ABSTRACT
Over the last two decades, several key advances have been made in the field of interventional cardiology including new techniques and treatments, organizational changes such as the management of acute myocardial infarction, and the arrival of satellite catheterization laboratories. All these advances require the updating of the requirements and equipment that are needed in an interventional cardiology unit. This consensus document by the Interventional Cardiology Association of the Spanish Society of Cardiology, the Ischemic Heart Disease and Acute Cardiac Care Association of the Spanish Society of Cardiology and the Spanish Association of Nursing in Cardiology which describes the recommendations that should be followed by percutaneous coronary intervention capable hospitals or centers intend to build interventional cardiology units. It also describes the requirements for provision, qualification of professionals, technological and material resource allocation, and aspects related to supervised catheterization laboratories and structural heart disease programs.
Keywords: Catheterization laboratory. Interventional cardiology. Acute myocardial infarction. Structural heart disease.
RESUMEN
En las últimas dos décadas han tenido lugar grandes avances en el campo de la cardiología intervencionista. Estos incluyen no solo nuevas técnicas y tratamientos, sino también cambios en la organización, como la atención continuada al infarto agudo de miocardio y la aparición de salas tuteladas. Todos estos avances hacen necesaria una actualización de los requisitos y del equipamiento necesarios en una unidad de hemodinámica y cardiología intervencionista. En este documento de consenso de la Asociación de Cardiología Intervencionista de la Sociedad Española de Cardiología, la Asociación de Cardiopatía Isquémica y Cuidados Agudos Cardiovasculares de la Sociedad Española de Cardiología, y la Asociación Española de Enfermería en Cardiología, se establecen las recomendaciones que deberían cumplir los centros hospitalarios donde esté instalada o se pretenda instalar una unidad de hemodinámica y cardiología intervencionista, los requisitos de dotación y cualificación de profesionales, las dotaciones tecnológicas y los materiales necesarios, y aspectos relacionados con las salas tuteladas y los programas de tratamiento de la cardiopatía estructural.
Palabras clave: Sala de cateterismo. Cardiología intervencionista. Infarto agudo de miocardio. Cardiopatía estructural.
Abbreviations:
ACI-SEC: Interventional Cardiology Association of the Spanish Society of Cardiology. AEEC: Spanish Association of Nursing in Cardiology. PCI: percutaneous coronary intervention. PCT: patient care technician. TAVI: transcatheter aortic valve implantation. UIC: unit of interventional cardiology.
INTRODUCTION
Over the last 2 decades, interventional cardiology has been one of the fastest growing medical specialties. The invasive management of acute coronary syndrome, the optimization of short and long-term results of percutaneous coronary intervention (PCI) techniques, and the development of percutaneous techniques to treat a large number of structural heart disease cases have become very popular. This has facilitated the management of patients with cardiovascular diseases who require diagnostic or therapeutic invasive techniques at the unit of interventional cardiology (UIC) at one time or another.
Parallel to this increasing healthcare demand, we have seen another very significant increase in the number of UIC-capable centers, the need for material and human resources, and development of the technology used. Some rules and regulations have changed over the last few years. The latest clinical practice guidelines were published by the Spanish Society of Cardiology (SEC) 20 years ago,1 and the very latest recommendations from the Spanish Ministry of Health were established almost 10 years ago.2 That is why it seems necessary to update these recommendations, in our field, on the hemodynamic and interventional cardiology requirements and adapt them to the current situation where most UICs already have continuous infarction care plans and structural heart programs implemented. For this reason, the Interventional Cardiology Association of the Spanish Society of Cardiology (ACI-SEC), the Spanish Society of Cardiology Working Group on Ischemic Heart Disease and Acute Cardiovascular Care, and the Spanish Association of Nursing in Cardiology (AEEC) have published this document.
HOSPITAL REQUIREMENTS
This document divides cath labs into autonomous cath labs (run with medical personnel from the center) and satellite or supervised cath labs (run with personnel from other centers to secure the provision of healthcare).
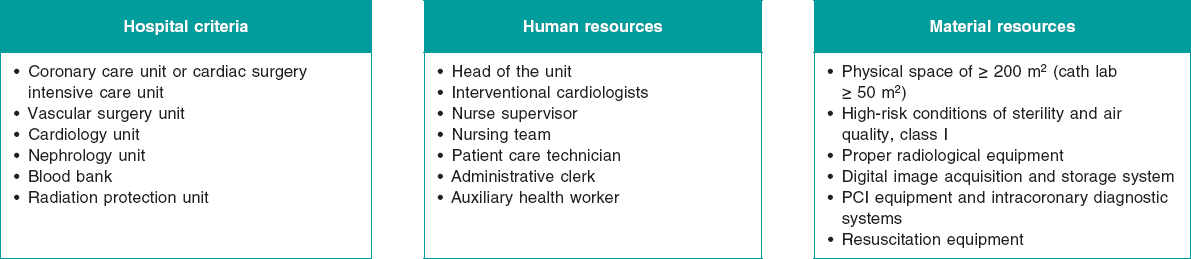
These are the requirements for hospitals to qualify as PCI-capable centers (figure 1):
- Presence of a coronary care unit or cardiac surgery intensive care unit.
- Presence of a cardiology unit and on-call cardiologists are highly recommended as well.
- Ability to treat vascular complications surgically at the center or at a partner center with patient transfer times under 60 minutes.
- Access to a nephrology and dialysis unit.
- Access to a hematology unit and blood bank.
- Access to a radiological protection unit in or out of the hospital setting.
Figure 1. Summary of hospital requirements regarding human and material resources that should become available at the interventional cardiology unit. PCI, percutaneous coronary intervention.
These requirements are applicable both to autonomous and satellite units. Regarding cardiac surgery, its existence in situ should not be considered a requirement per se for the center to qualify as a PCI-capable UIC.3 Also, a protocol needs to be agreed upon with a cardiac surgery unit to facilitate the transfer of patients for emergency surgeries in less than 60 min. Traditionally, structural heart procedures have not been deemed necessary to perform procedures such as valvuloplasties or percutaneous closures of interatrial defects. However, with the rise of structural heart procedures of higher risk and complexity like transcatheter aortic valve implantation (TAVI) or the management of mitral regurgitation using the MitraClip system, this question has gained popularity and the current clinical practice guidelines consider it necessary.
HUMAN RESOURCES
Chief, Director or Head of the UIC
The chief of the UIC should be a cardiologist accredited in the practice of interventional cardiology by the ACI-SEC. Although back in 2011, the Spanish Ministry of Health recommended, at least, more than 5 years of professional practice and over 500 procedures performed,2 we believe the time has come to update these numbers. Therefore, we recommend over 1000 diagnostic procedures and over 500 therapeutic procedures performed.
The basic functions and responsibilities of the head of the UIC are:
- Coordinate healthcare, training and research activities at the UIC.
- Develop and establish procedural protocols, checklists, and outcome assessments.
- Plan the annual objectives of the activities that will be performed and manage the provision of healthcare, education, training, and research at the UIC. Also, elaborate plans with the annual needs of the UIC.
- Implement policies to provide the office material, devices or technologies needed to run the UIC properly.
- Promote the electronic registry of procedures and results and be in charge of sending it to the ACI-SEC annual registry.
- Facilitate the communication and coordination of actions with other cardiology and hospital units.
- See that the rules, regulations, and general policy of both the cardiology unit and the hospital are observed in line with both the cardiology unit and hospital board of directors.
- Draw up an annual report of the activities developed at the UIC.
- Design internal sessions for the training of medical staff and non-professional healthcare workers.
- Participate in the general sessions held at the UIC, especially in the medical-surgical sessions held by the heart team.
- Make sure that the rules and regulations on radiation protection are implemented and being observed. Also, make sure that the UIC personnel has completed the radiation protection courses required by law.
- Be an active leader in and out of the UIC.
- Periodic assessments of:
- The quality of the clinical practice developed at the UIC by creating, reviewing, and updating the protocols of processes as well as diagnostic and therapeutic procedures.
- The activity, productivity, cost, efficiency, and safety of all the activities developed at the UIC.
- The degree of adherence to the goals set by the UIC with periodic follow-ups and problem solving approaches.
Medical staff
As explained in the “Training and competences” section below, the UIC medical personnel should hold a valid degree as cardiology specialists issued in Spain, follow the recommendations established by the ACI-SEC regarding specific training in interventional cardiology,4 and be in possession of the radiation protection course level 2.5
The functions and responsibilities of the interventional cardiologists who work at the UIC are:
- Perform the invasive procedures often performed in interventional cardiology.
- Perform evaluations of patients prior to performing any diagnostic or therapeutic invasive procedures including possible contraindications and individual risk assessments and confirm that the patients’ legally required informed consent is duly signed.
- Make diagnostic and therapeutic decisions based on validated protocols and clinical pathways established by both the hospital and the cardiology unit.
- Know the different procedures included in the UIC repertoire as well as their indications, risks, and methodologies.
- Collaborate with the remaining UIC team and coordinators to achieve the goals set.
- Know how the equipment works, its indications, and functioning.
- Know which structural heart diseases are eligible for percutaneous treatment and its indications.
- When performing structural heart procedures, it is mandatory to know about techniques and procedures, indications, risks, and contraindications. Also, to be competent in the management of all potential complications that may occur.
The recommended number of cardiologists with full dedication to interventional cardiology to provide scheduled care at an UIC with just 1 cath lab and be able to cover vacations is 3. At UICs with 2 cath labs the recommended number of cardiologists with full dedication to interventional cardiology is 5. For every additional cath lab over 2, 1 interventional cardiologist should be added. This is applicable to supervised cath labs too in such a way that in those centers where the UIC acts as the reference to 1 or more supervised cath labs, the number of interventional cardiologists needed should increase by a factor of 1 for every supervised cath lab available. In any case, if the UIC has continuous infarction care plans implemented (on a 24 hour/day basis 365 days/year), the minimum number of interventional cardiologists required for its correct functioning is 4.6 In order to guarantee the availability of continuous infarction care plans, in some centers (especially those with just 1 cath lab) it may be necessary to hire part-time interventional cardiologists who also work in other areas of cardiology.
The UIC accredited health professionals will facilitate and engage themselves in the development of training programs for both internal medicine residents (IMR) and internship recipients as long as the UIC is accredited to that effect. On the other hand, to perform special procedures, other health professionals who may not be part of the UIC such as cardiology specialists (echocardiography specialists or acute coronary care unit cardiologists) and anesthesiologists may be requested.
Nurse supervision
Nurse supervisors should have an adequate level of experience and training in interventional cardiology, as well as other specific functions and responsibilities. It is advisable that they should be accredited as experts in interventional cardiology by the AEEC.7 These are their responsibilities:
- Organize the UIC nursing staff.
- Supervise and coordinate the day’s work together with the head of the UIC.
- Organize the management of patients before and after performing the procedures.
- Prepare and keep the areas involved in observation and care totally operational.
- Implement the hospital protocols and clinical practice guidelines on monitorization, drug therapy, pre- and postoperative care while making sure that the patients’ safety is guaranteed at all times.
- Develop and establish procedural protocols, checklists, and outcome assessments.
- Organize continuous education and training programs for the nursing staff.
- Assess the competence of health professionals.
- Take good care of equipment and tools.
- Make sure that tools and drugs are always available.
Nursing staff
The minimum requirements for the nursing staff who work at the UIC are:
- Hold a bachelor’s degree in nursing.
- Have UIC training and be trained in the kind of procedures performed in this setting at least in the management of diagnostic procedures and PCI techniques.
- Have a radiological protection degree (preferably the level 2 radiological protection course).5
- At least 50% of the nursing team needs to be accredited in interventional cardiology by SEC/ACI-SEC/AEEC.7
Also, the UIC nursing team needs to be competent in cardiovascular care in general and in the early management of patients, their mental preparedness, and be able to handle postprocedural monitorization. Also, they need to be experienced in the management of cardiovascular disease, critical coronary care unit, management of cardiovascular drugs, be skilled starting IVs, experienced using cardiovascular tools, competent in the use of interventional cardiology tools and skilled using them.2,8
Regarding their competences at the UIC, the nursing team can be divided into: instrument nurses, circulating nurses, and polygraph nurse specialists; still, the entire nursing team needs to be competent in the 3 areas described above. The team should also be skilled in preparing the patients before the procedure and immediate monitorization are tasks that should be performed by expert UIC nurses.
The number of nurses required for the proper functioning of the UIC depends on the type of procedure performed. In order to perform diagnostic studies and PCIs, the minimum number of nurses is 2 (in this case, the same nurse does both the circulating and polygraph monitoring tasks) being 3 the ideal number. At least 3 nurses are required to perform structural heart procedures. The AEEC estimates that for quality care purposes, the proper number of nurses at a cath lab should be 3 in order to cover the aforementioned instrument, circulating, and polygraph monitoring tasks.8 In any case, at least 2 of these 3 nurses need to be experts in order to provide safe and quality care for the patients during and after cardiac catheterization.
Radiology technicians
Since radiation protection training is mandatory for both the UIC medical staff and the nursing team, radiology technicians are not considered essential workers at the UIC. Actually, most UICs simply don’t have them among their staff. However, if they are among the UIC staff, they need to take regular care and maintenance of the radiology equipment and know the different software applications and quantitative coronary angiography systems. Also, they need to understand how non-angiographic imaging modalities (intracoronary ultrasound and optical coherence tomography) and physiological systems (intracardiac pressures and intracoronary pressure guidewires) work. Also, they need to make sure that radiation emissions are safe both for the patients and the healthcare personnel.
Patient care technicians and non-professional healthcare workers
Patient care technicians (PCT) play an important role preparing the patients and helping the nursing team. At least 1 PCT needs to be present in UICs with 1 or 2 cath labs, and 2 PCTs in UICs with more than 2 cath labs.
The administrative personnel and auxiliary health workers are essential employees at the UIC. Administrative personnel handle medical appointments and all sorts of healthcare related documents. Auxiliary health workers are in charge of swiftly escorting the patients in and out of the hospital. At least 1 administrative clerk with full dedication to the UIC should be present in large volume centers with more than 1 cath lab. The cleaning personnel prepare the cath lab between cases while maintaining the proper hygienic conditions.
TRAINING AND COMPETENCES
The SEC, through the ACI-SEC, has been implementing an internal accreditation system for healthcare professionals and training centers since 1998.4 The requirements to access this accreditation system and the core curriculum update in interventional cardiology proposed by the European Association of Percutaneous Cardiovascular Interventions (EAPCI)9 are the basis of the recommendations described below.
Interventional cardiology training
Training in interventional cardiology should guarantee an absolute knowledge of all diagnostic and therapeutic invasive techniques available. Over the last few decades, Spanish cardiologists have been treating not only coronary artery disease but also non-valvular10 and valvular11,12 structural heart diseases percutaneously. It is important to stress that interventional cardiologists are also involved in the comprehensive cardiac management of the patients including the indication for the procedure, evaluations using imaging modalities, the management of all possible complications, and clinical follow-up.
The prerequisites to obtain the professional accreditation in interventional cardiology are:
- Hold a medical degree as cardiology specialist issued by the Spanish Ministry of Education.
- Be well-trained in acute cardiac care to treat any possible complications and clinical impairment that may occur while procedures are being performed.
- Have a level 2 accreditation in radiological protection oriented towards the practice of interventional cardiology.5
- Be properly trained in both diagnostic and therapeutic interventional cardiology. According to the accreditation criteria established by ACI-SEC, training should take place over a 2-year period in a UIC licensed and registered to host this kind of training.4 Since certain highly complex procedures are performed in a limited number of large volume centers, training can be carried out in more than 1 national accredited traing centre or international center with a good professional reputation. Ideally, the UIC medical staff should be accredited and licensed for the practice of interventional cardiology. Also, they can be carrying out this training as specialists already hired by the UIC. At the ICU there can be 1 or more cardiologists at different levels of advanced training under the supervision of already accredited interventional cardiologists.
- To have performed, at least, 250 therapeutic coronary procedures, half of them as lead operator. These procedures should be properly documented and certified by the head of the UIC from the center where the training sessions are taking place.
- Master all manual and cognitive skills on the selection of patients, devices, equipment, tools, drugs, information, and writing of documents. In summary:
- Coronary procedures: master all arterial and venous vascular accesses, hemostasis systems, and devices; PCIs for the management of simple lesions and acute coronary syndromes; and be experienced using complex techniques while performing PCIs including intravascular imaging, functional studies, treatment of bifurcations, chronic occlusions, calcified lesions, and implantation of circulatory mechanical support systems.
- Direct participation in the primary angioplasty program for the management of infarction.
- Have theoretical experience and practical knowledge as an assistant operator in structural heart procedures including transcatheter approaches for the management of different heart valve diseases and closures of septal defects, left atrial appendages, and paravalvular dehiscences.
- Know the care provided, and therapy administered to every patient before and after the procedure. Also keep a proper follow-up after hospital discharge.
- Have the capacity to treat all the possible complications that may occur associated with coronary procedures and coadjuvant therapies.
Training centers
In order to guarantee proper training in interventional cardiology, the clinical practice guidelines on the management of myocardial revascularization recommend13 that training should be carried out in large volume centers with an independent UIC and a structured acute coronary syndrome care program on a 24/7 basis.
In Spain, the ACI-SEC has an accreditation program with training centers adapted to the reality of our context that establishes the following minimum requirements4:
- The UIC needs to be included in a cardiology unit accredited by the SEC and the National Specialty Commission for the training of cardiology specialists via IMR.
- The UIC needs to have at least 1 cath lab that should meet all the requirements anticipated by the current Spanish legislation and be certified by the center radiological protection unit including supervision by accredited personnel for manipulation and supervision purposes.
- The center should perform at least 500 PCIs every year. Centers that perform, on average, 500 PICs annually can train a specialist during the first year and a second specialist during the second year. However, centers that perform at least 1000 PCIs/year can train 2 specialists during the first year and 2 during the second year.
- The training program coordinator needs to be competent in all the cognitive and technical activities included in interventional cardiology with an overall historic volume of procedures performed non-inferior to 1000 PCIs and a mean annual activity of 200 PCIs.
- The UIC should offer satisfactory advanced training with enough cases with all the possible subgroups of risk and complexity including PCIs for the management of acute myocardial infarction.
- The presence of a heart team on-call (on a 24/7 basis) for the management of patients with acute coronary syndrome that may require emergency procedures is essential. Similarly, this service should be able to provide immediate care to patients who may experience complications resulting from interventional techniques and procedures.
- The UIC should observe a minimum level of activity and scientific curiosity in interventional cardiology.4
Keeping the accreditation
There is a direct correlation between results and the volume of PCIs performed per center and operator, both regarding PCIs in general and14 in PCIs to treat infarctions.15 In order to remain competent in performing PCIs to treat acute coronary syndrome, interventional cardiologists need to perform at least 75 PCIs every year. This represents a total of 400 PCIs performed each year by PCI-capable centers on a 24/7 basis). They also need to perform at least 75 PCIs each year to treat acute coronary syndromes (a total of at least 200 annual PCIs per center). Ideally, centers and operators with fewer PCIs performed should partner with larger volume centers.13
Under the current accreditation system, at the time this manuscript was being written, in order to maintain competency the ACI-SEC required that every 5 years, all accredited professionals will be compelled to justify the activity developed during this time. The applicants will need to prove that they performed at least a total of 75 annual PCIs documented and certified by the head of the UIC.4
MATERIAL RESOURCES
Physical space
The ideal location of the UIC is a place close or with easy access to the emergency unit and the cardiology unit hospitalization areas. The UIC should be built with the following physical spaces in mind:
- Total area: at least 200 m2.
- Cath lab: it should have at least 50 m2 of useful surface depending on the equipment included in it. The height of the ceiling should be at least 3 meters. Its design should be rectangular, and the walls need to be covered with lead. It should have an entry door for the patients separate from the door that gives access to the control zone. Both doors should also be covered with lead. The entry door to the cath lab needs to have a red light that should automatically turn on when x-rays are activated. The floor should be antielectrostatic.
- Control zone of the radiology equipment and polygraphy machine connected (ideally through a microphone amplifier circuit) to the examination room and separated from it by radiation shielding lead glass. Ideally, it should be located at the smaller side of the cath lab facing the patient table and opposite the radiology equipment. It can be individual for every cath lab or used with several cath labs.
- Technical room hosting the back-up equipment for the angiography system, polygraph, and transmission of images. The current equipment requires less space. Still, 10 m2 are needed based on the specific needs of every manufacturer. It should have its own independent cooling system and all electric wires should be insulated.
- Reception area for patient preparedness and care. It can be an area adjacent to the cath lab or work as a day hospital does. It should be close to the examination rooms and used for pre- and postprocedural care. In the presence of outpatient catheter and PCI programs it is advisable to adapt this space as a day hospital to fit individual chairs or beds for privacy purposes. Every space should have its own individual monitoring system (electrocardiogram, arterial blood pressure, and oxygen saturation), gas outlets, and power sockets. This area needs to be monitored at all times by nurses and doctors in charge of the operations and procedures performed in such areas.
- Storage unit: since it is advisable to leave the fewest possible pieces of equipment at the cath lab (and always stored in specific surgical furniture and appliances) in order to secure the proper conditions of sterility and asepsis, the storage spaces should be big enough to store the material and equipment used during the procedures. Computerized storage control systems integrated into information and replacement systems are advisable and often used in an increasing number of UICs.
- Other zones intended to be part of this area: administrative area, waiting room and briefing room for families, medical report office, waiting room for the medical personnel, locker room for patients and medical personnel, and separate bathrooms.
Conditions of sterility and air quality
UNE regulation 100713 dated September 2005 classified all UICs as high-risk areas16, class I, and categorized them traditionally as operating rooms type B (ISO class 7),17 indicative that the air diffusion system recommended is turbulent flow.
According to UNE regulation 17134018 which classifies hospital aeras based on risk and type of ventilation/filtration used, cath labs are ranked as high-risk areas. The UICs built from 2012 onwards need to meet the aforementioned regulation to guarantee a sterile environment to be able to perform all kinds of minimally invasive procedures like TAVI, left atrial appendage closures, and use of the MitraClip system. Also, the conditions of sterility and asepsis allow us to use these UICs as conventional operating rooms too (for example, for the management of vascular complications). However, UICs built before this regulation became effective are not bound to it unless remodeled (table 1).
Table 1. Conditions of sterility and quality of air that all current cath labs should meet
| • Minimum advisable flow recirculation with 25 movements/hour of which ≥ 1200 m3/h should be with fresh air from outside |
| • Single air-handling unit |
| • Recirculated air should be treated exactly the same as the outside air by the same air-conditioner |
| • Periodic microbiological tests |
| • Air velocity at the room occupancy area between 0.2 m/s and 0.3 m/s |
| • Have, at least, 3 levels of filtration including these types of filters: |
| - Pre-filter EU4 |
| - Air-conditioning EU9 air filter |
| - Final H13 filter in the surgical area |
UICs should provide enough surgical coverage to perform procedures under conditions of sterility. The use of disposable material is also advised.19 Under conditions of special risk of infection for healthcare personnel, personal protection equipment is advised.20 In any case, all measures related to sterility at the cath lab and infection avoidance for the healthcare personnel should be discussed with both the preventive medicine and risk management units.
Radiology equipment and clinical support systems
In general, the UIC radiological and additional equipment should include (figure 2):
Figure 2. Equipment present at the cath lab. 1: patient table. 2: x-ray tube. 3: radiation shielding lead glass with upper leaded glass section and articulated adjustable arm mounted on the ceiling. 4: leaded skirt mounted on the table. 5: automated contrast media injector. 6: on/off ceiling light with adjustable articulated arm. 7: monitors. 8: infusion pumps. 9: anesthetic and respiratory equipment. 10: crash cart or code cart with defibrillator. 11: smart cabinet for material storage with automatic replacement. 12: table with the equipment needed to perform the procedure. 13: console of the pressure wire.
- A 100 kW-standard X-ray generator.
- Flat-panel imaging digital detector with field sizes big enough to facilitate the use of coronary and structural techniques. Twenty inches is the recommended size.
- Collimation system.
- Anticollision systems are mandatory to avoid short range collisions with the patients. Also, a grid should be incorporated to the system.
- Ceiling or floor mounted motorized arm with iso centric tilt movement and possibility of cranial and caudal ≥ ± 40° and lateral and oblique ≥ ± 90° angulations without having to move table or patient.
- Examination table: low-attenuation carbon fiber board or equivalent with longitudinal and cross-sectional movement capabilities—automatic or manual—and electromagnetic system blocking system on the table. Vertical movement needs to be motorized. Also, it needs to include accessories and outlets to adapt additional components (injector pump, polygraph, consoles for coronary physiology monitoring, etc).
- Contrast injector: automatic injectors are advised but not required.
- Monitors: mounted on the ceiling and movable or adjustable for correct visualization. The monitor can be a single ≥ 55-inch flat screen or multiple ≥ 19-inch monitors. They need to show at least 3 different imaging sources such as real-time radiological images, the reference radiological image, polygraphy, echocardiogram, intracoronary ultrasound, optical coherence tomography, computerized tomography scan or fusion tools.
- Polygraph: it should display continuous ECG monitoring, invasive arterial pressure with at least 2 independent pressure transducers, oxygen saturation through pulse oximetry, cardiac output cable, hemodynamic wave data recording, and be capable of processing hemodynamic data (eg, valvular areas, vascular resistances, gradients, and cardiac output). It needs to be programmed with software that should allow the reception of the working list, the sending of information to a storage system, and the transmission of images with storage and post-processing editing capabilities. Ideally, it should be controlled from the examination table and the working station should be located in the control zone outside the cath lab.
- We should be able to generate final reports on the procedure performed including data from the Kerma-air product (KAP) and dose-area product (DAP) that will be included in the patient’s medical history.
- Radiological contrast: iso-osmolar contrast media are advised since they are associated with a lower risk of contrast-induced nephropathy.
- Radiological protection systems:
- Protective lead curtains for the examination table, at least where the table controls are located and on the side where the procedure will be performed. The minimum lead cover should be 0.5 mm thick.
- Suspended and articulated transparent protection shield to protect the exposed medical personnel who participate in the procedure and remain close to the patient table. At the same time, it facilitates the visualization of the patient and should adapt to the patient contour.
- Radiological protection equipment for the medical staff: lead aprons, lead thyroid collar cover, lead glasses, and dose meters.
- Cold light operating lamp: hanging from the ceiling from an articulated arm and highly movable to light up specific sections of the surgical field.
- Intercommunicator between the examination room and the control room.
- Uninterruptible power supply systems for monitorization and life support purposes. Also, if possible, radiological equipment with enough power (15 min) to perform a fluoroscopy in case of possible power cuts.
Image acquisition systems and storage
The image acquisition system should be digital with a proper dynamic range for routine clinical applications. It should cover the low doses of the different imaging modalities of x-rays and the higher doses of digital acquisition including the most demanding ones of the digital subtraction angiography. The frequency range in pulsed fluoroscopy or graphic representation should be of 30 or more images per second. It should allow processing, visualization, and digital storage.
This equipment needs to include coronary and ventricular quantification applications. Currently, there are applications available for quantitative computed tomography assessment to plan procedures, and fusion systems of transesophageal echocardiography plus digital angiography that can be useful when performing interventional procedures to treat structural heart diseases.
The images of every patient will be saved and stored permanently in a filing system compatible with multiple DICOM modality worklist services (digital imaging and communication on medicine) of cardiac images with integrated DICOM-3 services. These images need to be stored in the corresponding hospital or health service PACS (picture archiving and communication system) so that all studies can be seen and analyzed from the different working stations connected to this server. For that purpose, TCP/IP communications protocols (transmission control protocol/ internet protocol) are required. These protocols should be used in full compliance with data protection legislation. The capabilities of compact disc and digital versatile disc recording and reading are advisable in compliance with the DICOM standard anticipating the possibility of exporting images and angiographic series to other imaging formats.
For real-time image processing and simultaneous image acquisition purposes, a working station will be required for case review and analysis that will join the working station of the image acquisition system. It should be located in the same control zone as the x-ray and polygraph equipment.
Resuscitation and life support systems
UICs should have specific resuscitation and life support systems:
- Crash carts or code carts: the entire UIC staff should be trained in cardiopulmonary resuscitation techniques. The cart should be placed at the patient’s bedside and include the following components that should be reviewed periodically:
- Defibrillator/monitor equipped with transcutaneous pacing capabilities.
- Oxygen administration systems.
- Orotracheal intubation equipment (laryngoscope and tubes).
- Ventilation system.
- Aspiration system.
- Drugs required for hemodynamic drug support, sedation, and management of cardiorespiratory arrest.
- Ventilator.
- Infusion pumps.
- Temporary transvenous pacemaker insertion equipment (electrocatheter and generator).
- Pericardiocentesis kit.
Specific material to perform coronary interventions
Added to the conventional material used to achieve diagnosis and perform coronary interventions (diagnostic catheters, guide catheters, angioplasty guidewires, angioplasty balloons, and coronary stents), it is advisable to have specific coronary stents available to treat coronary perforations, and plaque modification devices to treat nondilatable coronary lesions with conventional balloon or heavily calcified coronary lesions.21
Intracoronary diagnostic tools
In a large number of patients, the use of pressure guidewires or intracoronary imaging modalities will be required as established by the latest clinical practice guidelines on the management of myocardial revascularization.13
Clinical practice guidelines consider pressure guidewires as the proper tool to identify hemodynamically relevant coronary lesions in stable patients (indication class I, level of evidence A) and guide revascularization in patients with multivessel disease (indication class IIa, level of evidence B).13
Also, clinical practice guidelines indicate the use of intracoronary imaging modalities (both intracoronary ultrasound and optical coherence tomography) to study the mechanisms of stent failure and for implant optimization purposes in selected patients (indication class IIa, level of evidence B). Also, intracoronary ultrasound is considered the imaging modality of choice to study the severity of left main coronary artery lesions and for result optimization purposes (indication class IIa, level of evidence B)13.
Therefore, we believe it is necessary for UICs to have functional assessment methods available (eg, pressure guidewires) and intracoronary imaging modalities as well.
Circulatory support systems
Circulatory support systems are required at the UIC to approach complex angioplasties in high-risk patients and for the management of hemodynamically unstable patients or cardiogenic shock. Actually, this is very important in centers with continuous infarction care programs running, especially large volume centers and satellite cath labs without surgical coverage in situ. These systems can be:
- Intra-aortic counterpulsation balloon: catheters should be available at the UIC. However, the console can be stationed at the coronary care unit or cardiac surgery intensive care unit. It should be adaptable to any type of balloon, portable, and have a minimum power supply of 3 hours.
- Percutaneous left ventricular assist devices: the most commonly used one is transaortic microaxial blood pump. It is used for the management of patients with cardiogenic shock and to approach very high-risk PCIs. Its use should follow the recommendations established by the clinical practice guidelines.
- Venoarterial extracorporeal membrane oxygenation: this system is advisable in large volume centers that treat patients with refractory cardiogenic shock, cardiac arrest that remains unresponsive to cardiopulmonary resuscitation maneuvers, and refractory malignant ventricular arrythmias.
SPECIFIC CONSIDERATIONS
Supervised cath labs
Over the last decade, the model of satellite or supervised cath labs in large volume center units has been widely implemented. The reason for this is to bring coronary intervention techniques to a larger number of centers so patients can have access to these services without detriment to the advantages that experienced tertiary levels bring. The characteristics of a satellite or supervised cath lab are:
- The interventional cardiology staff is stationed in another reference unit but still provides coverage to this center to perform the procedures required.
- The head of the satellite cath lab and the head of the reference UIC where the medical staff is stationed is the same person.
- In general, these satellite cath labs are implemented in level II hospitals without cardiac surgery in situ.
-
The requirements of these centers are:
- They should meet all remaining requirements and have the same support units as an autonomous cath lab.
- They require fewer medical staff and health professionals compared to the reference unit. Actually, 1 interventional cardiologist should be enough. At least 2 nurses should be available. However, 3 nurses are advisable per satellite cath lab and day of occupancy. The medical personnel should be stationed at the reference center. The nursing staff and auxiliary health workers can be stationed at the hospital where the satellite cath lab is located.
- A prior written informed consent model needs to be implemented including the fact that emergency surgeries will be performed in a different partner center.
- Patient transfer time to the reference center when emergency surgery is required will not exceed 60 minutes.
A written agreement will need to be signed between the management of both centers for the provision of these services including a budget with all the expenses derived from buying the material required. These centers can be included in healthcare networks.
According to the legislation that regulates the planning and arrangement of the healthcare services provided by each Spanish autonomous community, satellite cath labs can have extraordinary continuous activity programs available on a 24/7 basis 365 days/year to provide urgent care especially within the framework of institutional infarction code programs. The implementation of these programs will be the sole responsibility of the reference UIC.
Structural heart procedures or urgent procedures will not be performed in the supervised cath lab. but in the reference center. However, very complex coronary procedures or interventions requiring special devices in clinically stable patients are ill-advised and they should be performed at the reference center.
Optimization of the infarction care program (primary angioplasty program)
The requirements and needs of infarction care networks have already been described in detail.6 In summary, hospitals with primary angioplasty programs require:
- A coronary care unit or general intensive care unit with levels of care 2 and 3 according to the Acute Cardiovascular Care Association.22
- Cardiologists on call physically present.
- A cardiac surgery unit capable of treating infarction related mechanical complications, or at least partnerships with centers with other cardiac surgery units, capable of transfering patients in less than 60 minutes.
-
Added to the material required to sustain life support and perform resuscitation maneuvers, UICs with infarction code care programs should include ventricular assist devices too. These UICs require a 24/7 on-call service throughout the year. The personal requirements for training and accreditation purposes are:
- At least 4 ACI-SEC- accredited interventional cardiologists in the on-call medical staff.
- A total of over 400 PCIs performed at the UIC every year. Also, each operator should perform at least 75 PCIs and 30 primary angioplasties each year.
- At least 2 nurses on-call and 1 PCT are required with proper training performing procedures in situ with the operators and expertise in the equipment used. It is advisable that the whole nursing staff should be part of the UIC.
- The quality of the program should be assessed using some sort of control mechanism including reperfusion times and mortality results. Similarly, it is advisable to participate in a regional or national registry to guarantee that the quality control process is properly carried out.
Structural heart intervention programs
The specific recommendations to perform structural heart procedures are:
- To perform structural heart procedures, interventional cardiologists should have been accredited in hemodynamics and interventional cardiology by the ACI-SEC at an accredited center. This training qualifies the accreditee to be able to perform PCIs.
- At least 2 cath labs are required in centers that perform structural heart procedures, to be able to assist the infarction care network while long structural heart procedures are still underway.
- UICs capable of performing structural heart procedures should have enough room for the echocardiography specialist and anesthesiologist when required.
- Transesophageal echocardiography (ideally with a 3D probe) is required. The availability of intracardiac echocardiography at the UIC setting is not mandatory and its use is regulated by the recommendations established by the clinical practice guidelines.
- The availability of cardiac surgery in centers that perform structural heart procedures like such as valvuloplasties (mitral, aortic or pulmonary) or percutaneous closures of interatrial septal defects or other short circuits has traditionally not been considered a necessity. The general recommendations established for all UICs apply here too when these procedures need to be performed (possibility of patient transfer in less than 60 minutes to a center with cardiac surgery capabilities). These are also the recommendations established to approach the closure of left atrial appendage.23 Regarding TAVI, developed by cardiology almost 20 years ago,24 the current clinical practice guidelines require the availability of cardiac surgery at the treating center,25,26 although these requirements may change in the future.27 The recommendations established for the management of the MitraClip system regarding the need for surgery are similar to those established for TAVI.28
- Hybrid cath labs are not required, but if structural heart procedure is performed in an operating room, it should include all the necessary equipment for constant hemodynamic monitorization purposes, a kinescope, and high-quality fluoroscopy with possibility of a wide array of angles, projections, and image storage; a mobile C-arm would not be suitable here. In this case, the necessary equipment to perform PCIs, implant transvenous pacemakers, use different types of vascular introducers of different sizes and lengths, as well as bailout devices in cases of device migration, transseptal puncture equipment and pericardiocentesis kit, vascular closure devices, and devices to perform vascular interventions will also be required.
- High-resolution monitors are required for the simultaneous visualization of hemodynamic monitorization images (pressures, electrocardiogram, oxygen saturation). Also, they need to be able to show images acquired using other imaging modalities like echocardiography.
- Two operators and 3 nurses are needed to perform structural heart procedures. In some cases, 1 echocardiography specialist and 1 anesthesiologist may be required. The presence of a cardiac or vascular surgeon may be required too to perform certain procedures.
- The head of the UIC or the coordinators of the structural heart program should be cardiologists with at least 1 year of specific training in structural heart procedures in a large volume centers, experienced in this kind of procedure. Also, they should have at least 5-year experience performing interventional procedures (both PCIs and noncoronary interventional techniques) including transseptal punctures, valvular procedures, and intracardiac device implantation and retrieval. If experience is limited with some of the techniques described, these procedures should be supervised until the proper experience has been gained.
- The number of procedures recommended for both the center and the operator is well-defined for TAVI: at least 50 per year.29 This is the case with transfemoral TAVI, the only access of which there is evidence in randomized clinical trials as an alternative to aortic valve replacement surgery. Clinical practice guidelines are a little unclear regarding other techniques.30-32 However, our recommendation is that at least 15 left atrial appendage closures and percutaneous mitral valve repairs and 10 percutaneous closures of interatrial septal defects should be performed every year.
- Centers capable of performing structural heart procedures will need to send the data from the procedures performed to the official registries of the ACI-SEC and the SEC. Also, data will be subject to the consequences that may arise from supervising these data.
Latest programs: cardiac arrest code and management of acute pulmonary embolism
Over the last few years, the management of cardiac arrest and acute pulmonary embolism has improved significantly. Actually, interventional cardiology has progressively gained interest in these conditions.
Regarding cardiac arrest, performing emergency coronary angiographies to treat acute coronary syndrome can bring clinical benefits. Our recommendation is that patients with out-of-hospital cardiac arrests should be transferred to specific centers. Actually, this kind of care for this type of patient has become a customary practice for some hospitals and is now called “cardiac arrest code”. Requirements for these centers are:
- Inclusion in an acute myocardial infarction care network.
- Cardiologists on call.
- Coronary care unit or cardiac surgery intensive care unit with circulatory support system implantation capabilities.
- Capability of performing therapeutic hypothermia.
- Neurology/neurophysiology unit.
Maastricht types III and IV controlled asystole organ donation programs are not required but highly recommended.
Regarding acute pulmonary embolism, more and more UICs have included the management of this condition in their repertoire using embolectomy catheters in hemodynamically compromised patients contraindicated for thrombolysis.
Based on experience and efficiency, both the cardiac arrest code and the management of pulmonary embolism should be handled by personnel from the continuous infarction care program-according to the internal reality of every hospital and the healthcare regulations of the department of health of the Spanish autonomous community concerned.
CONCLUSION
Over the last few years, the wide invasive management of acute coronary syndrome, development of acute myocardial infarction care networks, creation of supervised cath labs, the arrival and development of new diagnostic and therapeutic coronary techniques and coronary interventions for the management of structural heart disease, as well as legislation changes have changed the equipment, and human resources associated with UICs. This document comes as a response to the need for adapting the current situation to the recommendations in our context regarding requirements in hemodynamics and interventional cardiology. In the future, the recommendations published in this document will need to be updated based on the future steps interventional cardiology may take.
FUNDING
No funding.
CONFLICTS OF INTEREST
The authors declared no conflicts of interest regarding this manuscript. R. Moreno is associate editor of REC: Interventional Cardiology; the editorial protocol of the journal was observed to guarantee an impartial manuscript handling.
REFERENCES
1. Morís de la Tassa C, Cequier Fillat A, Moreu Burgos J, Pérez Hernández H, Aguirre Salcedo JM. Guías de práctica clínica de la Sociedad Española de Cardiología sobre requerimientos y equipamiento en hemodinámica y cardiología intervencionista. Rev Esp Cardiol. 2001;54:741-750.
2. Palanca Sanchéz I, Castro Beiras A, Macaya Miguel C, Elola Somoza J, Bernal Sobrino JL, Paniagua Caparrós JL;Grupo de Expertos. Unidades asistenciales del área del corazón:estándares y recomendaciones. Madrid:Ministerio de Sanidad, Política Social e Igualdad;2011.
3. Esplugas E, Hernández RA, López Bescós L, Moreu J, Pomar JL. The performance of coronary angioplasties at centers without cardiac surgery. The recommendations of the Sociedad Española de Cardiología. Rev Esp Cardiol. 1999;52:5-12.
4. Sistema de acreditación para el ejercicio y la enseñanza de Hemodinámica y Cardiología Intervencionista dirigido a Profesionales y Unidades de Formación. Asociación de Cardiología Intervencionista de la Sociedad Espa-ñola de Cardiología (ACI-SEC). Available online: https://www.hemodinamica.com/institucional/ acreditacion/. Accessed 23 Sep 2020.
5. Orden SCO/3276/2007, de 23 de octubre, por la que se publica el Acuerdo de la Comisión de Recursos Humanos del Sistema Nacional de Salud, mediante el que se articula el segundo nivel de formación en protección radiológica de los profesionales que llevan a cabo procedimientos de radiología intervencionista. Available online: https://www.boe.es/eli/es/o/2007/10/23/sco3276. Accessed 23 Sep 2020.
6. Cequier A, Pérez de Prado A, Cid AB, et al. Requisitos y sostenibilidad de los programas de ICP primaria en España en el IAMCEST. Documento de consenso de SEC, AEEC y SEMES. REC Interv Cardiol. 2019;2:108-119.
7. Gómez M, Rodríguez V, Pedrosa CP, et al. Perfil Profesional de Enfermería de Hemodinámica y Cardiología Intervencionista. Sistema de Acreditación Competencias Avanzadas. 2018. Available online:http://hemodinamica.enfermeriaencardiologia.com/wp-content/uploads/documento-de-perfil-normas-de-acreditacion.pdf Accessed 23 Sep 2020.
8. Fernández JM, García FJ, Gómez M, et al. Manual de Procedimientos de Enfermería en Hemodinámica y Cardiología Intervencionista. Madrid:Asociación Española de Enfermería en Cardiología;2014.
9. Van Belle E, Teles R, Pyxaras S, et al. Core curriculum EAPCI. EAPCI core curriculum for the interventional cardiologists. Committee for Education and Training. EuroIntervention. 2020. https://doi.org/10.4244/EIJ-D-18-00448.
10. Zabala Argüelles JI, García E, Zunzunegui Martínez JL, et al. Cierre percutáneo de la comunicación interauricular:resultados a medio plazo de esta nueva opción terapéutica. Rev Esp Cardiol. 2000;53:21-6.
11. Calvo OL, Sobrino N, Gamallo C, Oliver J, Dominguez F, Iglesias A. Balloon percutaneous valvuloplasty for stenotic bioprosthetic valves in the mitral position. Am J Cardiol. 1987;60:736-737.
12. Medina A, Bethencourt A, Coello I, Hernandez E, Goicolea J, Melián F, et al. A new type of adjustable vascular introducer for balloon valvuloplasty:technical note. Cardiovasc Intervent Radiol. 1989;12:169-171.
13. Neumann FJ, Sousa-Uva M, Ahlsson A, et al.;ESC Scientific Document Group. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40:87-165.
14. Hannan EL, Wu C, Walford G, et al. Volume-outcome relationships for percutaneous coronary interventions in the stent era. Circulation. 2005;112:1171-1179.
15. Nallamothu BK, Wang Y, Magid DJ, et al. National Registry of Myocardial Infarction Investigators. Relation between hospital specialization with primary percutaneous coronary intervention and clinical outcomes in ST-segment elevation myocardial infarction:National Registry of Myocardial Infarction-4 analysis. Circulation. 2006;113:222-229.
16. UNE. UNE 100713:2005. Instalaciones de acondicionamiento de aire en hospitales. Available online: https://www.une.org/encuentra-tu-norma/busca-tu-norma/norma/?c=N0034264. Accessed 23 Sep 2020.
17. UNE. UNE 14644-1:2016. Salas limpias y locales anexos. Parte 1:Clasificación de la limpieza del aire mediante la concentración de partículas (ISO 14644-1:2015). Available online: https://www.une.org/encuentra-tu-norma/busca-tu-norma/norma/?c=N0057435. Accessed 23 Sep 2020.
18. UNE. UNE 171340:2020. Validación y cualificación de salas de ambiente controlado en hospitales. Available online: https://www.une.org/encuentra-tu-norma/busca-tu-norma/norma/?c=N0064465. Accessed 23 Sep 2020.
19. European Committee for Standardization. European Standard EN 137951:2019. Surgical clothing and drapes Requirements and test methods Part 1: Surgical drapes and gowns. Available online: https://www.sls.se/media/v3hf5pb1/pren-13795-1.pdf. Accessed 23 Sep 2020.
20. Romaguera R, Cruz-González I, Ojeda S, et al. Gestión de las salas de procedimientos invasivos cardiológicos durante el brote de coronavirus COVID-19. Documento de consenso de la Asociación de Cardiología Intervencionista y la Asociación del Ritmo Cardiaco de la Sociedad Española de Cardiología. REC Interv Cardiol. 2020;2:106-111.
21. Cubero-Gallego H, Tizón-Marcos H, Vaquerizo B. Opciones actuales para el tratamiento de las lesiones calcificadas. REC Interv Cardiol. 2020;2:129-139.
22. Bonnefoy-Cudraz E, Bueno H, Casella G, et al. Editor's Choice —Acute Cardiovascular Care Association Position Paper on Intensive Cardiovascular Care Units:An update on their definition, structure, organisation and function. Eur Heart J Acute Cardiovasc Care. 2018;7:80-95.
23. Glikson M, Wolff R, Hindricks G, et al. EHRA/EAPCI Expert Consensus Statement on Catheter-Based Left Atrial Appendage Occlusion —An Update. EuroIntervention 2020;15:1133-1180.
24. Cribier A, Eltchaninoff H, Bash A, et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis:first human case description. Circulation. 2002;106:3006-3008.
25. Baumgartner H, Falk V, Bax JJ, et al.;ESC Scientific Document Group. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2017;38:2739-2791.
26. Bavaria JE, Tommaso CL, Brindis RG, et al. 2018 AATS/ACC/SCAI/STS Expert Consensus Systems of Care Document:operator and institutional recommendations and requirements for transcatheter aortic valve replace ment. J Am Coll Cardiol. 2019;73:340-374.
27. Jiménez Quevedo P, Pan M, Moreno R, Pérez de Prado A. Scientific evidence versus expert opinion. Should we modify clinical practice guidelines?Rev Esp Cardiol. 2020;73:187-189.
28. Nishimura RA, O'Gara PT, Bavaria JE, et al. 2019 AATS/ACC/ASE/SCAI/ STS Expert Consensus Systems of Care Document:A Proposal to Optimize Care for Patients With Valvular Heart Disease:A Joint Report of the American Association for Thoracic Surgery, American College of Cardi ology, American Society of Echocardiography, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2019;73:2609-2635.
29. Wassef AWA, Rodes-Cabau J, Liu Y, et al. The learning curve and annual procedure volume standards for optimum outcomes of transcatheter aortic valve replacement:findings from an international registry. JACC Cardiovasc Interv. 2018;11:1669-1679.
30. Glikson M, Wolff R, Hindricks G, et al.;ESC Scientific Document Group. EHRA/EAPCI expert consensus statement on catheter-based left atrial appendage occlusion —an update. EuroIntervention. 2020;15:1133-1180.
31. Chhatriwalla AK, Vemulapalli S, Holmes DR Jr, et al. Institutional Experience With Transcatheter Mitral Valve Repair and Clinical Outcomes:Insights From the TVT Registry. JACC Cardiovasc Interv. 2019;22:1342-1352.
32. Horlick E, Kavinsky CJ, Amin Z, et al. SCAI expert consensus statement on operator and institutional requirements for PFO closure for secondary prevention of paradoxical embolic stroke. Catheter Cardiovasc Interv. 2019;93:859-874.