ABSTRACT
Introductionand objectives: We assessed whether the routine use of subcutaneous nitroglycerin prior to a cannulation attempt improves transradial access significantly (the NiSAR study [subcutaneous nitroglycerin in radial access]).
Methods: Patients undergoing a coronary angiography were enrolled in a prospective, double-blind, multicenter, randomized trial in 2 groups (nitroglycerin group vs control group). The primary endpoints were the overall number of puncture attempts, access and procedural time, switch to transfemoral access, and local perceived discomfort score. The secondary endpoints were the pre- and post-anesthetic pulse score. A subgroup of patients underwent ultrasound scans performed through the radial artery.
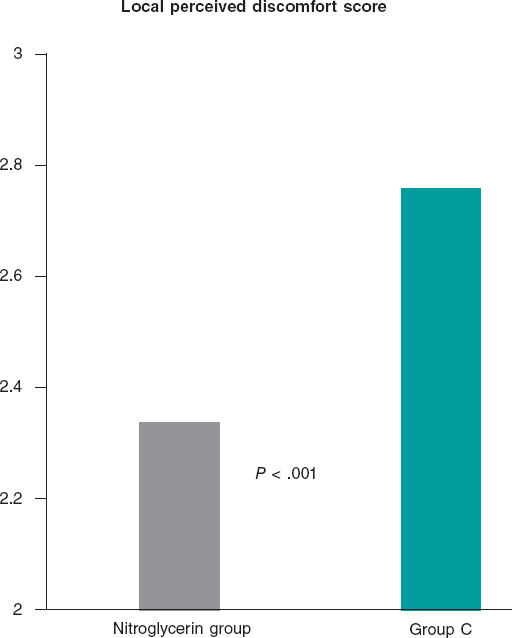
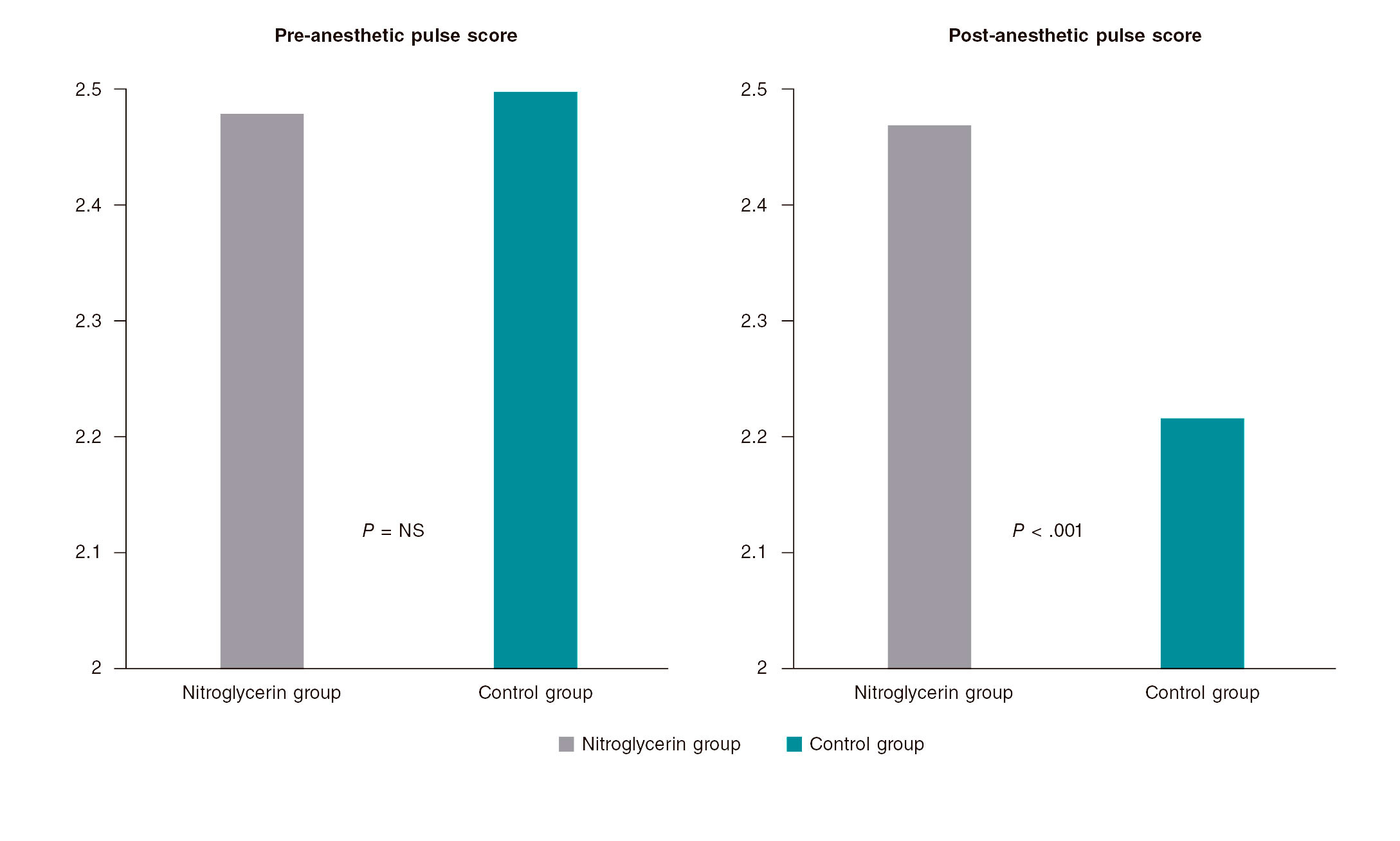
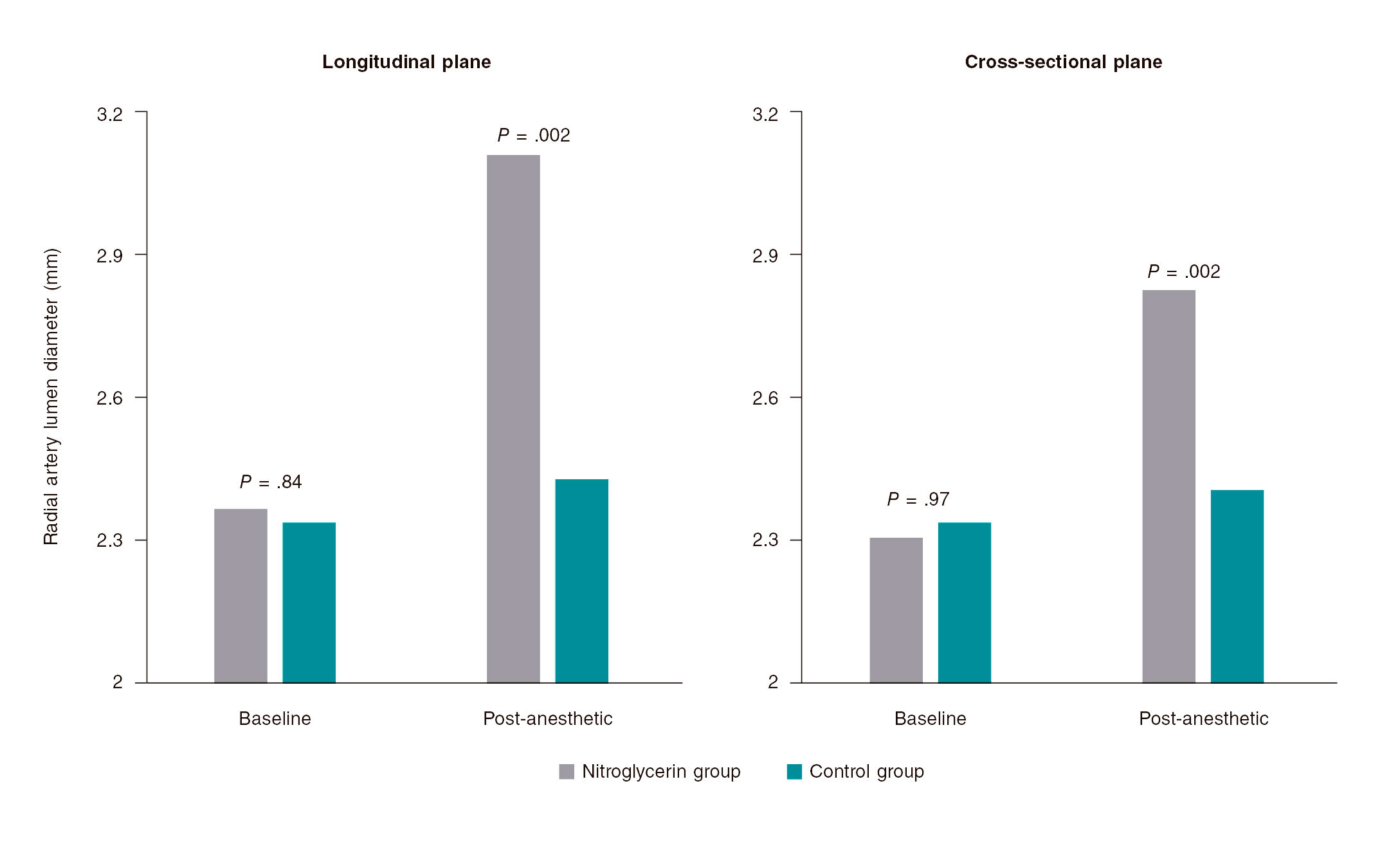
Results: 736 patients were enrolled in the trial: 379 in the nitroglycerin group and 357 in control group. The average number of puncture attempts was similar (1.70 vs 1.76; P = .42). Access and procedural time did not change significantly (61.1 s and 33.3 s vs 63 s and 33.4 s; P = .66 and P = .64, respectively). No significant differences were found either between the 2 groups in the number of switches to transfemoral access (7.1% vs 8.4%; P = .52). However, the average local perceived discomfort score and post-anesthetic pulse score were significantly better in the nitroglycerin group (2.34 vs 2.76; P< .001 and 2.47 vs 2.22; P< .001). The ultrasound scan performed through the radial artery showed post-anesthetic radial artery lumen diameters that were significantly higher in the nitroglycerin group in both the longitudinal (3.11 mm vs 2.43 mm; P = .002) and cross-sectional planes (2.83 mm vs 2.41 mm; P = .002). A trend towards fewer local hematomas in the nitroglycerin group was seen (6.1% vs 9.8%; P = .059). Headaches were more common in the nitroglycerin group (3.2% vs 0.6%; P = .021).
Conclusions: The routine use of subcutaneous nitroglycerin prior to radial puncture was not associated with fewer punctures or shorter access times. However, the lower local perceived discomfort and enlargement of the radial artery size would justify its daily use in the routine clinical practice to enhance the transradial experience for both patients and operators.
Keywords: Transradial access. Subcutaneous nitroglycerin. Radial spasm.
RESUMEN
Introducción y objetivos: Se evaluó si la utilización sistemática de nitroglicerina subcutánea previa a cualquier intento de canulación podía mejorar de forma significativa el acceso transradial (nitroglicerina subcutánea acceso radial [NiSAR]).
Métodos: Se incluyeron todos los pacientes sometidos a angiografía coronaria en un estudio prospectivo, multicéntrico, doble ciego y aleatorizado, y se dividió la población en 2 grupos: grupo de nitroglicerina y grupo control. Los objetivos primarios del estudio fueron el número total de punciones radiales, el tiempo total de acceso y de procedimiento, la necesidad de cambio a acceso femoral y la puntuación de disconfort local. El objetivo secundario fue la evaluación del pulso antes y tras la anestesia. Además, un subgrupo de pacientes fue evaluado con ecografía de la arteria radial.
Resultados: Se incluyeron736 pacientes: 379 en el grupo de nitroglicerina y 357 en el grupo C. El número promedio de intentos de punción radial fue similar en ambos (1,70 frente a 1,76; p = 0,42). No hubo diferencias significativas en los 2 grupos con respecto al tiempo total del acceso y del procedimiento (61,1 y 33,3 s frente a 63 y 33,4 s; p = 0,66 y p = 0,64, respectivamente). Tampoco se encontraron diferencias significativas entre los 2 grupos en la tasa de conversión a acceso femoral (7,1 en el grupo de nitroglicerina frente a 8,4% en el grupo C; p = 0,52). Sin embargo, el índice de malestar local y el de pulso tras la anestesia fueron significativamente mejores en el grupo de nitroglicerina (2,34 frente a 2,76, p < 0,001; 2,47 frente a 2,22, p < 0,001). La ecografía mostró un diámetro radial significativamente mayor en el grupo de nitroglicerina tanto en la vista longitudinal (3,11 frente a 2,43 mm; p = 0,002) como en la transversal (2,83 frente a 2,41 mm; p = 0,002). Hubo una menor incidencia de hematoma en el antebrazo en el grupo de nitroglicerina (6,1 frente a 9,8%; p = 0,059). La cefalea fue más frecuente en los pacientes del grupo de nitroglicerina (3,2 frente a 0,6%; p = 0,021).
Conclusiones: El uso sistemático de nitroglicerina subcutánea previo a la punción radial no estuvo asociado a una reducción en el número de punciones ni en el tiempo de acceso, pero el menor malestar local y el aumento del calibre de la arteria radial podrían justificar su uso en la práctica clínica para mejorar la experiencia del acceso transradial tanto en el paciente como en el operador.
Palabras clave: Espasmo radial. Nitroglicerina subcutánea. Acceso radial.
INTRODUCTION
Transradial access to perform coronary and peripheral procedures is becoming more successful compared to transfemoral access thanks to several advantages including more comfort as reported by the patients, early ambulation and discharge, less bleeding, and overall better outcomes.1-5However, the radial artery is more susceptible to spasm, which can stop the advance of the catheter, extend the duration of the procedure, and increase its difficulty.6Also, radial artery spasm has been identified as an independent predictor of radial access failure.7
When radial artery spasm occurs after an introducer sheath has been inserted, the intra-arterial administration of vasodilator drugs has proved to improve the conduit effectively.8Still, the subcutaneous administration of nitroglycerin relieves the spasm causing the reduction significantly and the eventual loss of pulse volume after several ineffective attempts to cannulate the radial artery.9Also, it enhances radial pulse palpation, and eventually makes the puncture of radial artery easier.10,11
Because the first puncture failure is a powerful predictor of radial artery spasm,12we conducted a double-blind, randomized, controlled trial in 4 Argentinian centers to see whether the routine subcutaneous administration of nitroglycerin prior to a cannulation attempt improved transradial access significantly (the NISAR study [subcutaneous nitroglycerin in radial access]).
Specifically, the primary endpoints of the study were to assess the number of radial artery puncture attempts, the time required to place the sheath introducer, the number of times that switching to transfemoral access was required, and the patients’ tolerance to the procedure. The secondary endpoints included the assessment of the radial artery pulse and diameter and local and systemic complications.
METHODS
Patients and procedures
Patients undergoing a coronary angiography with evidence of myocardial ischemia were enrolled in a prospective, multicenter, and randomized clinical trial conducted in 4 Argentinian centers into 2 different groups based on the periradial subcutaneous administration of nitroglycerin. In the nitroglycerin group, 2% xylocaine (1 mL) was used followed by 200 mcg of nitroglycerin (2 mL). In control group, 2% xylocaine (1 mL) was followed by the infusion of a normal saline solution (2 mL) used as placebo. Trained nurses from each center prepared the syringes following a 1:1 randomization scheme and making sure that their content was unknown to both the operators and the patients.
The coronary angiographies and revascularization procedures were performed using 5-Fr or 6-Fr diagnostic and guiding catheters as selected by the operators. In all cases a properly sized sheath introducer was inserted using the Seldinger or modified Seldinger technique. Five thousand units of heparin were consistently administered through a bolus injection with further additions to keep the activated clotting time between 250 and 300 seconds if a percutaneous coronary intervention was performed.
All procedures were performed after patients gave their informed consent by 8 skilled and experienced operators who had performed over 1500 transradial procedures. All operators used the right radial artery as the access of choice; the left radial artery was spared for cases with right radial artery occlusion and patients with left internal mammary artery graft. The Ethics Committe reviewed and approved this study. Patients' informed consent to publish was obtained.
Outcome measures
The primary outcome measures were the overall number of puncture attempts, access, and procedural time, switch to transfemoral access, and local perceived discomfort score.
Access time was defined as the time elapsed between the administration of local anesthesia and the insertion of the radial sheath introducer. When the initial radial access could not be completed, the contralateral radial access was never tried and access site changed to the femoral access. The local perceived discomfort score was assessed by the patient after undergoing the procedure and graded according to a radial-related pain score between 0 = no pain and 10 = unbearable pain.
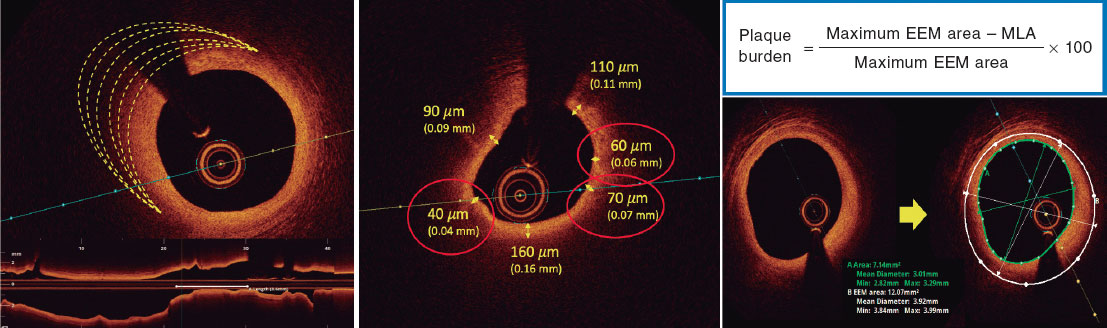
The secondary outcome measures were the pre- and post-anesthetic pulse score assessed by the operator by palpating the radial pulse before and 1 minute after the administration of local anesthesia and graded as: 1 = weak pulse; 2 = easily palpable pulse; 3 = strong pulse. Also, local and systemic complications including forearm hematomas, radial artery spasm, headaches, and symptomatic hypotension were recorded. Also, a subgroup of patients underwent a radial artery ultrasound scan both at the baseline and after the administration of anesthesia. Patients were examined in the supine position using a commercially available ultrasound system. The radial artery lumen diameter was measured on M-mode imaging in both the longitudinal and cross-sectional planes and 1 cm proximal to the radius styloid process. Three measures were taken in each plane and their values averaged.
Statistics
Continuous variables were compared using the Student t test. Categorical variables were compared using Pearson chi-square test. Data were expressed as mean ± standard deviation or frequency (percentage). Two-tailed P values < .05 were considered statistically significant.
RESULTS
Characteristics of patients and procedural details
Overall, 736 patients (450 men, age 65 ± 10 years) were enrolled in the trial: 379 (51.5%) in the nitroglycerin group and 357 (48.5%) in control group. Table 1 shows their general characteristics. Active smoking and diabetes mellitus were reported by 292 (39.7%) and 168 (22.8%) of the patients, respectively and 240 (46.1%) showed an unstable presentation. The radial access was the first access attempted in 597 patients (81.1%).
Table 1. General characteristics of the patients
| Overall (N = 736) | Nitroglycerin group (N = 379) | Control group (N = 357) | P | |
|---|---|---|---|---|
| Age (years) | 64.9 ± 10.1 | 64.9 ± 10.1 | 65.1 ± 10.1 | .80 |
| Male gender | 450 (61.1%) | 230 (60.7%) | 220 (61.6%) | .79 |
| Body mass index | 28.5 ± 4.2 | 28.5 ± 4.2 | 28.4 ± 4.2 | .82 |
| Active smoking | 292 (39.7%) | 153 (40.3%) | 139 (38.9%) | .69 |
| Hypertension | 520 (70.6%) | 277 (73.1%) | 243 (68.1%) | .14 |
| High cholesterol | 365 (49.6%) | 189 (49.8%) | 176 (49.3%) | .88 |
| Diabetes mellitus | 168 (22.8%) | 97 (25.6%) | 71 (19.9%) | .07 |
| Clinical presentation | ||||
| ST-segment elevation myocardial infarction | 55 (7.5%) | 28 (7.4%) | 27 (7.6%) | .68 |
| Non-ST-elevation acute myocardial infarction | 285 (38.7%) | 139 (36.7%) | 146 (40.9%) | |
| Chronic stable angina | 90 (12.2%) | 51 (13.4%) | 39 (10.9%) | |
| Silent ischemia | 123 (16.7%) | 67 (17.7%) | 56 (15.7%) | |
| Preoperative assessment | 64 (8.7%) | 33 (8.7%) | 31 (8.7%) | |
| First transradial access attempt | 597 (81.1%) | 307 (81%) | 290 (81.2%) | .94 |
| Procedure | ||||
| Coronary angiography | 507 (68.9%) | 259 (68.3%) | 248 (69.5%) | .55 |
| Percutaneous coronary intervention | 24 (3.3%) | 15 (3.9%) | 9 (2.5%) | |
| Coronary angiography and ad hoc revascularization procedure | 205 (27.9%) | 105 (27.7%) | 100 (28%) |
Procedural details are shown on table 2. In most cases, the radial artery was punctured with a 20G IV catheter using the modified Seldinger technique and a plastic-jacked mini-guidewire advanced through the artery lumen. Small and short sheath introducers were used in less than half of the patients.
| Overall (N = 736) | Nitroglycerin group (N = 379) | Control group (N = 357) | P | |
|---|---|---|---|---|
| Allen test result | ||||
| Normal | 659 (89.5%) | 338 (89.2%) | 321 (89.9%) | .94 |
| Intermediate | 66 (9%) | 35 (9.2%) | 31 (8.7%) | |
| Abnormal | 11 (1.5%) | 6 (1.6%) | 5 (1.4%) | |
| Radial puncture and introducer placement | ||||
| 20G IV catheter | 719 (97.7%) | 371 (97.9%) | 348 (97.5%) | .71 |
| 0.021 in mini-guidewire | 701 (95.2%) | 364 (96%) | 337 (94.4%) | .29 |
| Plastic-jacketed mini-guidewire | 684 (92.9%) | 358 (94.4%) | 326 (91.3%) | .10 |
| Introducer length < 10 cm | 292 (39.7%) | 162 (42.7%) | 130 (36.4%) | .08 |
| Introducer size < 6-Fr | 318 (43.2%) | 166 (43.8%) | 152 (42.5%) | .74 |
| Radial artery angiography | 271 (36.8%) | 144 (38%) | 127 (35.6%) | .50 |
Outcomes
The average number of puncture attempts was similar in the nitroglycerin group compared to control group (1.70 vs 1.76; P = .42). Access and procedural times did not change significantly in either one of the 2 groups (61.1 s and 33.3 s vs 63 s and 33.4 s; P = .66 and P = .64, respectively). No significant inter-group differences were found either in the rate of switch to transfemoral access (7.1% in the nitroglycerin group vs 8.4% in control group, P = .52).
The main results of the patients and their local perceived discomfort score are shown on figure 1. The average local perceived discomfort score was significantly better in the nitroglycerin group (2.34 vs 2.76; P< .001) with a significantly higher rate of grade 0/1 (34.3% vs 25.2%; P = .088) and a lower rate of grade > 3 (33.5% vs 50.4%; P< .001).
Figure 1. Patients tolerance to the transradial procedure. The average local perceived discomfort score was significantly better in patients in whom nitroglycerin was administered subcutaneously compared to those in whom placebo was used (2.34 vs 2.76; P < .001).
figure 2 shows the results of pre- and post-anesthetic pulse score assessment. No significant differences were seen in the pre-anesthetic pulse score. However, the post-anesthetic pulse score was significantly higher in the nitroglycerin group (2.47 vs 2.22, P< .001). The rate of post-anesthetic pulse score < 3 was significantly lower in the nitroglycerin group compared to group C (41.7% vs 57.1%, P< .001).
Figure 2. Operator assessment of radial pulse. The left panel shows that no significant differences were found in the pre-anesthetic pulse score between patients in whom nitroglycerin was administered subcutaneously (nitroglycerin group) and those in whom placebo was used control group. The right panel shows that the post-anesthetic pulse score was significantly higher in the nitroglycerin group compared to control group (2.47 vs 2.22; P < .001).
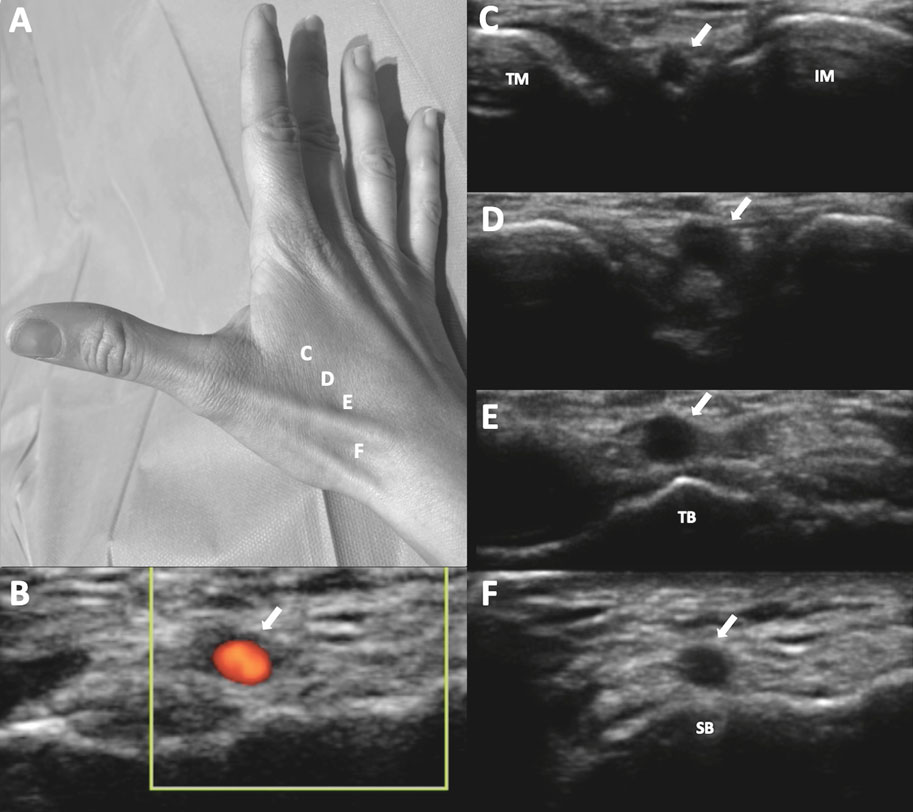
Radial artery ultrasound scans were performed in 70 patients; the results are shown on figure 3. No significant inter-group differences were seen at the baseline between the longitudinal (2.37 mm vs 2.34 mm; P = .84) and cross-sectional planes (2.31 mm vs 2.34 mm; P = .97). However, the post-anesthetic radial artery lumen diameter was significantly higher in the nitroglycerin group in both the longitudinal (3.11 mm vs 2.43 mm; P = .002) and cross-sectional planes (2.83 mm vs 2.41 mm; P = .002).
Figure 3. Radial artery ultrasound scan. No significant inter-group differences were seen at the baseline between the longitudinal (2.37 mm vs 2.34 mm; P= .84) and the cross-sectional planes (2.31 mm vs 2.34 mm; P = .97). However, the post-anesthetic radial artery lumen diameter was significantly higher in the nitroglycerin group compared to control group in both the longitudinal (3.11 mm vs 2.43 mm; P = .002) and cross-sectional planes (2.83 mm vs 2.41 mm; P = .002).
As shown on table 3, no significant differences in local complications were seen, although a trend towards a lower rate of local hematomas was seen in the nitroglycerin group (6.1% vs 9.8% P = .059). Headaches were more common among patients from nitroglycerin groups (3.2% vs 0.6%, P = .021).
Table 3. Main local and systemic complications
| Overall (N = 736) | Nitroglycerin group (N = 379) | Control group (N = 357) | P | |
|---|---|---|---|---|
| Local complications | ||||
| Forearm hematoma | 58 (7.9%) | 23 (6.1%) | 35 (9.8%) | .059 |
| Radial artery spasm | 109 (14.8%) | 49 (12.9%) | 60 (16.8%) | .14 |
| Systemic complications | ||||
| Headache | 14 (1.9%) | 12 (3.2%) | 2 (0.6%) | .021 |
| Symptomatic hypotension | 16 (2.2%) | 11 (2.9%) | 5 (1.4%) | .25 |
DISCUSSION
The main findings of our study are that the subcutaneous administration of nitroglycerin plus the administration of a local anesthetic agent prior to radial artery puncture did not show any statistically significant differences in the number of punctures attempted, access and procedural time or switch to transfemoral access. However, it significantly improved: a) the patients’ perceived comfort during the procedure; b) the radial artery pulse; and c) the radial artery size. Also, our data suggest a possible reduction in the occurrence of local hematomas. Also consistent with former studies, the subcutaneous use of nitroglycerin significantly increased the diameter of the radial artery in patients in whom an ultrasound scan was performed.10,13
The radial artery spasm is the most common complication of transradial access in both coronary angiographies and procedures. It often holds up the regular course of the procedure impacting the patients’ compliance and interfering with the cath lab proceedings.6,9Also, the occurrence of radial artery spasm before radial artery cannulation is even more frustrating to treat and may anticipate that the cannulation of the vessel will be impossible.
Multiple puncture attempts are the leading cause for radial artery spasm and may be a specific issue in the teaching environment.14,15Also, the administration of local anesthetics such as lidocaine has vasoconstrictive properties16 and the radial artery has a relatively small diameter and a relatively thicker tunica media of smooth muscle cells, which leads to a high receptor-mediated vasomotion compared to other muscular arteries.17,18Conversely, the radial artery is particularly sensitive to nitroglycerin.19
Former studies have shown that nitroglycerin delivered through IV,20topical,21or intra-arterial16,22-24routes of administration determines the radial artery dilatation; current evidence with subcutaneous nitroglycerin to facilitate radial access suggests that it can be beneficial to increase the radial pulse and reduce the number of attempts. However, the evidence on this regard is scarce and based on small studies.10,11A review that assessed this issue also failed to find significant differences between both strategies.25Our study rigorously used a double-blind, randomized protocol to assess the role of the subcutaneous administration of nitroglycerin prior to radial artery puncture. It concluded that its systematic use can improve the patient’s perceived discomfort and make puncture easier for the operator but without reducing the number of punctures attempted or access time. Our findings are especially relevant in light of the improved safety associated with transradial access.26
The subcutaneous administration of nitroglycerin is a straightforward and inexpensive technique that allows a high concentration and long persistence of the vasoactive agent at the spasm site level without entering the bloodstream significantly.9As a matter of fact, in our study no significant differences were seen in the hemodynamic effect of patients who received subcutaneous nitroglycerin or placebo.
Also, the Doppler ultrasound scans performed on the radial artery pre- and post-nitroglycerin in a subgroup of patients triggered the new NISAR study (Eco nitroglicerina subcutánea acceso radial)—currently in its design phase—with echocardiographic evaluation of all the patients included.
Limitations
All the patients of this study were taking standard anti-ischemic drugs including nitrates. We did not study the confounding effect of the vasodilation caused by these drugs. The inter-observer and inter-operator variabilities were not studied either. The Doppler ultrasound scan was used in a small subgroup of patients.
CONCLUSIONS
The routine use of subcutaneous nitroglycerin prior to radial puncture was not associated with a lower number of punctures or shorter access times. However, the lower local perceived discomfort and improved radial artery size would justify its daily use in the routine clinical practice to enhance the transradial experience of both patients and operators.
FUNDING
No funding was received for this work.
CONFLICTS OF INTEREST
None declared.
WHAT IS KNOWN ABOUT THE TOPIC?
- Radial artery spasm is still an issue; intra-arterial nitroglycerin and calcium blockers are systematically used after achieving radial access to prevent it. However, the use of subcutaneous nitroglycerin plus the administration of a local anesthetic agent prior to radial puncture is still controversial. This is so because the studies conducted so far on this issue are mostly scarce, small, and not randomized. This was confirmed in a review published back in 2018.
WHAT DOES THIS STUDY ADD?
- The strength of our study is that it is the first prospective, randomized, multicenter, double-blind trial to assess this issue.
- Regarding the results from the trial and although some hard endpoints did not reach statistically significant differences, we believe that the fact that patients tolerated the procedure better, the increase seen in the pulse score and the radial artery diameter after the administration of subcutaneous nitroglycerin added to the simplicity, security and great availability of the procedure is indicative that this technique should be widely used.
REFERENCES
1. Rao SV, Cohen MG, Kandzari DE, Bertrand OF, Gilchrist IC. The transradial approach to percutaneous coronary intervention:historical perspective, current concepts, and future directions. J Am Coll Cardiol. 2010;55:2187-2195.
2. Cooper CJ, El-Shiekh RA, Cohen DJ, et al. Effect of transradial access on quality of life and cost of cardiac catheterization:A randomized comparison. Am Heart J. 1999;138:430-436.
3. Valgimigli M, Gagnor A, Calabro P, et al. Radial versus femoral access in patients with acute coronary syndromes undergoing invasive management:a randomised multicentre trial. Lancet. 2015;385:2465-2476.
4. Wiper A, Kumar S, MacDonald J, Roberts DH. Day case transradial coronary angioplasty:a four-year single-center experience. Catheter Cardiovasc Interv. 2006;68:549-553.
5. Bertrand OF, De Larochelliere R, Rodes-Cabau J, et al. A randomized study comparing same-day home discharge and abciximab bolus only to overnight hospitalization and abciximab bolus and infusion after transradial coronary stent implantation. Circulation. 2006;114:2636-2643.
6. Ruiz-Salmeron RJ, Mora R, Velez-Gimon M, et al. Radial artery spasm in transradial cardiac catheterization. Assessment of factors related to its occurrence, and of its consequences during follow-up. Rev Esp Cardiol. 2005;58:504-511.
7. Abdelaal E, Brousseau-Provencher C, Montminy S, et al. Risk score, causes, and clinical impact of failure of transradial approach for percutaneous coronary interventions. JACC Cardiovasc Interv. 2013;6:1129-1137.
8. Kiemeneij F, Vajifdar BU, Eccleshall SC, Laarman G, Slagboom T, van der Wieken R. Evaluation of a spasmolytic cocktail to prevent radial artery spasm during coronary procedures. Catheter Cardiovasc Interv. 2003;58:281-284.
9. Pancholy SB, Coppola J, Patel T. Subcutaneous administration of nitroglycerin to facilitate radial artery cannulation. Catheter Cardiovasc Interv. 2006;68:389-391.
10. Ezhumalai B, Satheesh S, Jayaraman B. Effects of subcutaneously infiltrated nitroglycerin on diameter, palpability, ease-of-puncture and pre-cannulation spasm of radial artery during transradial coronary angiography. Indian Heart J. 2014;66:593-597
11. Ouadhour A, Sideris G, Smida W, Logeart D, Stratiev V, Henry P. Usefulness of subcutaneous nitrate for radial access. Catheter Cardiovasc Interv. 2008;72:343-346.
12. Jia DA, Zhou YJ, Shi DM, et al. Incidence and predictors of radial artery spasm during transradial coronary angiography and intervention. Chin Med J. 2010;123:843-847.
13. Candemir B, Kumbasar D, Turhan S, Kilickap M, Ozdol C, Akyurek O,et al. Facilitation of radial artery cannulation by periradial subcuta-neous administration of nitroglycerin. J Vasc Interv Radiol. 2009;20:1151-1156.
14. Goldberg SL, Renslo R, Sinow R, French WJ. Learning curve in the use of the radial artery as vascular access in the performance of percutaneous transluminal coronary angioplasty. Cathet Cardiovasc Diagn. 1998;44:147-152.
15. Fukuda N, Iwahara S, Harada A, et al. Vasospasms of the radial artery after the transradial approach for coronary angiography and angioplasty. Jpn Heart J. 2004;45:723-731.
16. Abe S, Meguro T, Endoh N et al. Response of the radial artery to three vasodilatory agents. Catheter Cardiovasc Interv. 2000;49:253-256.
17. He GW, Yang CQ. Radial artery has higher receptor-mediated contractility but similar endothelial function compared with mammary artery. Ann Thorac Surg. 1997;63:1346-1352.
18. He GW, Yang CQ. Characteristics of adrenoceptors in the human radial artery:clinical implications. J Thorac Cardiovasc Surg. 1998;115:1136-1141.
19. Shapira OM, Xu A, Aldea GS, Vita JA, Shemin RJ, Keaney JF Jr. Enhanced nitric oxide-mediated vascular relaxation in radial artery compared with internal mammary artery or saphenous vein. Circulation. 1999;100:II322-7.
20. Zabeeda D, Medalion B, Jackobshvilli S, Ezra S, Schachner A, Cohen AJ. Comparison of systemic vasodilators:effects on flow in internal mammary and radial arteries. Ann Thorac Surg. 2001;71:138-141.
21. Beyer AT, Ng R, Singh A et al. Topical nitroglycerin and lidocaine to dilate the radial artery prior to transradial cardiac catheterization:a randomized, placebo-controlled, double-blind clinical trial:the PRE-DILATE Study. Int J Cardiol. 2013;168:2575-2578.
22. Boyer N, Beyer A, Gupta V, et al. The effects of intra-arterial vasodilators on radial artery size and spasm:implications for contemporary use of trans-radial access for coronary angiography and percutaneous coronary intervention. Cardiovasc Revasc Med. 2013;14:321-324.
23. Carrillo X, Fernandez-Nofrerias E, Ciompi F, et al. Changes in radial artery volume assessed using intravascular ultrasound:a comparison of two vasodilator regimens in transradial coronary interventions. J Invasive Cardiol. 2011;23:401-404.
24. Varenne O, Jegou A, Cohen R et al. Prevention of arterial spasm during percutaneous coronary interventions through radial artery:the SPASM study. Catheter Cardiovasc Interv. 2006;68:231-235.
25. Curtis E, Fernandez R, Lee A. The effect of topical medications on radial artery spasm in patients undergoing transradial coronary procedures:a systematic review. JBI Database System Rev Implement Rep. 2018;16:738-751.
26. Ferrante G, Rao SV, Juni P, et al. Radial Versus Femoral Access for Coronary Interventions Across the Entire Spectrum of Patients With Coronary Artery Disease:A Meta-Analysis of Randomized Trials. JACC Cardiovasc Interv. 2016;9:1419-1434.
Corresponding author: Av. Roca (S) 342, 4º Piso, 4200 Santiago del Estero, Argentine.
E-mail address: sfcoroleu@gmail.com (S. Coroleu).