CASE PRESENTATION
This is the case of a 72-year-old woman with a past medical history of permanent atrial fibrillation treated with acenocoumarol, and rheumatic valvular heart disease that appears as a double severe mitral lesion and severe tricuspid regurgitation due to annular dilatation with dyspnea-like symptoms. The cardiologic examination completed before planning valve replacement surgery discarded the presence of coronary lesions. The case was presented to the medical-surgical committee and approved for mitral valve replacement, and tricuspid annuloplasty.
Procedure was performed electively with a 25 mm On-X 25 prosthetic mechanical mitral valve (Life Technologies, GA, United States) followed by tricuspid annuloplasty with annular prosthesis. After weaning from extracorporeal support and circulation machine, a hemorrhage was revealed due to the rupture of the atrioventricular groove in the vicinity of left atrial appendage that was repaired with suture reinforcement on the pericardium and Teflon until achieving hemostasis. In this context, the patient showed hemodynamic impairment, and ventricular function deterioration that required escalating the inotropic support, and intra-aortic balloon pump implantation.
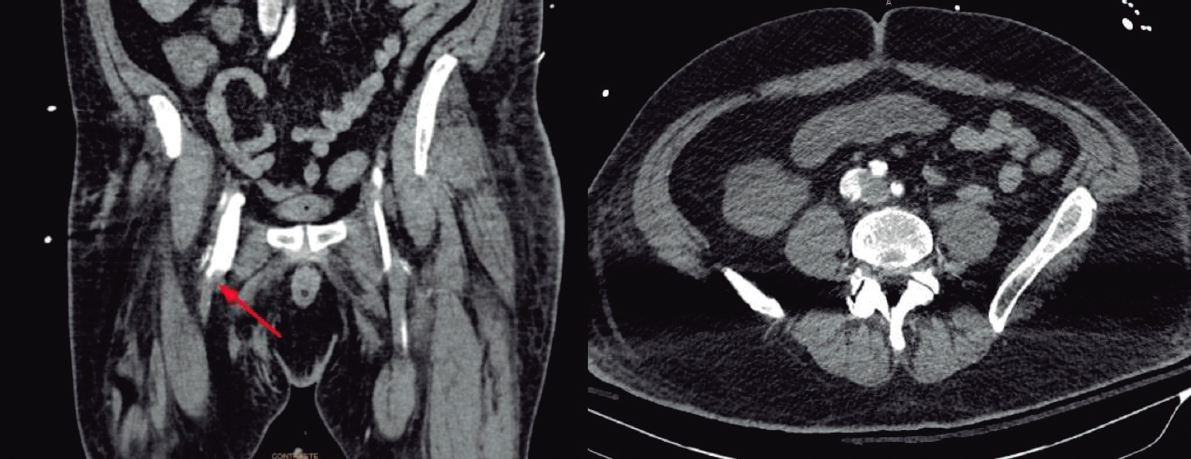
The postoperative period at the critical care unit was torpid. Five days after surgery, the patient broke a fever in the context of ventilator-associated pneumonia. That is why a thoracic computed tomography scan was performed that revealed the presence of a tear—7 mm of maximum diameter—in the left ventricular lateral wall with formation of a large intrapericardial pseudoaneurysm of 8 cm of maximum diameter (figure 1) (video 1 from the supplementary data).
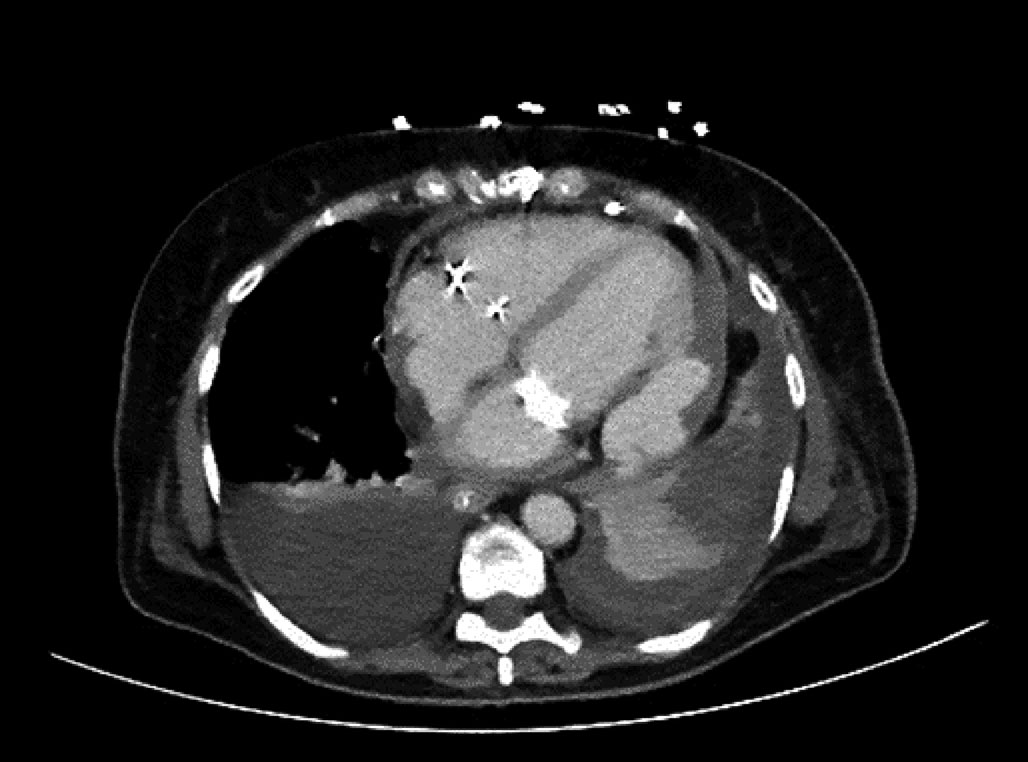
Figure 1. Changes after heart surgery: mitral valve replacement and tricuspid annuloplasty. Tear of 7 mm of maximum diameter in the left ventricular lateral wall with formation of a large cavity/intrapericardial pseudoaneurysm (asterisk) of 8 cm of maximum diameter associated with hemopericardium.
The cardiac computed tomography confirmed the existence of a large defect with a maximum diameter of 7.46 cm, and a minimum diameter of 3.89 cm (figure 2). The entry orifice of the defect—of almost circular morphology—had a maximum diameter of 7.45 mm and a minimum diameter of 6.8 mm (figure 3). The defect was found in the left ventricular lateral wall underneath the mitral valvular projection (video 2 from the supplementary data).
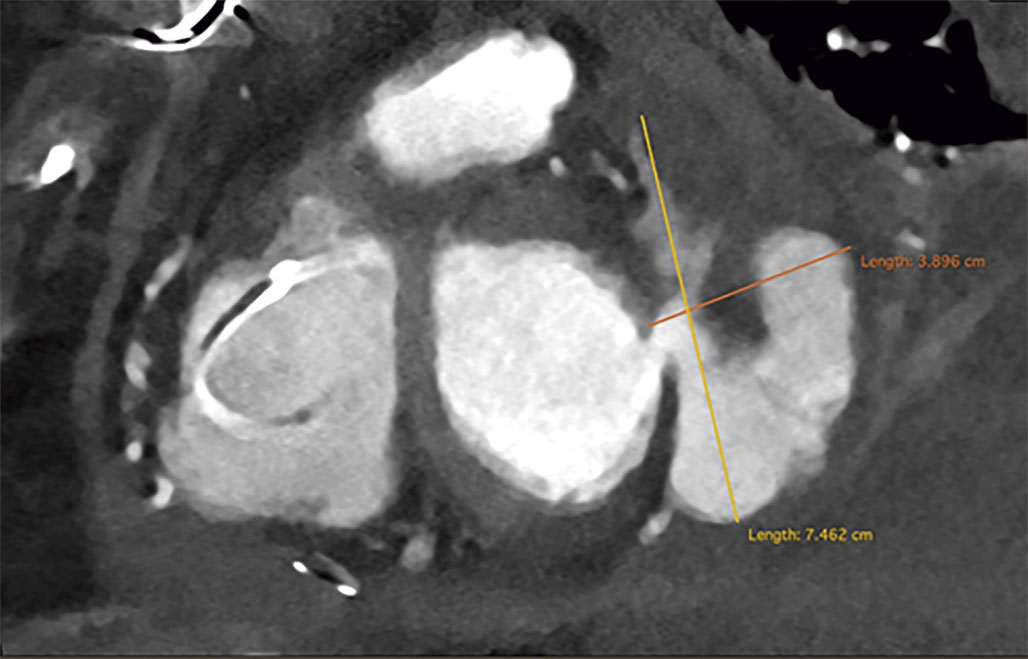
Figure 2. Cardiac computed tomography. Details of the defect. Maximum (yellow) and minimum (orange) diameters of the pseudoaneurysm.

Figure 3. Cardiac computed tomography. Detail of the entry orifice of the defect and its diameter.
The patient’s written and verbal informed consents were obtained before publishing this case report.
FUNDING
None whatsoever.
AUTHORS’ CONTRIBUTIONS
L. Gutiérrez Alonso drafted the manuscript and was directly involved in patient care. D. Arzamendi, X. Millán, L. Asmarats, and M. Torres were directly involved in patient care. D. Arzamendi supervised the draft of the manuscript. Chi Hion Li was directly involved in the case and provided the images.
CONFLICTS OF INTEREST
None whatsoever.
SUPPLEMENTARY DATA
Vídeo 1. Gutiérrez Alonso L. DOI: 10.24875/RECICE.M22000284
Vídeo 2. Gutiérrez Alonso L. DOI: 10.24875/RECICE.M22000284
* Corresponding author:
E-mail address: lolagutialonso@gmail.com (L. Gutiérrez Alonso).