxito angiográfico en todos los pacientes excepto en 1. Tras una mediana de seguimiento de 373 días (256-439), 1 paciente presentó infarto agudo de miocardio a los 3 meses y 1 paciente falleció durante el ingreso por insuficiencia cardiaca. No hubo ningún caso de trombosis definitiva del stent ni de revascularización de la lesión tratada.
Conclusiones: En nuestra experiencia de la vida real, el stent STENTYS Xposition S demostró un buen resultado angiográfico y clínico.
Palabras clave: Stent autoexpandible. Lesión coronaria. Eventos cardiovasculares adversos mayores.
Abbreviations LMCA: left main coronary artery. MACE: major adverse cardiovascular events.
INTRODUCTION
The STENTYS Xposition S (STENTYS S.A., Paris, France) is a sirolimus-eluting self-expanding nitinol stent designed to adapt its size to the vessel diameter and facilitate its complete apposition when exerting chronic strength towards the outside. It has long been confirmed that one of the most important factors of stent thrombosis is the incorrect apposition of the stent.1 The characteristics of this stent make it especially useful to revascularize acute coronary syndromes (ACS), especially ST-segment elevation acute coronary syndromes with lesions with high thrombotic load. Also, a potential benefit in ectatic coronary vessels and lesions with great proximal and the distal diameter mismatch has been confirmed, bifurcations (left main coronary artery [LMCA] included), and venous grafts.
The objective of this study was to assess the benefit of this stent in the routine clinical practice by analyzing the type of lesions this stent is used with and the immediate angiographic results and at the clinical follow-up.
METHODS
A cohort of consecutive patients treated with the STENTYS Xposition S stent was analyzed from January 2018 through October 2019 in a tertiary hospital where over 1000 percutaneous coronary interventions are performed each year. All coronary lesions were quantified using a quantitative coronary angiography. Lesions in vessels with changes in size (ectasia or proximal-distal diameter mismatch of the lesion), in a bifurcation, in the presence of a high thrombotic load or in a venous graft were analyzed. The interventional strategy to be followed, imaging modalities included, was left to the operator’s criterion. The clinical and follow-up data were obtained from the electronical clinical records of the healthcare system of our autonomous community. All events were defined in a standard way according to the Academic Research Consortium-2 (ARC-2) consensus document.2
Patients' informed consent was obtained to the interventional procedure and, subsequently, verbal informed consent was given during the follow-up.
The data analysis was conducted using the IBM SPSS 20.0 statistical software package. Continuous variables were expressed as mean ± standard deviation or median with interquartile range depending on whether they followed a normal distribution or not, respectively. Qualitative variables were expressed as relative percentage. The cumulative incidence of events at the follow-up was estimated.
RESULTS
From January 2018 through September 2019, 1692 percutaneous coronary interventions with stent implantation were performed. The STENTYS Xposition S stent was used in 50 patients (62 lesions). The patients’ median age was 66 years [49-92]. Eighty-eight per cent of the patients were males. Table 1 shows the clinical characteristic of patients and coronary lesions. The most common clinical presentation was ST-segment elevation acute coronary syndrome in 23 patients (46%) followed by non-ST-segment elevation acute coronary syndrome in 22 patients (44%), and stable angina in 5 patients (10%). According to the classification established by the American College of Cardiology/American Heart Association the most common type of lesion was B1 lesion (38.7%). The right coronary artery was the most frequently treated vessel in 33 patients (53.2%).
Table 1 Clinical characteristics of patients and angiographic characteristics of the lesions
| Patients (N) | 50 |
| Age (years) | 66.6 (49-92) |
| Males | 44 (88%) |
| Arterial hypertension | 33 (66%) |
| Body mass index (kg/m2) | 27.9 ± 4.9 |
| Dyslipidemia | 32 (64%) |
| Diabetes mellitus | 12 (24%) |
| Smoking | 27 (54%) |
| Family history of ischemic heart disease | 3 (6%) |
| Peripheral vasculopathy | 3 (6%) |
| Atrial fibrillation | 6 (12%) |
| Chronic pulmonary disease | 6 (12%) |
| Kidney disease | 6 (12%) |
| Stable angina pectoris | 5 (10%) |
| NSTEACS | 22 (44%) |
| STEACS | 23 (46%) |
| Lesions (N) | 62 |
| Lesion length (mm) | 14.56 ± 3.64 |
| Reference diameter (mm) | 4.1 ± 0.8 |
| Percent stenosis. QCA (%) | 70.08 ± 17 |
| Location of the lesion | |
| Left main coronary artery | 3 (4.8) |
| Left anterior descending coronary artery | 11 (17.7) |
| Left circumflex artery | 15 (24.2) |
| Right coronary artery | 33 (53.2) |
| Classification of the lesion | |
| A | 0 |
| B1 | 24 (38.8) |
| B2 | 19 (30.6) |
| C | 19 (30.6) |
| Indication for STENTYS | |
| Ectasia. Proximal-distal diameter mismatch | 45 (72.6) |
| Bifurcation | 17 (27.4) |
| Provisional stenting technique | 15 (88.2) |
| Double stent technique | 2 (11.8) |
|
NSTEACS, non-ST-segment elevation acute coronary syndrome; QCA, quantitative coronary angiography; STEACS, ST-segment elevation acute coronary syndrome. Kidney damage: glomerular filtration rate < 60 mL/min/1.73 m2. Data are expressed as N (%) o mean ± standard deviation. |
|
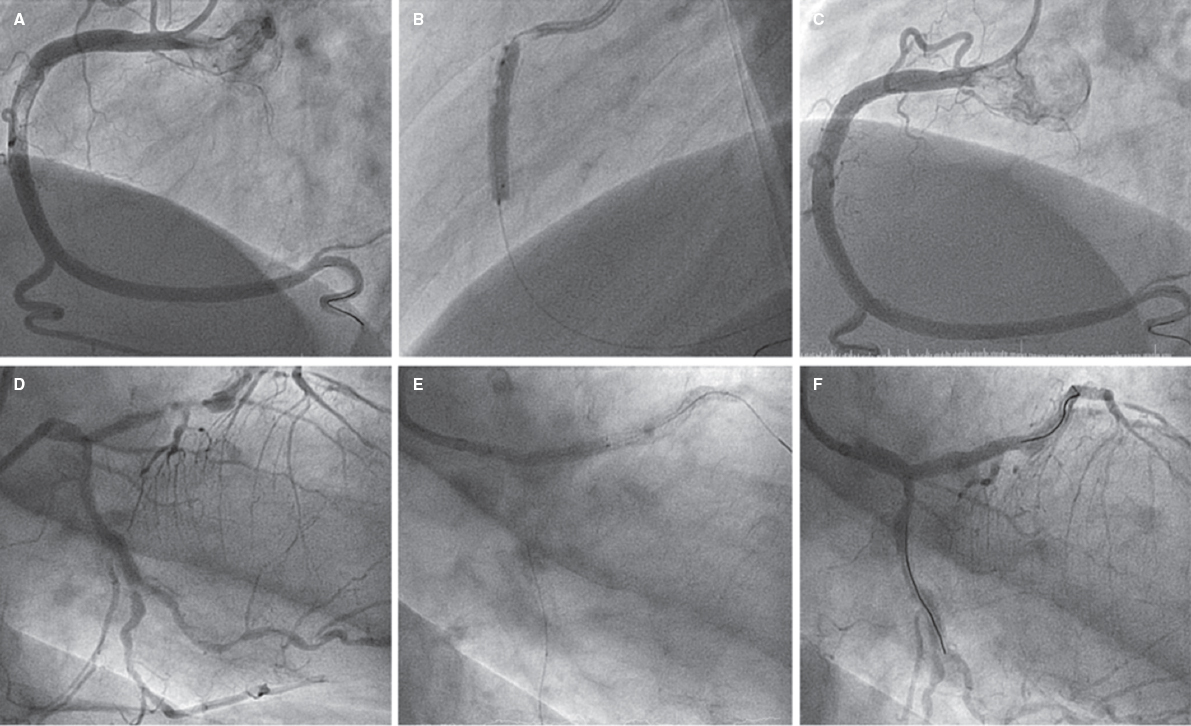
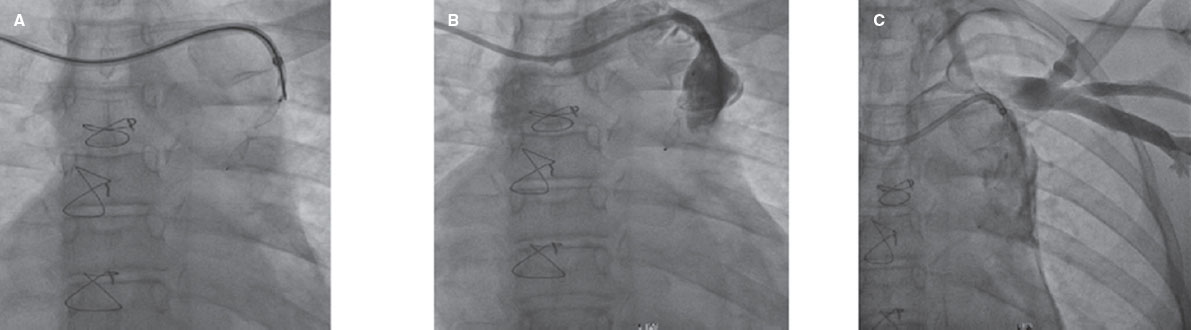
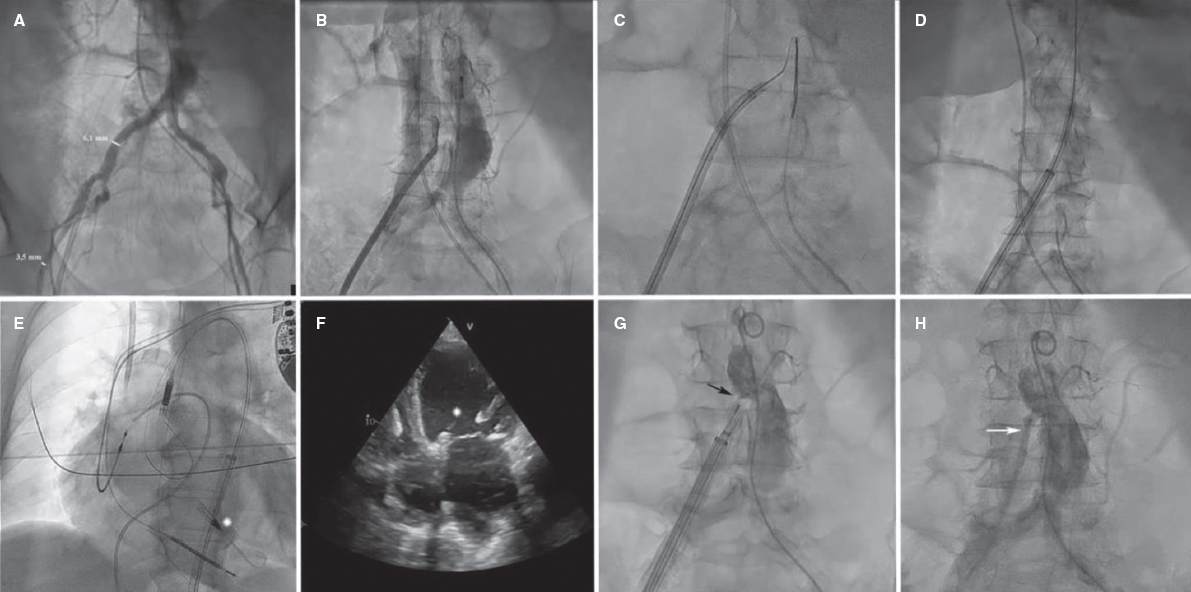
Ectasia and great proximal-distal diameter mistmatch at the lesion were the main indication for the use of this stent, in 72.6% of the lesions, with a mean vessel reference diameter of 4.1 mm ± 0.8 mm. A certain size was required to use this type of stent. The percutaneous coronary interventional on a bifurcation was the second most common indication, in 27.4% of the patients (2 of them on the LMCA). The most common type of bifurcation according to the Medina classification was 1-1-0, in 9 cases (52.9%). The secondary branch was damaged in 17% of the patients. The provisional stenting technique was the most widely used in 15 cases (88.2% of bifurcations) re-crossing to the secondary branch in 9 of them (60%). The dilatation of the secondary branch only occurred in 7 patients and only in the other 2 stents were implanted: one in a 0-1-1 bifurcation according to the Medina classification (minicrash technique) and the other in a 1-1-1 bifurcation according to this classification (TAP technique [T-and protrusion technique]). In both cases the STENTYS Xposition S stent was implanted in the main vessel and a non-self-apposing stent in the secondary branch (figure 1).
Figure 1. A: lesion with significant thrombotic load in the mid right coronary artery, which remains after thrombus aspiration. B: 3.5-4.5 mm × 27 mm Xposition S direct stent implantation. C: final angiographic result. D: significant stenosis in distal left main coronary artery. E: 3-3.5 mm × 27 mm Xposition S stent implantation from the proximal left main coronary artery to the left anterior descending coronary artery. F: angiographic result after postdilatation.
A high thrombotic load (Thrombolysis in Myocardial Infarction flow grade 4-5) was seen in 8 lesions. All of them in ectatic coronary vessels or with proximal-distal caliber mismatch. No case of venous graft treated with STENTYS was reported.
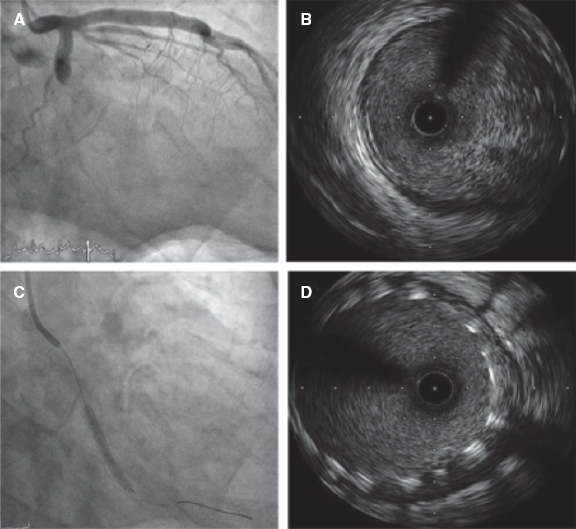
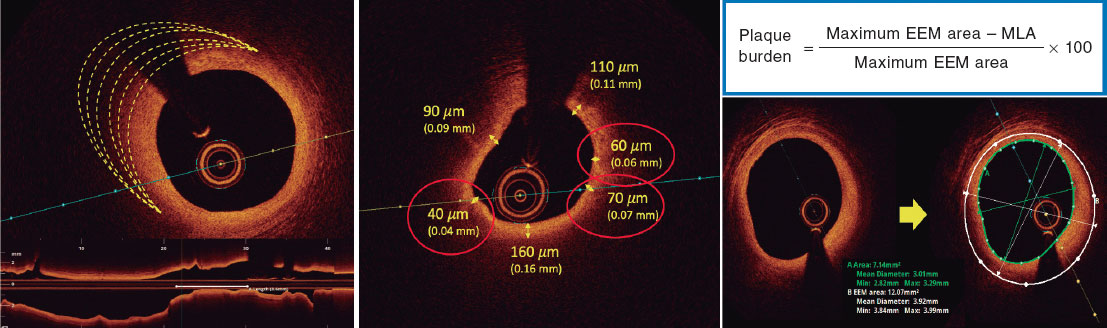
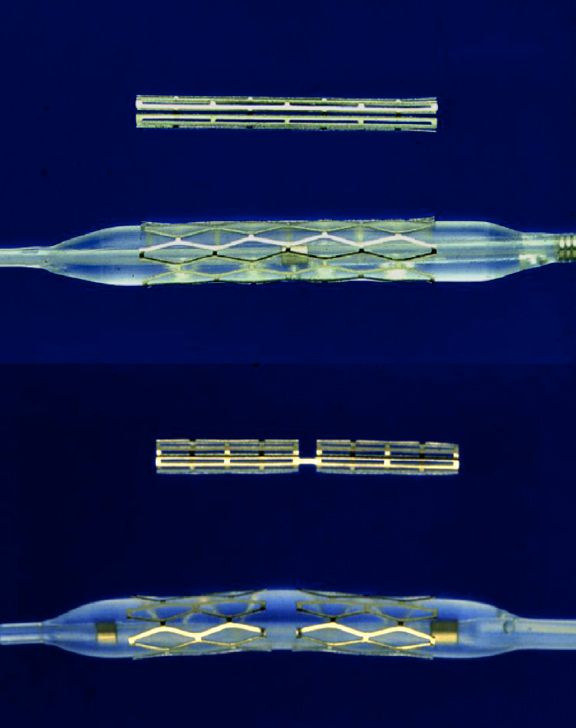
Predilatation occurred in 32 lesions (51.6%) and postdilatation in 37 (59.7%). The criterion used for postdilatation was angiography guided visual underexpansion. Intravascular ultrasound was performed in 15 patients (30%) before the implant. It was also used in 2 patients to optimize the percutaneous coronary intervention given the persistent stent underexpansion seen on the angiography. In both cases the minimum lumen area was > 5.5 mm2 with stent expansion > 80% and lack of incomplete apposition (defined as a strut separation of > 0.4 mm axial and 1 mm longitudinal) (figure 2). The optical coherence tomography was performed in a patient with ST-segment elevation acute coronary syndrome before and after the implant. It revealed a high thrombotic load with lack of immediate stent malapposition.
Figure 2. A: acute thrombotic occlusion in left circumflex artery with Thrombolysis in Myocardial Infarction flow grade 0. B: the intravascular ultrasound shows a great deal of thrombus in the lesions despite thrombus aspiration. C: implantation of 2 3.5-4.5 mm × 27 mm Xposition S overlapping stents. D: the intravascular ultrasound performed after stent implantation confirms the good angiographic results and lack of stent malapposition.
Angiographic success was achieved (with the stent properly implanted, a residual lesion ≤ 10%, and Thrombolysis in Myocardial Infarction flow grade 3) in all patients but 1, in whom stent implantation failed in a severely calcified LMCA lesion. In this case, predilatation was first attempted using a conventional balloon and then a cutting balloon on the LMCA severe distal lesion. A 3.3-4.5 mm × 22 mm STENTYS Xposition S stent was implanted with stent loss during retrieval, which remained braced to the guide catheter. Afterwards, a balloon-expandable drug-eluting stent was successfully implanted. The un-crimped stent was retrieved by crossing a guidewire from the femoral access through the stent distal struts. It was finally captured with a snare.
The median score obtained in the PRECISE-DAPT risk calculator (Predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy) was 16.5 (7-25), and the median score obtained in the DAPT index (Dual antiplatelet therapy) was 1.15 (−2-4). Ticagrelor was the most commonly used P2Y12 inhibitor (58.1%). A 12-month course of dual antiplatelet therapy was prescribed in 48 patients (96%).
After a median follow-up of 373 days (256-439), 1 patient had an acute myocardial infarction 3 months after the intervention. However, the coronary angiography did not reveal coronary artery disease progression but confirmed the good results of the previous intervention. An 84-year-old woman died at admission due to heart failure. Three patients died of non-cardiac causes: 1 due to septic shock at admission, the other patient died 6 months after the percutaneous coronary intervention due to high-grade lymphoma, and the third one 4 months after the percutaneous coronary intervention due to lung cancer. No cases of definitive stent thrombosis or revascularization of the treated lesion were reported. No bleeding was seen either at the follow-up.
DISCUSSION
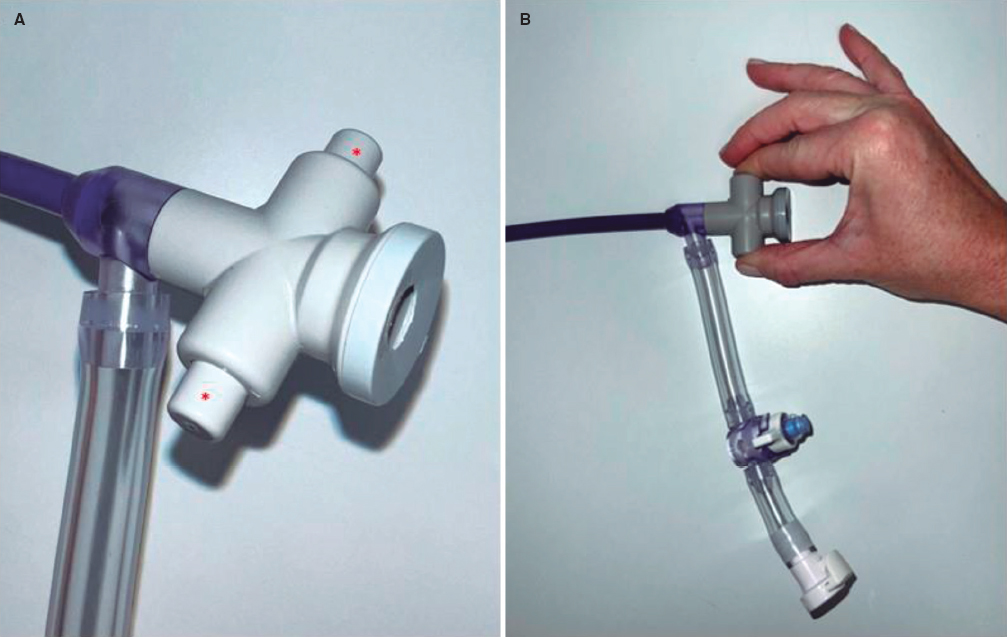
This type of stent is not widely used in our setting and we believe 2 are the reasons why. The first one is the need for a learning curve to know how to handle this implant. In former iterations of the device, the delivery system had some technical limitations like the jumping phenomenon that could occur right when the sheath was being released due to the elastic properties of nitinol. Unlike its predecessor (STENTYS sirolimus DES), the stent of the new STENTYS Xposition S system, is mounted over a semicompliant balloon and covered by a 0.0032 in-thick sheath. The reason for balloon inflation is not to dilate the stent, but to rupture the external sheath from the distal to the proximal border to allow a proper vessel-wall stent apposition. This has reduced the complexity of the release mechanism.3 However, we should remember that after the implant, the retrieval of both the balloon and the device sheath should be conducted with care by separating the guide catheter from the ostium to avoid deep intubation. The other reason that may explain why this stent is still not widely used can the augmented profile of the device and its rigidity, which both reduce its navigational and crossing capabilities compared to balloon-expandable stents.
Due to the characteristics of the stent and the experienced gained using it, the clinical settings where it can be useful are: ectatic vessel, since the stent reaches 6.5 mm of diameter with the device L size; proximal and distal diameter mismatch due to its adaptative capabilities to the vessel caliber; lesions with high thrombotic load, since this stent self-expanding capabilities facilitate its expansion until it reaches the vessel wall if thrombus reabsorption occurs, which avoids late stent malapposition; and bifurcations with ostial damage and 30º to 70° angles. The stent z-shaped mesh and the presence of small interconnectors facilitate re-crossing the lateral branch and disconnecting the struts without having to use the final kissing balloon technique. Thanks to its self-expanding capabilities, the unconnected struts cover the lateral branch ostium making the double stent technique unnecessary on many occasions.
In the studies published on former iterations of the device, the self-expanding stent proved superior to the balloon-expandable stent regarding better apposition. The randomized APOSSITION II clinical trial,4 conducted among patients with acute myocardial infarction, showed a lower rate of stent malapposition (defined as > 5% of struts per patient as seen on the optical coherence tomography) 3 days after the primary percutaneous coronary intervention. The APOSSITION IV clinical trial,5 also conducted among patients with acute myocardial infarction, showed a significantly lower percentage of stent malapposition at the 4-month follow-up in patients treated with self-expanding stents compared to patients treated with balloon-expandable stents (0.07% vs 1.16%; P = .002). However, no inter-group differences were found at the 9-month follow-up (0.43% vs 0.28%; P = .55) or in the rate of major adverse cardiovascular events (MACE). The clinical repercussions of this improvement in the early apposition of the stent has not been studied thoroughly. The APOSSITTION III trial6 showed that the use of STENTYS BMS in the percutaneous coronary intervention setting was associated with acceptable cardiovascular results at the 2-year follow-up, an overall rate of MACE of 11.2%, and a rate of stent thrombosis of 3.3%. We should mention that this study revealed a significant reduction of adverse events after the systematic implementation of a standard protocol (predilatation, implantation, postdilatation). The data available support the hypothesis of the need for mild postdilatation to avoid early complications probably because the stent does not have enough radial strength to achieve a proper expansion in rigid often calcified lesions, especially when predilatation is not fully effective. Therefore, postdilatation would avoid the incomplete expansion of the stent, which may increase the risk of stent thrombosis.7
Our study with the STENTYS Xposition S stent reached angiographic success in 98.4% of the cases, although we should remember that, from the anatomical point of view, they were not complex lesions (only 30% were type C lesion). Stent implantation failed in 1 severely calcified LMCA lesion; it is precisely in this type of lesions where its use is ill-advised, especially if predilatation is not effective.8
Regarding its use in bifurcations the studies published to this day have also discussed a former iteration of this device with good results. In the observational, multicenter, and prospective OPEN II trial,9 the rate of MACE at the 12-month follow-up was 13% (10.1% at 6 months). This rate of events was basically due to the need for revascularization of the treated lesion, while the rate of stent thrombosis at the 12-month follow-up was 1%. We should also mention that the kissing balloon technique was only used in 21.7% of the patients. Also, there were no significant differences in the rate of MACE between patients in whom the kissing balloon technique was used and those in whom it was not used.9
To this day, the only study published on the new STENTYS Xposition S model is the TRUNC, a prospective and multicenter study that assessed the efficacy and safety profile of this type of stent in the LMCA. Angiographic success was achieved in 96.6% of the patients and the overall rate of MACE was 8.3% at the 12-month follow-up, basically due to revascularization of the lesion treated in 5.4%.10 Here we should mention the preliminary results reported by the SIZING (Worldwide every-day practice registry assessing the Xposition S self-apposing stent in challenging lesions with vessel diameter variance) and WIN (World-wide registry to assess the STENTYS Xposition S for revascularization of coronary arteries in routine clinical practice) registries. Both registries confirm the safety and efficacy profile of the current iteration of the stent in the routine clinical practice.
Limitations
Our study has several limitations. Because of its retrospective, single-center nature and the limited number of cases involved, we cannot draw definitive conclusions on the device safety and efficacy profile. No intracoronary imaging modality was performed systematically to guide the implant, which may have been useful, especially the optical coherence tomography. However, we believe that this study is relevant due to the scarce evidence available on the last iteration of this stent.
CONCLUSIONS
In our series of lesions located in ectatic vessels or with proximal-distal diameter mismatch and in bifurcations, the STENTYS Xposition S stent is a good therapeutic alternative that achieves good immediate angiographic results and good mid-term clinical results.
FUNDING
No funding to declare.
AUTHORS' CONTRIBUTIONS
Data collection: A. Pérez Guerrero, I. Caballero Jambrina. Data analysis: A. Pérez Guerrero, G. Fuertes Ferré, I. Caballero Jambrina, G. Galache Osuna, M.C. Gracia Ferrer. Analysis and interpretation of data: A. Pérez Guerrero, G. Fuertes Ferré, J. Sánchez-Rubio, G. Galache Osuna, M.C. Gracia Ferrer. Critical review of manuscript: J.A. Diarte de Miguel, M.R. Ortas Nadal.
CONFLICTS OF INTEREST
None declared.
WHAT IS KNOWN ABOUT THE TOPIC?
- Balloon expandable stents can have limitation in certain scenarios like in the revascularization of lesions with significant proximal-distal diameter mismatch, high thrombotic loads, and situations of bifurcations or in venous grafts. In these situations, the STENTYS Xposition S self-expanding stent can be especially useful.
WHAT DOES THIS STUDY ADD?
- This type of stent is not widely used in our specialty. We described the experience of our own center with the STENTYS Xposition S stent. Despite the greater difficulty when trying to advance it and the complexity involved in its delivery, the rate of successful implantation was high. We should not forget that this type of stent is recommended in non-complex or non-calcified anatomical lesions. In general, predilatation is recommended to prepare the lesion and postdilatation to secure the proper expansion of the stent since the stent lacks the necessary radial strength. In our series of patients, the STENTYS Xposition S stent was safe and with a low rate of adverse cardiovascular adverse events at the 1-year follow-up.
REFERENCES
1. Cook S, Eshtehardi P, Kalesan B, et al. Impact of incomplete stent apposition on long-term clinical outcome after drug-eluting stent implantation. Eur Heart J. 2012;33:1334-1343.
2. Garcia-Garcia HM, McFadden EP, Farb A, et al. Standardized End Point Definitions for Coronary Intervention Trials:The Academic Research Consortium-2 Consensus Document. Circulation. 2018;137:2635-2650.
3. Lu H, IJsselmuiden AJ, Grundeken MJ, et al. First-in-man evaluation of the novel balloon delivery system STENTYS Xposition S for the self-apposing coronary artery stent:impact on longitudinal geographic miss during stenting. EuroIntervention. 2016;11:1341-1345.
4. Van Geuns R-J, Tamburino C, Fajadet J, et al. Self-expanding versus balloon-expandable stents in acute myocardial infarction:Results from the APPOSITION II study. Self-expanding stents in ST-segment elevation myocardial infarction. J Am Coll Cardiol Intv. 2012;5:1209-1219.
5. Van Geuns RJ, Yetgin T, La Manna A, et al. STENTYS self-apposing sirolimus-eluting stent in ST-segment elevation myocardial infarction:results from the randomised APPOSITION IV trial. EuroIntervention. 2016;11:1267-1274.
6. Koch KT, Grundeken MJ, Vos NS, et al. One-year clinical outcomes of the STENTYS Self-Apposing(R) coronary stent in patients presenting with ST-segment elevation myocardial infarction:results from the APPOSITION III registry. EuroIntervention. 2015;11:264-271.
7. Sato T, Kameyama T, Noto T, Nozawa T, Inoue H. Impact of preinterventional plaque composition and eccentricity on late-acquired incomplete stent apposition after sirolimus- eluting stent implantation:an intravascular ultrasound radiofrequency analysis. Coron Artery Dis. 2012;23:432-437.
8. Verheye S, Ramcharitar S, Grube E, et al. Six-month clinical and angiographic results of the STENTYS R self-apposing stent in bifurcation lesions. EuroIntervention. 2011;7:580-587.
9. Naber CK, Pyxaras SA, Nef H, et al. Final results of a self-apposing paclitaxel-eluting stent for the percutaneous treatment of de novo lesions in native bifurcated coronary arteries study. EuroIntervention. 2016;12:356-358.
10. Tamburino C, Briguori C, Jessurun GA, et al. TCT-329 prospective evaluation of drug eluting selfapposing stent for the treatment of unprotected left main coronary artery disease:1-year results of the TRUNC study. J Am Coll Cardiol. 2018;72:134-135.
Corresponding author: Servicio de Cardiología, Hospital Universitario Miguel Servet, Paseo Isabel la Católica 1-3, 50009 Zaragoza, Spain.
E-mail address: ainhoaperezguerrero@gmail.com (A. Pérez Guerrero).