CASE RESOLUTION
Immediate shock after transcatheter aortic valve implantation (TAVI) is a rare complication that requires quick diagnosis and treatment.
The causes are alterations of the area adjacent to the implant (aortic regurgitation, aortic annulus complications or ischemia due to occlusion or coronary artery embolism), complications distant from the implant area (perforations associated with the pacemaker or the support guidewire in the left ventricle or mitral apparatus alterations) or vascular complications (in the femoroiliac access or the aorta). All of these complications were discarded in our female patient.
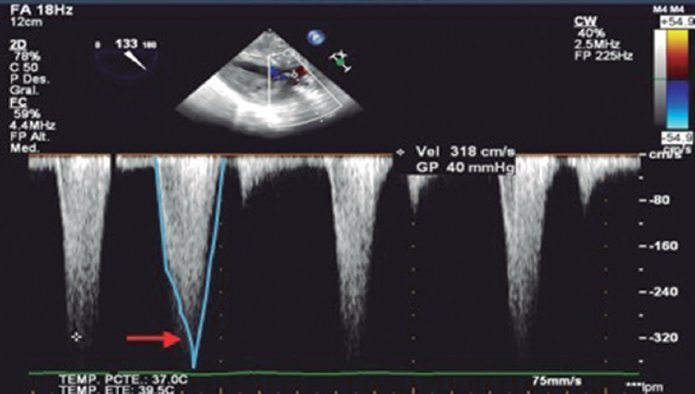
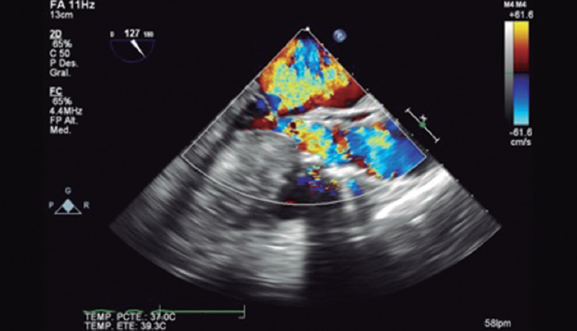
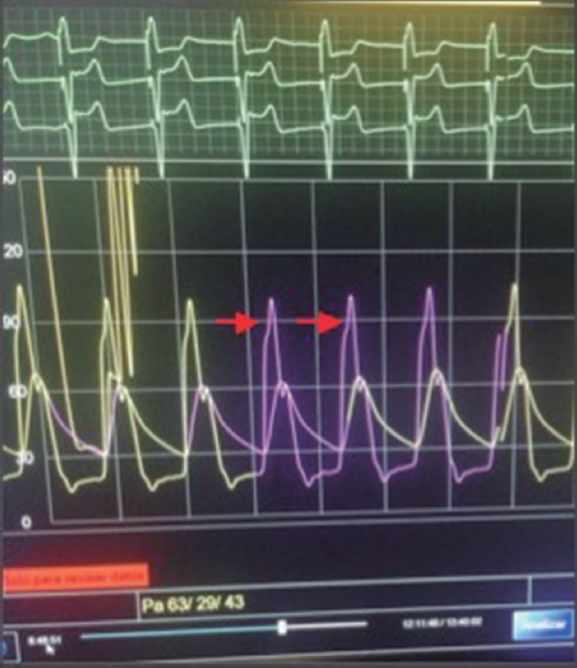
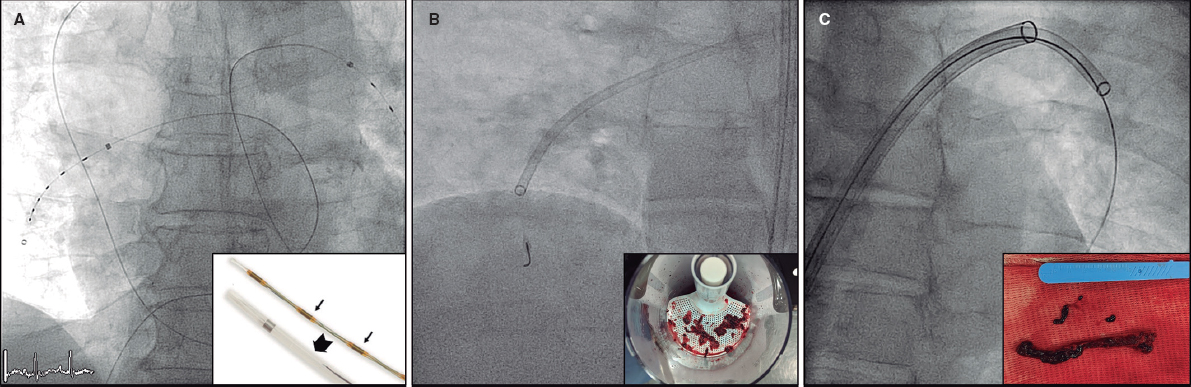
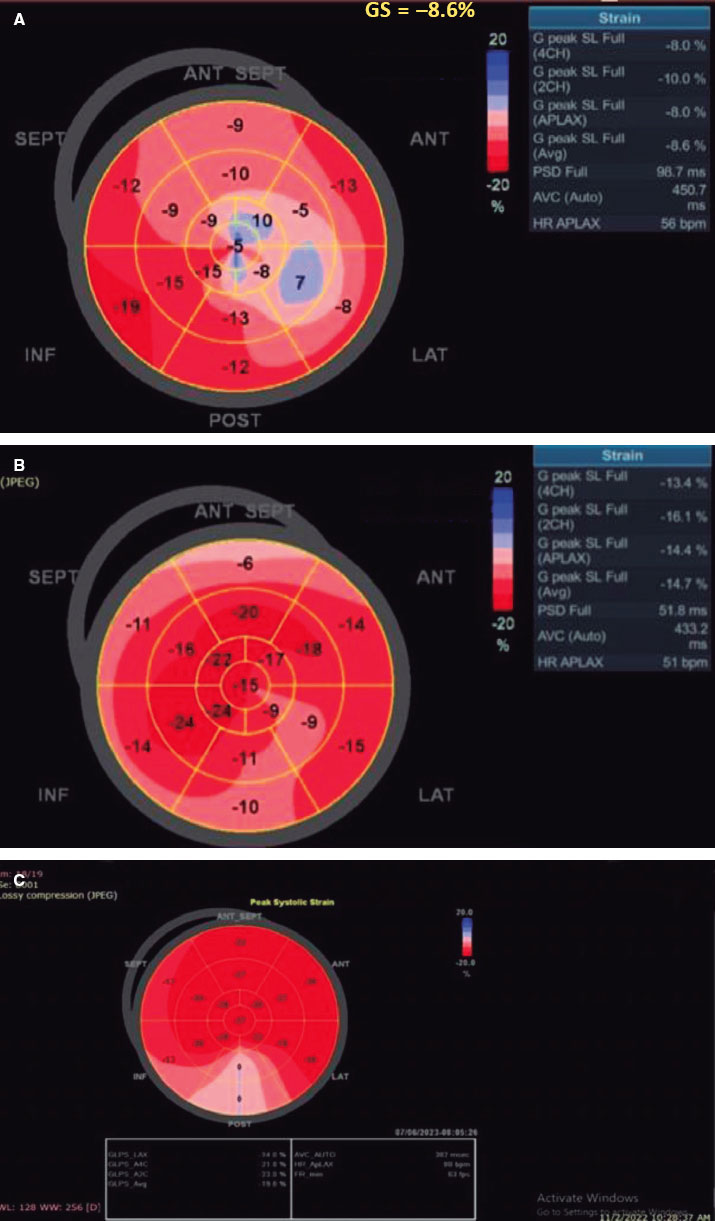
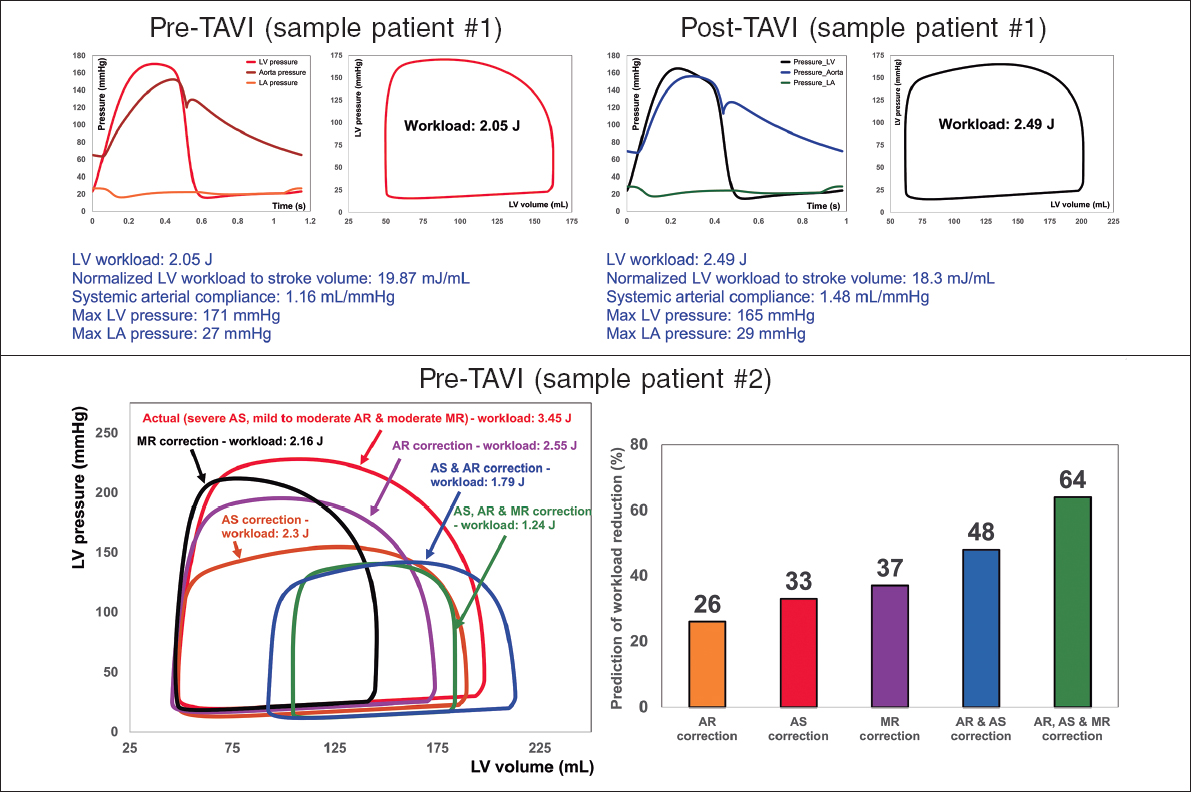
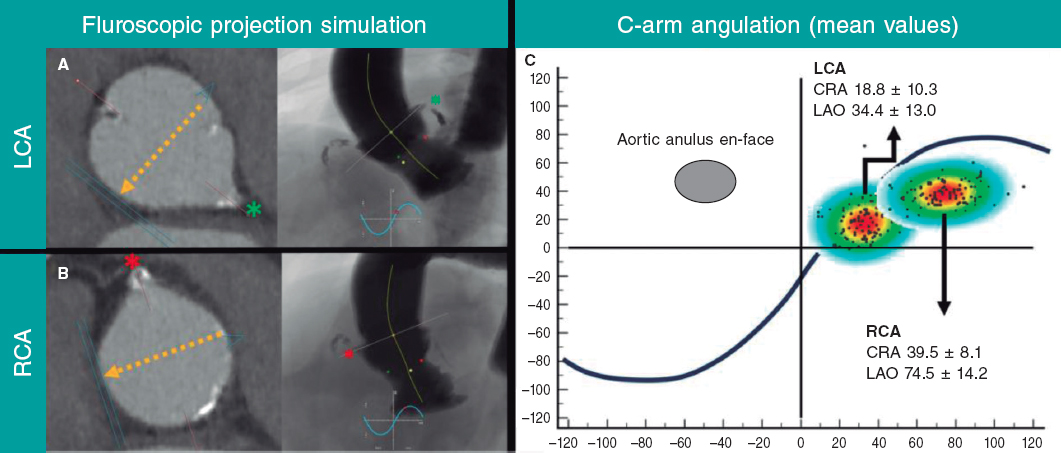
The videos of the case presentation suggested a suspected rare cause for the shock: suicide left ventricle consisting of ventricular collapse that triggers dynamic obstruction (video 1 of the supplementary data). The intraventricular gradient (figure 1) can generate anterior systolic movement of the mitral valve and severe mitral regurgitation (figure 2). A catheter was advanced to the apex that confirmed the severe intraventricular dynamic gradient (figure 3).
Figure 1. Intraventricular dynamic gradient with late peak (arrow).
Figure 2. Flow acceleration due to dynamic obstruction, anterior systolic movement of the mitral valve, and severe mitral regurgitation.
Figure 3. Registry of aortic and left ventricular pressures immediately after TAVI: intraventricular dynamic gradient with late peak (arrows). No withdrawal, multimodal diagnosis.
Targeted therapy with fluid therapy was used to optimize preload followed by IV esmolol, and phenylephrine. Also, the rhythm itself was optimized in order to keep atrioventricular synchrony and extend the diastolic filling period. This made the gradient go away (figure 4) and improved the patient’s hemodynamic situation.
Figure 4. Registry of aortic and left ventricular pressures after treatment; gradient resolution.
Progression was good and sustained in time. The control echocardiography performed at the hospital discharge showed a minimum dynamic gradient without anterior systolic movement of the mitral valve treated with atenolol (25 mg/day).
The chronic increase of ventricular postload due to aortic stenosis can trigger myocardial hypertrophy and intraventricular gradient that are masked by a fixed valvular obstruction.1 However, after implanting the valve it triggers a series of hemodynamic changes that can unmask this gradient2 and eventually lead to hemodynamic collpase.1
The importance of the case is that in the presence of sudden hypotension, vasopressor drugs are often used. However, they can deteriorate both the intraventricular gradient and hypotension by increasing inotropism; that is why it is essential to be aware of this condition and use beta-blockers.1
There are echocardiographic data available on the baseline study to predict the higher risk of developing suicide left ventricle1
FUNDING
No funding.
AUTHORS' CONTRIBUTION
All authors prepared and revised the article.
CONFLICTS OF INTEREST
None declared.
SUPPLEMENTARY DATA
Vídeo 1. Barrionuevo Sánchez M. I. DOI: 10.24875/RECICE.M20000161.
REFERENCES
1. Suh WM, Witzke CF, Palacios IF. Suicide left ventricle following transcatheter aortic valve implantation. Catheter Cardiovasc Interv. 2010;76:616-620.
2. Alfonso F, Domínguez L, Rivero F, et al. Severe intraventricular dynamic gradient following transcatheter aortic valve implantation:Suicide ventricle?EuroIntervention. 2015;11:e1.
3. Gerckens U, Pizzulli L, Raisakis K. Alcohol septal ablation as a bail-out procedure for suicide left ventricle after transcatheter aortic valve implantation. J Invasive Cardiol. 2013;25:E114-E117.
Corresponding author: Servicio de Cardiología, Hospital Universitari de Bellvitge, Feixa Llarga s/n, 08907, L’Hospitalet de Llobregat, Barcelona, Spain.
E-mail address: bsanchezmarisa@gmail.com (M.I. Barrionuevo Sánchez).