ABSTRACT
Introduction and objectives: In patients with ST-segment elevation myocardial infarction (STEMI) treatment delay significantly affects outcomes. The effect of admission time in STEMI patients is unknown when percutaneous coronary intervention (PCI) is the preferred reperfusion strategy. This study aimed to determine the association between STEMI outcomes and the timing of admission in a PCI center in south-western Europe.
Methods: This retrospective cohort study analyzed the local electronic data from 1222 consecutive STEMI patients treated with PCI. On-hours were defined as admission from Monday to Friday between 8:00 AM and 6:00 PM on non-national holidays.
Results: A total of 439 patients (36%) were admitted on-hours and 783 patients (64%) were admitted off-hours. Baseline characteristics were well-balanced between the 2 groups, including the percentage of patients admitted in cardiogenic shock (on-hours 5% vs off-hours 4%; P = .62). The median time from first medical contact to reperfusion did not differ between the 2 groups (on-hours 120 minutes vs off-hours 123 minutes, P = .54) and no association was observed between admission time and in-hospital mortality (on-hours 5% vs off-hours 5%, P = .90) or 1-year mortality (on-hours 10% vs off-hours 10%, P = .97). Survival analysis showed no differences in on-hours PCI vs off-hours PCI (HR, 1.1; 95%CI, 0.74-1.64; P = .64).
Conclusions: In a contemporary emergency network, the timing of STEMI patients’ admission to the PCI center was not associated with reperfusion delays or increased mortality.
Keywords: ST-segment elevation myocardial infarction. Admisison time. Percutaneous coronary intervention. Emergency medical services. Mortality.
RESUMEN
Introducción y objetivos: En pacientes con infarto agudo de miocardio con elevación del segmento ST (IAMCEST), el retraso en el tratamiento afecta de manera importante los resultados. El efecto del horario de atención en los pacientes con IAMCEST es dudoso cuando la intervención coronaria percutánea (ICP) es la estrategia de reperfusión preferida. Este estudio tuvo como objetivo determinar la asociación entre los resultados del IAMCEST y el momento de la admisión en un centro con ICP del suroeste de Europa.
Métodos: Estudio de cohorte retrospectivo en el que se analizaron los datos electrónicos locales de 1.222 pacientes consecutivos con IAMCEST tratados con ICP. El horario de atención laboral se definió como la admisión de lunes a viernes de 8 a 18 horas, en días no festivos.
Resultados: Un total de 439 pacientes (36%) ingresaron en horario laboral y 783 (64%) se admitieron fuera del horario. Las características iniciales estaban bien equilibradas entre los grupos, incluyendo el porcentaje de pacientes ingresados en shock cardiogénico (en horario laboral el 5% y fuera del horario laboral el 4%; p = 0,62). La mediana de tiempo desde el primer contacto médico hasta la reperfusión no fue diferente entre los 2 grupos (dentro del horario laboral 120 min y fuera del horario laboral 123 min; p = 0,54). No se observó asociación entre el tiempo de admisión y la mortalidad hospitalaria (dentro del horario laboral el 5% y fuera del horario laboral el 5%; p = 0,90) ni la mortalidad a 1 año (en horario laboral el 10% y fuera del horario el 10%; p = 0,97). El análisis de supervivencia no mostró diferencias entre la admisión dentro del horario laboral y la admisión fuera del horario laboral (HR = 1,1; IC95%, 0,74-1,64; p = 0,64).
Conclusiones: En una red de código infarto contemporáneo, el horario de admisión de pacientes con IAMCEST no se asoció con retrasos en la reperfusión ni con un aumento de la mortalidad.
Palabras clave: Infarto agudo de miocardio con elevación del segmento ST. Horario de ingreso. Intervención coronaria percutánea. Emergencia médica. Mortalidad.
Abbreviations PCI: percutaneous coronary intervention. STEMI: ST-segment elevation myocardial infarction.
INTRODUCTION
Ischemic heart disease is the leading cause of death worldwide. In Europe, despite the decline in incidence and mortality between 1990 and 2009, these trends have slowed in recent years. Moreover, Mediterranean countries showed lower rate of decline during this period.1
ST-segment elevation myocardial infarction (STEMI) is a particularly important presentation, associated with high mortality in young individuals.2,3 Primary percutaneous coronary intervention (PCI) is recommended as the first-line therapy to lower mortality and morbidity in STEMI patients.4-6 The timing of treatment is crucial for positive outcomes, and minimization of the time from symptom onset to revascularization is essencial.7,8 While several factors affect treatment timing, emergency system delays play a crucial role as they can be more easily altered by organizational measures and are often used as a quality measurement in STEMI networks.4,9-13
To ensure timely treatment, primary PCI centers included in STEMI networks are recommended to have a 24/7 service.4 However, the impact of admission time (on- vs off-hours) on treatment delay and patient outcomes remains a matter of debate. Some studies and a large meta-analysis have shown that off-hours admission is associated with worse outcomes, partially explained by longer system delays, less guideline-directed management, and less revascularization.14-16 Conversely, studies in high-volume PCI centers integrated in STEMI networks, demonstrated no differences in outcomes according to admission time.17-20 Overall, these results are heterogeneous and include populations from different health care systems.
In Europe, efforts have been made to improve STEMI care through public awareness, emergency medical system operations, and the implementation of a full national coverage 24/7 PCI network.21
The aim of this study was to determine the association between timing of admission in a PCI center and STEMI patients’ outcomes, within a STEMI network in south-western Europe.
METHODS
Study design and population
This retrospective observational cohort study identified 1369 consecutive patients treated with primary PCI at the catheterization laboratory of the Hospital de Braga (Portugal) between June 2011 and May 2016, through the local database that systematically includes all patients undergoing invasive coronary procedures. After an initial analysis, 115 patients were found to have evolved STEMI (> 12 hours since symptom onset) and were therefore excluded. To avoid duplication of results, we excluded 12 records of a repeat episode of STEMI in a patient previously identified in the selected time frame. Lastly, clinical follow-up data were not available for 20 patients, resulting in a final sample of 1222 patients (figure 1). These patients were divided into 2 groups according to admission time (on-hours and off-hours admission), and the main outcome measures evaluated were time delays, in-hospital mortality, and 1-year mortality.
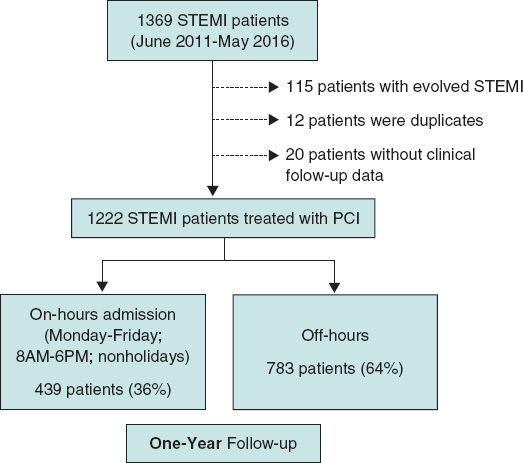
Figure 1. Study flow-chart. PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction.
Definitions
STEMI was defined as the presence of symptoms of myocardial ischemia, associated with electrocardiographic criteria for ST-segment elevation.4
Admission time was based on arrival at the catheterization laboratory. On-hours were defined as admission from Monday to Friday between 8:00 AM and 6:00 PM on non-national holidays.
The first medical contact was defined as the first contact with a health service (hospital or primary care clinic). In patients primarily attended by the emergency medical system, the moment when the emergency vehicle carrying a trained physician arrived at the location of the patient was recorded. The reperfusion time was considered as the moment when the angioplasty guidewire crossed the culprit lesion. Time delays from symptom onset to first medical contact (patient-dependent time), from first medical contact to reperfusion (system-dependent time) and from symptom onset to reperfusion (total ischemic time) were characterized.
Patient stratification according to the Killip classification was based on physical examination and the development of heart failure. A Killip class IV classification was assigned to patients in cardiogenic shock.22
STEMI network organization
Hospital de Braga has a 24/7 catheterization laboratory service for primary PCI, performed by senior interventional cardiologists (on-call during off-hours). The hospital is the only primary PCI-capable hospital in the Minho region in the north of Portugal and serves approximately 1.1 million people (figure 2). First medical contact can be made by the emergency medical system or in non-PCI-capable hospitals and clinics, which decide whether to transfer the patient to the PCI-center after consulting the on-call clinical cardiologist. First medical contact can also be made in Hospital de Braga, with rapid triage to primary PCI.
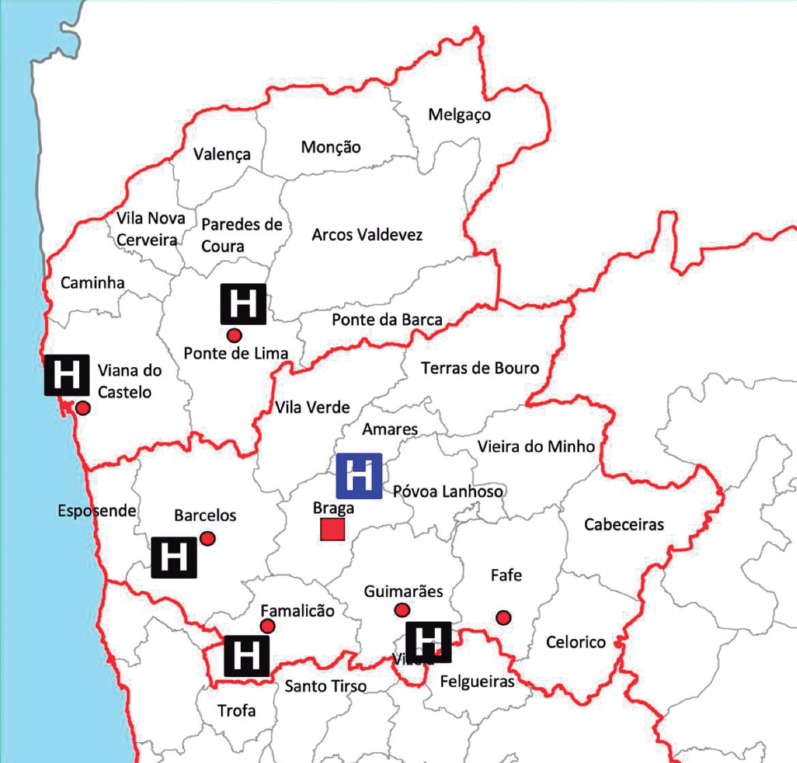
Figure 2. Referral network of the catheterization laboratory of Hospital de Braga.
Data collection and statistical analysis
The data for the present study were obtained from the local database of the patient undergoing PCI, the patient’s clinical record, and the electronic health registry of Portugal. Clinical and demographic variables were collected.
The IBM Statistical Package for the Social Sciences (IBM SPSS) version 28.0 was used for data treatment. The variables studied to characterize the patients were divided into continuous variables and categorical variables. For the analysis of continuous variables, the distribution was first evaluated. If the variables showed symmetrical normal distribution, the results are presented as mean ± standard deviation, while for variables without normal distribution, the results are reported as median [interquartile range]. To compare continuous variables between the 2 groups of patients, parametric tests were applied for variables with normal distribution and nonparametric tests for the remainder. The Student t test for independent samples was used as the parametric test, after evaluation of the homogeneity of variances using the Levene test. The Mann-Whitney U test was the nonparametric test applied. For the description of categorical variables, absolute (No.) and relative (%) frequencies were calculated. The comparison of proportions between the study groups was made using the chi-square test or Fisher exact test when the percentage of cells in the table with an expected frequency less than 5 was greater than 20%. The 1-year survival analysis was performed using the Kaplan-Meier method, comparing the groups using the log-rank test. A multivariate analysis with Cox regression was performed, and was adjusted for confounding variables that were statistically significant in the univariate analysis (age, sex, smoking, diabetes mellitus, hypertension, cardiogenic shock, and total ischemia time), to determine if the timing of patient admission was an independent predictor of 1-year mortality. The adjusted hazard ratio (HR) and 95% confidence interval (95%CI) were analyzed to determine the significance of the predictor. In all analyses, results with probability values of P < .05 were considered statistically significant.
Confidentiality and ethical considerations
Informed consent for the procedure was obtained in all patients. The confidentiality and anonymity of all collected data were ensured during all phases of the study. This study was approved by the local ethics committee and complies with the provisions of the Helsinki Declaration. Informed consent for the present analysis was waived by the ethics committee due to the retrospective nature of the study.
RESULTS
Baseline characteristics
Between June 2011 and May 2016, of 1222 consecutive patients with confirmed STEMI, a total of 439 (36%) were admitted on-hours and 783 (64%) were admitted off-hours. Baseline characteristics were well-balanced between groups, including the percentage of patients admitted in cardiogenic shock (on-hours 5% vs off-hours 4%; P = .62) (table 1).
Table 1. Baseline characteristics
| Total (N = 1222) | On-hours (N = 439) | Off-hours (N = 783) | P | |
|---|---|---|---|---|
| Clinical characteristics | ||||
| Age, y | 61 ± 13 | 62 ± 13 | 61 ± 14 | .40 |
| Female | 269 (22) | 102 (23) | 167 (21) | .44 |
| Smoking (active or previous) | 625 (54) | 218 (51) | 407 (55) | .18 |
| Dyslipidemia | 553 (46) | 201 (46) | 352 (45) | .72 |
| Diabetes | 250 (22) | 104 (25) | 146 (20) | .04 |
| Hypertension | 622 (51) | 224 (52) | 398 (51) | .89 |
| Previous history | ||||
| ACS | 84 (7) | 28 (6) | 56 (7) | .63 |
| PCI | 62 (5) | 43 (4) | 19 (6) | .38 |
| CABG | 11 (1) | 5 (1) | 6 (1) | .50 |
| Presentation | ||||
| Direct admission | 452 (36) | 159 (37) | 293 (37) | .68 |
| Anterior MI | 642 (53) | 229 (52) | 413 (53) | .85 |
| Cardiogenic shock | 51 (4) | 20 (5) | 31 (4) | .62 |
| Angiography | ||||
| Multivessel disease | 583 (48) | 215 (49) | 368 (47) | .51 |
| Echocardiography | ||||
| LVEF | 44 ± 10 | 45 ± 10 | 44 ± 10 | .41 |
ACS, acute coronary syndrome; CABG, coronary artery bypass graft; LVEF, left ventricular ejection fraction; MI, myocardial infarction; PCI, percutaneous coronary intervention. Data are expressed as No. (%) or mean ± standard deviation. | ||||
Comparison of treatment delays
The statistical analysis revealed no significant differences between groups for system-related, patient-related, and total ischemia time (table 2). Similarly, when examining patients directly admitted to the PCI-center, no significant differences were observed in terms of system-related, patient-related, and total ischemia time (table 2).
Table 2. Treatment delays
| Irrespective of place of FMC | Total (N = 1222) | On-hours (N = 439) | Off-hours (N = 783) | P |
|---|---|---|---|---|
| Patient-related SO-FMC, min | 87 [45-165] | 82 [45-160] | 89 [48-166] | .30 |
| Emergency system-related FMC-reperfusion, min | 123 [92-172] | 120 [91-169] | 123 [92-173] | .54 |
| Total ischemic time SO-reperfusion | 225 [164-354] | 220 [159-343] | 228 [165-360] | .39 |
| Admitted directly to the PCI-center | Subtotal (N1 = 452) | On-hours (N1 = 159) | Off-hours (N1 = 293) | P |
| Patient-related SO-FMC, min | 77 [40-150] | 75 [45-155] | 78 [40-150] | .96 |
| Emergency system-related FMC-reperfusion, min | 88 [68-115] | 87 [68-115] | 88 [70-115] | .54 |
| Total ischemic time SO-revascularization, min | 177 [125-265] | 175 [127-254] | 177 [124-267] | .92 |
FMC, first medical contact; PCI, percutaneous coronary intervention; SO, symptom onset. Values are expressed as median [interquartile range]. | ||||
Association between admission time and outcomes
A 1-year follow-up was completed for all patients included in the analysis. There was no association between on- and off-hours admission time and in-hospital (5% vs 5%; P = .90) or 1-year mortality (10% vs 10%; P = .97). Equally, in patients admitted on- and off-hours directly to the PCI center, in-hospital (4% vs 7%; P = .30) and 1-year mortality (9% vs 13%; P = .27) was similar.
Patients who experienced cardiogenic shock had significantly higher rates of both in-hospital (55% vs 3%; P < .01) and 1-year mortality (71% vs 7%; P < .01) compared with stable patients. However, the time of admission to the hospital did not show a significant impact on the in-hospital (on-hours 50% vs off-hours 58%; P = .57) or 1-year mortality (on-hours 65% vs off-hours 74%; P = .48) for those with cardiogenic shock.
Hospital admissions for heart failure did not differ in patients admitted on- and off-hours (3% vs 3%; P = .60).
Kaplan-Meier curves showed no differences between timings in survival terms (log-rank P = .95) (figure 3). The timing of admission was not a predictor of 1-year mortality after adjustment (HR, 1.1; 95%CI, 0.74-1.64; P = .64). Independent predictors of mortality at 1-year are depicted in table 3, with cardiogenic shock emerging as the only strong predictor of 1-year mortality.
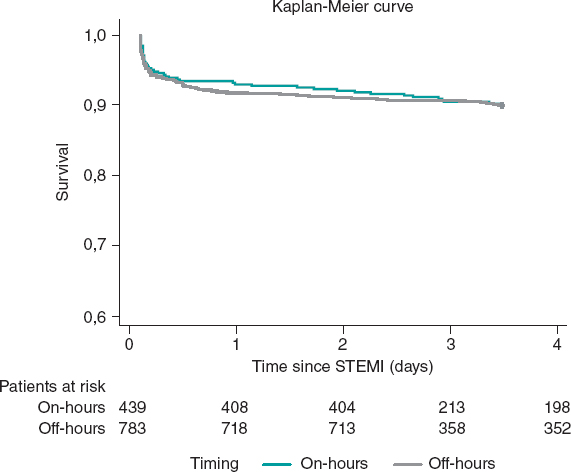
Figure 3. Kaplan-Meier curves for 1-year survival. STEMI, ST-segment elevation myocardial infarction.
Table 3. Predictive factors of 1-year mortality
| Adjusted HR* | 95%CI | P | |
|---|---|---|---|
| Age | 1.08 | 1.06-1.10 | < .01 |
| Cardiogenic shock | 12.64 | 7.60-19.47 | < .01 |
| Diabetes mellitus | 1.49 | 0.98-2.26 | .06 |
| Hypertension | 1.11 | 0.72-1.73 | .63 |
| Sex | 1.29 | 0.78-1.88 | .43 |
| Smoking | 1.06 | 0.65-1.74 | .81 |
| Total ischemic time | 1.00 | 1.00-1.01 | .06 |
95%CI, 95% confidence interval; HR, hazard ratio. * Multivariate analysis with Cox regression adjusted for confounding variables that were statistically significant in the univariate analysis (age, cardiogenic shock, diabetes mellitus, hypertension, sex, smoking, and total ischemia time). Admission time was not associated with 1-year mortality in univariate analysis (P = .95). | |||
DISCUSSION
This study suggests that there is no association between the timing of admission in the PCI center and adverse outcomes, in a structured STEMI network that offers PCI as the standard of care 24/7. Patients admitted off-hours had the same characteristics and were offered the same quality of care as those admitted on-hours, reflected by the similarity in treatment delays. Previous studies, in networks that provided the same quality of care whatever the admission time, reported no differences in outcomes.17-20
On the other hand, studies that report worst outcomes in patients admitted off-hours, mainly reflect differences in care during this period, with increased delay before revascularization, lower delivery of primary PCI, different procedural characteristics, and fewer available staff during off-hours.16,23-25 Additionally, several studies found that patients tended to have worse clinical status on admission during off-hours, which adversely impacted outcomes.16,26 A finding that supports the outmost importance of presentation status is the fact that cardiogenic shock at admission was found to be an independent predictor of 1-year mortality in this study. However, we did not find significant differences in presentation status according to admission time.
This analysis emphasizes that good organization of STEMI networks, with fast-track 24/7 primary PCI, is key to improve patient outcomes and to obviate the adverse impact of off-hours. However, time delays can still be optimized. Public awareness is key to reduce patient-dependent delays, and efforts should be made to improve recognition of symptoms and activation of emergency medical systems. System delays are quality of care indexes, and in this study, they are in the upper margin for benefit of PCI over fibrinolysis (120 minutes).4,27 This group previously analyzed the impact of interhospital transfer in time from first medical contact to reperfusion, and suggested improvements in chest pain work-up in emergency rooms and prompt transfer protocols after STEMI detection.28
Mortality rates in STEMI differ widely among analyses according to the geographical area, time frame analyzed, patient inclusion criteria, and patient management protocols.29,30 Nonetheless, in this analysis, mortality rates (5% in-hospital and 10% 1-year mortality) were in line with those reported in contemporary registries.2,31
To the best of our knowledge, this is the first study in a STEMI network in south-western Europe ensuring the feasibility and safety of on-call off-hours primary PCI in a contemporary STEMI network. This provides substantial reassurance to the usual organization of cath labs with on-call professionals, essential for workload management and organization of the laboratory workforce.
Study limitations
First, this is a single-center study and may not reflect regional differences in STEMI network organization. Moreover, the results of this study reflect those of a high-volume PC center with a long-standing 24/7 primary PCI program, which may differ from others due to diverse organizational features and available resources. This could be tackled by a future study analyzing national registry data.
Second, the retrospective nature of this study has the limitations inherent to this type of design.
Third, the definition of off-hours admission time is heterogeneous across the literature. In this study, it was defined according to the organizational features of the cath lab, which may not reflect off-hours in other centers/networks.
Additionally, overall mortality in this study may be underestimated, as the group of patients diagnosed in hospitals other than the PCI center and who died before or during transfer were not included in this analysis.
Another limitation of this study is the focus on the management of the patient exclusively until the performance of the primary PCI. Other factors that affect outcomes in these patients, most importantly the delivery of guideline directed medical therapies immediately after revascularization, were not analyzed.
Our findings, based on procedures conducted between 2011 and 2016, may not fully reflect the most current health care trends, given the continuous development of clinical guidelines and treatment approaches. For instance, the reduced use of thrombus aspiration, in line with updated guidelines, highlights the imperative for ongoing research to capture the latest developments in the field.
CONCLUSIONS
In a contemporary emergency network, STEMI patients’ admission time in the PCI-center was not associated with reperfusion delays or increased in-hospital and 1-year mortality. Mortality in efficient STEMI networks is primarily affected by the severity of clinical presentation.
FUNDING
None.
ETHICAL CONSIDERATIONS
Informed consent for the procedure was obtained in all cases. The confidentiality and anonymity of all collected data were ensured during all phases of the study. This study was approved by the local ethics committee and complied with the provisions of the Helsinki Declaration. Informed consent for the present analysis was waived by the ethics committee due to the retrospective nature of the study.
Possible sex/gender biases were taken into account and avoided.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCE
The authors did not use artificial intelligence tools during the preparation of this study.
AUTHORS’ CONTRIBUTIONS
All the authors contributed to the study design, performed a critical review of the manuscript, gave their final approval, and are fully responsible for all aspects of the study guaranteeing both its integrity and accuracy.
CONFLICTS OF INTEREST
None.
WHAT IS KNOWN ABOUT THE TOPIC?
- The impact of admission time (on- vs off-hours) on treatment delay and patient outcomes remains a matter of debate. Some studies have shown that off-hours admission is associated with worse outcomes, while others disprove these findings.
- Previous analyses are heterogeneous and include populations from different health care systems.
WHAT DOES THIS STUDY ADD?
- Real-world clinical evidence that STEMI patients’ admission time to the PCI-center is not associated with reperfusion delays or increased in-hospital and 1-year mortality.
- Mortality in a STEMI network is primarily affected by the severity of clinical presentation.
REFERENCES
1. Vancheri F, Tate AR, Henein M, et al. Time trends in ischaemic heart disease incidence and mortality over three decades (1990–2019) in 20 Western European countries:systematic analysis of the Global Burden of Disease Study 2019. Eur J Prev Cardiol. 2022;29:396-403.
2. Zeymer U, Ludman P, Danchin N, et al. Reperfusion therapies and in-hospital outcomes for ST-elevation myocardial infarction in Europe:the ACVC-EAPCI EORP STEMI Registry of the European Society of Cardiology. Eur Heart J. 2021;42:4536-4549.
3. Fokkema ML, James SK, Albertsson P, et al. Population Trends in Percutaneous Coronary Intervention:20-Year Results From the SCAAR (Swedish Coronary Angiography and Angioplasty Registry). J Am Coll Cardiol. 2013;61:1222-1230.
4. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2018;39:119-177.
5. Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction:A quantitative review of 23 randomised trials. Lancet. 2003;361:13-20.
6. Nielsen PH, Maeng M, Busk M, et al. Primary angioplasty versus fibrinolysis in acute myocardial infarction:Long-term follow-up in the danish acute myocardial infarction 2 trial. Circulation. 2010;121:1484-1491.
7. Cannon CP, Gibson CM, Lambrew CT, et al. Relationship of Symptom-Onset-to-Balloon Time and Door-to-Balloon Time With Mortality in Patients Undergoing Angioplasty for Acute Myocardial Infarction. JAMA. 2000;283:2941-2947.
8. Koul S, Andell P, Martinsson A, et al. Delay from first medical contact to primary PCI and all-cause mortality:a nationwide study of patients with ST-elevation myocardial infarction. J Am Heart Assoc. 2014;3:e000486.
9. Terkelsen CJ, Sørensen JT, Maeng M, et al. System Delay and Mortality Among Patients With STEMI Treated With Primary Percutaneous Coronary Intervention. JAMA. 2010;304:763-771.
10. Peterson MC, Syndergaard T, Bowler J, Doxey R. A systematic review of factors predicting door to balloon time in ST-segment elevation myocardial infarction treated with percutaneous intervention. Int J Cardiol. 2012;157:8-23.
11. Pereira H, CaléR, Pinto FJ, et al. Factors influencing patient delay before primary percutaneous coronary intervention in ST-segment elevation myocardial infarction:The Stent for life initiative in Portugal. Rev Port Cardiol. 2018;37:409-421.
12. Pereira H, CaléR, Pereira E, et al. Five years of Stent for Life in Portugal. Rev Port Cardiol. 2021;40:81-90.
13. Wein B, Bashkireva A, Au-Yeung A, et al. Systematic investment in the delivery of guideline-coherent therapy reduces mortality and overall costs in patients with ST-elevation myocardial infarction:Results from the Stent for Life economic model for Romania, Portugal, Basque Country and Kemerovo region. Eur Heart J Acute Cardiovasc Care. 2020;9:902-910.
14. Kostis WJ, Demissie K, Marcella SW, Shao YH, Wilson AC, Moreyra AE. Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med. 2007;356:1099-1109.
15. Magid DJ, Wang Y, Herrin J, et al. Relationship Between Time of Day, Day of Week, Timeliness of Reperfusion, and In-Hospital Mortality for Patients With Acute ST-Segment Elevation Myocardial Infarction. JAMA. 2005;294:803-812.
16. Sorita A, Ahmed A, Starr SR, et al. Off-hour presentation and outcomes in patients with acute myocardial infarction:systematic review and meta-analysis. BMJ. 2014;348:f7393.
17. de Boer SPM, Oemrawsingh RM, Lenzen MJ, et al. Primary PCI during off-hours is not related to increased mortality. Eur Heart J Acute Cardiovasc Care. 2012;1:33-39.
18. Rathod KS, Jones DA, Gallagher SM, et al. Out-of-hours primary percutaneous coronary intervention for ST-elevation myocardial infarction is not associated with excess mortality:a study of 3347 patients treated in an integrated cardiac network. BMJ Open. 2013;3:e003063.
19. Lattuca B, Kerneis M, Saib A, et al. On- Versus Off-Hours Presentation and Mortality of ST-Segment Elevation Myocardial Infarction Patients Treated With Primary Percutaneous Coronary Intervention. Cardiovascular Interventions. 2019;12:2260-2268.
20. Casella G, Ottani F, Ortolani P, et al. Off-hour primary percutaneous coronary angioplasty does not affect outcome of patients with ST-segment elevation acute myocardial infarction treated within a regional network for reperfusion:The REAL (Registro Regionale Angioplastiche dell'Emilia-Romagna) registry. JACC Cardiovasc Interv. 2011;4:270-278.
21. Wein B, Bashkireva A, Au-Yeung A, et al. Systematic investment in the delivery of guideline-coherent therapy reduces mortality and overall costs in patients with ST-elevation myocardial infarction:Results from the Stent for Life economic model for Romania, Portugal, Basque Country and Kemerovo region. Eur Heart J Acute Cardiovasc Care. 2020;9:902-910.
22. Killip T, Kimball JT. Treatment of myocardial infarction in a coronary care unit:A Two year experience with 250 patients. Am J Cardiol. 1967;20:457-464.
23. Magid DJ, Wang Y, Herrin J, et al. Relationship Between Time of Day, Day of Week, Timeliness of Reperfusion, and In-Hospital Mortality for Patients With Acute ST-Segment Elevation Myocardial Infarction. JAMA. 2005;294:803-812.
24. Barnett Pathak E, Strom JA. Disparities in Use of Same-Day Percutaneous Coronary Intervention for Patients With ST-Elevation Myocardial Infarction in Florida, 2001–2005. Am J Cardiol. 2008;102:802-808.
25. Cavallazzi R, Marik PE, Hirani A, Pachinburavan M, Vasu TS, Leiby BE. Association Between Time of Admission to the ICU and Mortality:A Systematic Review and Metaanalysis. Chest. 2010;138:68-75.
26. Glaser R, Naidu SS, Selzer F, et al. Factors Associated With Poorer Prognosis for Patients Undergoing Primary Percutaneous Coronary Intervention During Off-Hours. Biology or Systems Failure?JACC Cardiovasc Interv. 2008;1:681-688.
27. Pinto DS, Frederick PD, Chakrabarti AK, et al. Benefit of transferring ST-segment-elevation myocardial infarction patients for percutaneous coronary intervention compared with administration of onsite fibrinolytic declines as delays increase. Circulation. 2011;124:2512-2521.
28. Ferreira AS, Costa J, Braga CG, Marques J. Impacto na mortalidade da admissão direta versus transferência inter?hospitalar nos doentes com enfarte agudo do miocárdio com elevação do segmento ST submetidos a intervenção coronária percutânea primária. Rev Port Cardiol. 2019;38:621-631.
29. Williams C, Fordyce CB, Cairns JA, et al. Temporal Trends in Reperfusion Delivery and Clinical Outcomes Following Implementation of a Regional STEMI Protocol:A 12-Year Perspective. CJC Open. 2023;5:181-190.
30. Landon BE, Hatfield LA, Bakx P, et al. Differences in Treatment Patterns and Outcomes of Acute Myocardial Infarction for Low- and High-Income Patients in 6 Countries. JAMA. 2023;329:1088-1097.
31. Szummer K, Wallentin L, Lindhagen L, et al. Improved outcomes in patients with ST-elevation myocardial infarction during the last 20?years are related to implementation of evidence-based treatments:experiences from the SWEDEHEART registry 1995–2014. Eur Heart J. 2017;38:3056-3065.