ABSTRACT
Introduction and objectives: During the lockdown due to the pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a decrease in the number of admissions due to acute coronary syndrome (ACS) was observed. The objective of our study was to evaluate the impact lockdown had on the incidence, morbidity and mortality, and management of ACS.
Methods: A retrospective and multicenter study was conducted including patients admitted due to ACS from February 14 through June 24, 2020. Patients with acute myocardial infarction and coronary arteries without significant lesions were excluded. The following groups were established based on the period of admission: a) 1 month before lockdown; b) during lockdown; and c) 1 month after lockdown. The differences in mortality seen among the 3 groups were evaluated, as well as the temporal differences reported between symptom onset and the first medical contact (FMC).
Results: a total of 634 patients were included (group a, 205; group b, 303, and group c, 126). A 41% decrease in the number of admissions due to ACS was observed during the first month of lockdown compared to the previous month, as well as diagnostic delay during this same period (group a, 66 minutes (45-180), group b, 120 minutes (60-240), and group c, 120 minutes (60-240), P = .007). However, a higher mortality rate during confinement was not reported (RR, 1.26; 95%CI, 0.53-2.97; P = .60).
Conclusions: During lockdown, a remarkable decrease in the number of admissions due to ACS was observed, and although there was an increase in the time elapsed from symptom onset to the FCM in this period in patients with STEMI, the mortality rate was similar in the 3 groups studied.
Keywords: COVID-19. SARS-CoV-2. Acute coronary syndrome. Pandemic. Revascularization. Lockdown.
RESUMEN
Introducción y objetivos: Durante el confinamiento por la pandemia provocada por el coronavirus del síndrome respiratorio agudo grave de tipo 2 (SARS-CoV-2) se observó un descenso en los ingresos por síndrome coronario agudo (SCA). El objetivo de este estudio fue evaluar el impacto del confinamiento en la incidencia, la morbimortalidad y el tratamiento del SCA.
Métodos: Estudio retrospectivo y multicéntrico, en el que se incluyeron los pacientes ingresados por SCA entre el 14 de febrero y el 24 de junio de 2020. Se excluyeron los pacientes con infarto agudo de miocardio y coronarias sin lesiones significativas. Se establecieron 3 grupos en función del periodo de ingreso: a) 1 mes antes del confinamiento; b) durante el confinamiento; y c) 1 mes después del confinamiento. Se evaluaron las diferencias en la mortalidad entre los 3 grupos, así como las diferencias temporales entre el inicio de los síntomas y el primer contacto médico.
Resultados: Se incluyeron 634 pacientes (grupo A: 205; grupo B: 303; grupo C: 126). Se observó un descenso del 41% en los ingresos por SCA durante el primer mes del confinamiento respecto al mes previo, así como un retraso en el diagnóstico durante este mismo periodo: grupo A, 66 minutos (45-180); grupo B, 120 minutos (60-240); grupo C, 120 minutos (60-240) (p = 0,007). Sin embargo, no hubo mayor mortalidad durante el confinamiento (riesgo relativo, 1.26; intervalo de confianza del 95%, 0.53-2.97; p = 0,60).
Conclusiones: Durante el confinamiento se produjo un marcado descenso en los ingresos por SCA y, a pesar de que se dilató el tiempo desde el inicio de los síntomas hasta el primer contacto médico en este periodo en los pacientes con SCA con elevación del segmento ST, la mortalidad fue similar en los 3 grupos estudiados.
Palabras clave: COVID-19. SARS-CoV-2. Síndrome coronario agudo. Pandemia. Revascularización. Confinamiento.
Abbreviations ACS: acute coronary syndrome. SARS-CoV-2: severe acute respiratory syndrome coronavirus 2. STEMI: ST-segment elevation myocardial infarction.
INTRODUCTION
By the end of December 2019, The People’s Republic of China reported the World Health Organization on the first cases detected of an unknown pneumonia caused by a new type of coronavirus in the City of Wuhan, China.1,2 Since then, the disease caused by this virus has spread rapidly bringing the healthcare systems of several countries to the point of collapse ultimately triggering dramatic preventive measures by the health authorities.
The pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has had a tremendous social, economic, and health impact across the world. Again and again, the healthcare setting has sustained several organizational and care changes that have triggered significant variations in the management therapeutic approach of the remaining diseases.3-5 Some studies have reported a lower number of admissions due to cardiovascular diseases, which has had a significant impact on morbidity and mortality alike.6-8
Pressure to the healthcare system due to COVID-19, the lockdown, and the lower demand for assistance are some of the reasons that may account for these changes. The objective of this study is to assess the rate of acute coronary syndrome (ACS) across the different stages of the pandemic in Spain, as well as the impact it has had on morbidity, mortality, and therapeutic management.
METHODS
Retrospective, observational, and multicenter study including data from patients admitted to 4 tertiary care centers of our country from 3 autonomous communities due to ACS from February 14, 2020 through June 24, 2020. Patients with ST-segment elevation acute coronary syndrome (STEACS), and non-ST-segment elevation acute coronary syndrome and were included. Patients with acute myocardial infarction and without significant lesions in coronary arteries were excluded. Patients were categorized into 3 groups based on the length of hospital stay: group A, from February 14 through March 14, 2020 (1 month before the lockdown); group B, from March 15 through May 24, 2020 (during the lockdown), and group C, from May 25 through June 24, 2020 (1 month after the stay-at-home lockdown). The patients’ baseline characteristics, acute complications, and cardiovascular events reported at the follow-up like all-cause mortality, cardiac death, stroke, reinfarction, stent thrombosis, and need for rehospitalization were recorded. In patients with STEACS the times elapsed between symptom onset and the first medical contact (FMC), and between electrocardiographic diagnosis until reperfusion were recorded. Clinical follow-up was completed back in July 25, 2020. Data curation was approved by the local ethics committee of each participant center.
The study primary endpoint was to assess the differences reported in all-cause mortality after 30 days since the onset of the acute coronary event among the 3 study groups. The study secondary endpoint was to analyze the differences reported in a composite of cardiac death, stroke, admission due to new ACS, stent thrombosis, and need for new revascularization. Complications reported after infarction at the follow-up, a high left ventricular ejection fraction, and revascularization times (from symptom onset until the first medical contact, and from diagnosis until reperfusion) were also studied in a secondary analysis and compared among the 3 groups.
Statistical analysis
Categorical variables were expressed as number and percentage using brackets and compared using the chi-square test or Fisher’s exact test, when appropriate. Continuous variables were expressed as mean and standard deviation or median and interquartile range in cases without a normal distribution. The Shapiro-Wilk test was used to assess the normal distribution of continuous variables that were compared using the analysis of variance (ANOVA) for independent samples or Kruskall-Wallis H test based on their normal distribution looking for differences among the 3 groups. Survival was studied using the Kaplan-Meier curves, and differences were assessed using the log-rank test. Cox proportional hazards regression analysis was used to assess the impact of group B (lockdown period) in the overall mortality of the patients. All estimates were performed using the statistical software package STATA version 15.1. P values < .05 were considered statistically significant.
RESULTS
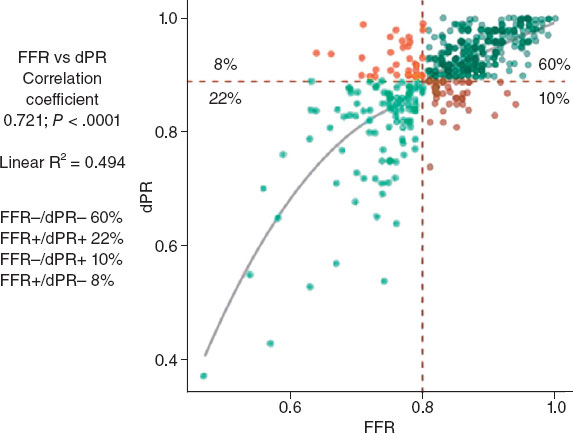
A total of 634 patients were included from February 14, 2020 through June 24, 2020. Of these, 205 were patients from group A, 303 from group B, and 126 from group C with a median follow-up of 98 days (63-137 days). The number of admissions due to ACS was 120, 138, and 151 within the first, second, and third months since the state of alarm declared. This lowered the rate of admissions due to ACS by 41%, 33%, and 26%, respectively compared to the rates reported 1 month before the lockdown for the same 30-day period (figure 1).
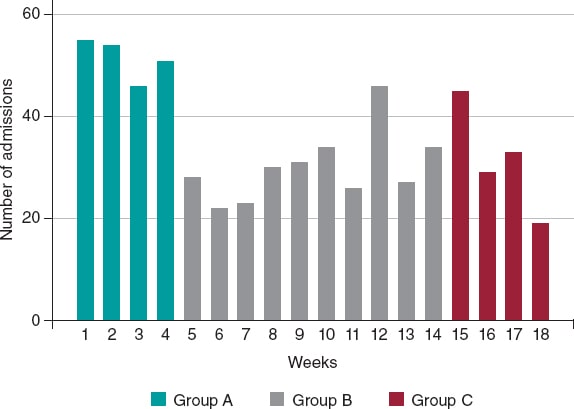
Figure 1. Absolute number of patients admitted due to acute coronary syndrome, expressed in weeks and categorized into group A, B, and C.
A total of 356 (56.2%) from the overall number of patients were admitted due to STEACS, and 278 (43.8%) due to non-ST-segment elevation acute coronary syndrome. The cohort baseline characteristics are shown on table 1. Patients admitted during the lockdown (group B) were younger (P = .012) and had lower levels of hypertension and dyslipidemia. On the other hand, these patients’ past medical history showed less ischemic heart disease, and coronary revascularization (P < .001).
Table 1. Baseline characteristics, diagnosis at admission, and treatment
| Variable | Total (N = 634) | Group A (N = 205) | Group B (N = 303) | Group C (N = 126) | P |
|---|---|---|---|---|---|
| Age | 66.3 ±12.6 | 67.4 ±11.6 | 64.8 ±12.7 | 68.2 ±13.6 | .012 |
| Sex, male | 494 (77.9) | 158 (77.1) | 241 (79.5) | 95 (75.4) | .603 |
| AHT | 400 (63.1) | 143 (69.8) | 176 (58.1) | 81 (64.3) | .027 |
| DM | 191 (30.1) | 71 (35.1) | 89 (29.4) | 30 (23.8) | .086 |
| DL | 368 (58.0) | 137 (66.8) | 164 (54.1) | 67 (53.2) | .008 |
| Smoking | 364 (57.4) | 124 (60.5) | 182 (60.1) | 58 (46.0) | .015 |
| PVD | 36 (5.7) | 15 (7.3) | 16 (5.3) | 5 (4.0) | .405 |
| Stroke | 37 (5.8) | 11 (5.4) | 16 (5.3) | 110 (7.9) | .531 |
| CKD (GF < 60) | 30 (4.7) | 18 (8.8) | 7 (2.3) | 5 (4.0) | .003 |
| COPD | 45 (7.1) | 14 (6.8) | 22 (7.3) | 9 (7.1) | .981 |
| AF | 40 (6.3) | 16 (7.8) | 16 (5.3) | 8 (6.4) | .517 |
| IHD | 150 (23.7) | 79 (38.5) | 46 (15.2) | 25 (19.8) | < .001 |
| AMI | 103 (16.3) | 52 (25.4) | 31 (10.2) | 20 (15.9) | < .001 |
| PCI | 117 (18.5) | 60 (29.3) | 36 (11.9) | 21 (16.7) | < .001 |
| CABG | 23 (3.6) | 12 (5.9) | 7 (2.3) | 4 (3.2) | .112 |
| Diagnoses | |||||
| UA | 83 (13.1) | 36 (17.6) | 27 (8.9) | 20 (15.9) | .003 |
| NSTEMI | 195 (30.8) | 67 (32.7) | 83 (27.4) | 45 (35.7) | .003 |
| STEACS | 356 (56.2) | 102 (49.8) | 193 (63.7) | 61 (48.4) | .003 |
| GRACE | 120.1 ±35.6 | 118.4 ±35.4 | 119.1 ±34.6 | 124.8 ±38.3 | .264 |
| CRUSADE | 31.4 ±13.8 | 34.1 ±15.2 | 30.4 ±13.3 | 29.7 ±11.8 | .001 |
| Cardiac catheterization | 616 (97.5) | 198 (96.6) | 295 (97.7) | 123 (98.4) | .565 |
| Emergency | 375 (59.5) | 112 (54.9) | 190 (63.1) | 73 (58.4) | .447 |
| Deferred | 242 (38.4) | 87 (42.7) | 105 (34.9) | 50 (40.0) | .447 |
| Fibrinolysis | 29 (5.1) | 10 (5.7) | 13 (4.5) | 6 (6.1) | .652 |
| PCI | 534 (94.3) | 165 (93.2) | 276 (95.2) | 93 (94.0) | .652 |
| CABG | 29 (4.6) | 11 (5.4) | 8 (2.7) | 10 (8.1) | .045 |
| LMCA or 3-vessel disease | 136 (21.5) | 52 (25.4) | 55 (18.6) | 29 (23.0) | .135 |
| CABG (LMCA or 3-vessels) | 22 (16.3) | 9 (17.7) | 3 (5.5) | 10 (34.5) | .003 |
| Conservative treatment | 3 (0.5) | 2 (1.1) | 1 (0.3) | 0 (0) | .652 |
| Complete revascularization | 456 (75.6) | 138 (74.6) | 223 (76.1) | 95 (76.0) | .926 |
| LVEF at discharge | 49.2 ±11.1 | 49.7 ±11.6 | 48.6 ±11.2 | 49.9 ±10.0 | .421 |
AF, atrial fibrillation; AHT, arterial hypertension; AMI, acute myocardial infarction; CABG, coronary artery bypass graft; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; DL, dyslipidemia; DM, diabetes mellitus; GF, glomerular filtration; HT, arterial hypertension; IHD, ischemic heart disease; LMCA, left main coronary artery; LVEF, left ventricular ejection fraction; NSTEMI, non-ST-segment elevation myocardial infarction; PCI, percutaneous coronary intervention; PVD, peripheral vascular disease; STEACS, ST-segment elevation acute coronary syndrome; UA, unstable angina. Data are expressed as no. (%) or mean ± standard deviation. | |||||
A diagnostic coronary angiography was performed on 97.1% of the cohort without any differences being reported regarding percutaneous coronary intervention throughout the different periods studied (P = .652); however, a significant reduction in the number of surgical coronary revascularizations performed during the lockdown was reported (group A, 5.4%; group B, 2.7%; group C, 8.1%; P = .045) including the subgroup of patients with left main coronary artery disease or 3-vessel disease (P = .003) (table 1).
A total of 36 deaths were reported, 22 of which were due to cardiovascular causes. No statistically significant differences were reported in the all-cause mortality rate after 30 days among the 3 groups (P = .327). According to a Cox regression analysis, being in the lockdown group (group B) was not associated with a higher all-cause mortality rate (P = .60). No survival differences were reported either among the 3 groups (figure 2).
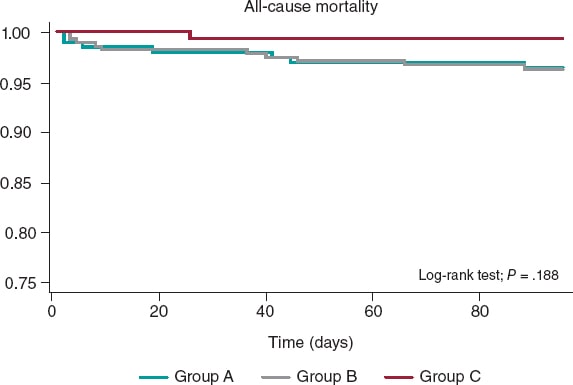
Figure 2. Kaplan-Meier survival curves for all-cause mortality in groups A (February 14-March 14), B (March 15-May 24), and C (May 25-June 24).
No significant differences were reported at the follow-up in a composite of cardiac death, stroke, readmission due to new ACS, stent thrombosis, and new revascularization (P = .120). The remaining clinical events at the follow-up are shown on table 2 and the in-hospital events on table 3.
Table 2. Clinical events at the follow-up
| Variable | Total (N = 634) | Group A (N = 205) | Group B (N = 303) | Group C (N = 126) | P |
|---|---|---|---|---|---|
| All-cause mortality | 36 (5.7) | 15 (7.3) | 13 (4.3) | 8 (6.4) | .327 |
| Cardiac death | 22 (64.7) | 7 (50) | 9 (75) | 6 (75) | .427 |
| Stroke | 20 (3.2) | 9 (4.4) | 8 (2.6) | 3 (2.4) | .551 |
| Re-AMI | 4 (0.7) | 1 (0.5) | 2 (0.7) | 1 (0.8) | 1.000 |
| Stent thrombosis | 12 (2.0) | 8 (4.1) | 1 (0.3) | 3 (2.4) | .006 |
| New revascularization | 6 (1.0) | 4 (2.0) | 2 (0.7) | 0 (0) | .259 |
| CV death + stroke + Re-AMI + stent thrombosis + new revascularization | 57 (9.0) | 24 (11.7) | 20 (6.6) | 13 (10.3) | .120 |
CV, cardiovascular; Re-AMI, new acute myocardial infarction. Data are expressed as no. (%). | |||||
Table 3. In-hospital events
| Variable | Total (N = 634) | Group A (N = 205) | Group B (N = 303) | Group C (N = 126) | P |
|---|---|---|---|---|---|
| Inotropic agents | 53 (8.5) | 17 (8.4) | 27 (9.0) | 9 (7.2) | .836 |
| PM at admission | 12 (1.9) | 4 (2.0) | 8 (2.7) | 0 (0) | .188 |
| IABP | 11 (1.7) | 7 (3.4) | 4 (1.3) | 0 (0) | .048 |
| OTI | 41 (6.5) | 15 (7.3) | 21 (7.0) | 5 (4.0) | .444 |
| NIMV | 18 (2.9) | 6 (2.9) | 7 (2.3) | 5 (4.0) | .604 |
| RRT | 10 (1.6) | 6 (3) | 3 (1.0) | 1 (0.8) | .192 |
| AVB | 20 (3.2) | 7 (3.4) | 12 (4.0) | 1 (0.8) | .227 |
| SMVT | 18 (2.9) | 6 (2.9) | 9 (3.0) | 3 (2.4) | 1.000 |
| VF | 29 (4.6) | 12 (5.9) | 12 (4.0) | 5 (4.0) | .582 |
| AF at admission | 42 (6.7) | 11 (5.4) | 23 (7.6) | 8 (6.4) | .597 |
| BARC bleeding type > 3 | 16 (2.5) | 2 (1.0) | 9 (3.0) | 5 (4.0) | .161 |
| Infection | 57 (9.0) | 12 (6.0) | 28 (10.1) | 17 (11.0) | .184 |
| ARDS | 12 (1.9) | 1 (0.5) | 7 (2.5) | 4 (2.6) | .208 |
| Mechanical complications | 10 (1.6) | 3 (1.5) | 6 (2.0) | 1 (0.8) | .774 |
| Killip III or IV | 62 (9.8) | 20 (9.8) | 31 (10.3) | 11 (8.8) | .898 |
AF, atrial fibrillation; ARDS, acute respiratory distress syndrome; AVB, atrioventricular block; BARC, Bleeding Academic Research Consortium; IABP, intra-aortic balloon pump; NIMV, non-invasive mechanical ventilation; OTI, orotracheal intubation; PM, pacemaker; RRT, renal replacement therapy; SMVT, sustained monomorphic ventricular tachycardia; VF, ventricular fibrillation. Data are expressed as no. (%). | |||||
Regarding delay times, significant differences were reported among the different groups with longer times elapsed between symptom onset and the first medical contact during (group B) and after lockdown (group C) compared to the previous period (group A): group A, 66 min (45-180), group B, 120 min (60-240), group C, 120 min (60-240); P = .007). The time elapsed between symptom onset until the first medical contact was similar in groups B and C (P = .7102). Finally, the time elapsed between diagnosis and reperfusion was shorter in patients from group C (P = .025) compared to the remaining cohort (table 4).
Table 4. Times between symptom onset and the first medical contact, and between electrocardiographic diagnosis and reperfusion (guidewire passage), in minutes, in the cohort of patients with ST-segment elevation acute coronary syndrome
| Variable | Total | Grupo A | Grupo B | Grupo C | p |
|---|---|---|---|---|---|
| Symptom onset-first medical contact (N = 332) | 120 [60-240] | 66 [45-180] (N = 97) | 120 [60-240] (N = 180) | 120 [60-240] (N = 55) | .007 |
| Diagnosis-reperfusion (N = 322) | 120 [60-180] | 120 [60-186] (N = 93) | 120 [60-225] (N = 176) | 60 [60-120] (N = 53) | .025 |
Data are expressed as median [interquartile range]. | |||||
DISCUSSION
The main findings from this study were a lower number of admissions due to ACS within the first few months of lockdown, and longer periods of time elapsed between symptom onset and the first medical contact in patients with STEACS that did not translate into higher morbidity and mortality rates.
Lower rate of acute coronary syndrome
Former studies have reported less activity at the cath lab due to fewer admissions due to ACS during the pandemic, especially in the STEACS setting.7,9-11 Our findings confirm this trend with a significant 41% drop within the first 30 days compared to the previous month. This reduction was kept in the remaining time during and after lockdown; however, as the isolation measures were being lifted and the rate of cases of COVID-19 dropped, a gradual increase in the number of admissions due to ACS was confirmed. One of the contributing factors may have been the intense pressure put to the healthcare system within the first few months of lockdown with the corresponding underdiagnosis of ACS and fewer admissions reported.12 Another hypothesis that may justified the lower rate of ACS during this time is the higher number of out-of-hospital sudden deaths reported. Although reported by other authors in the past, this was not cause for analysis in our study.13-16
Times elapsed among symptom onset, the first medical contact, and revascularization in patients with ST-segment elevation myocardial infarction, and association with adverse events
During the lockdown (group B) patients with STEACS were admitted more often (P = .003). The time elapsed between symptom onset and the first medical contact was significantly longer during this time compared to other times, which is consistent with the peak number of cases reported (similar findings to those reported by former studies);17 however, this delay did not increase the rates of mechanical complications or mortality. This can be explained because patients admitted during the lockdown (group B) were younger and had fewer comorbidities.18,19 Data suggests that elderly patients with more serious past medical histories and associated comorbidities may have delayed or even postponed indefinitely their access to the healthcare system over fears of getting infected.20,21
Rodríguez-Leor et al.22 reported time delays between symptom onset and the first medical contact, and similar times between diagnosis and reperfusion. This delay was associated with a higher mortality rate during the pandemic (7.5% vs 5.1%), which contradicts our findings. The lack of a direct association between time delays until diagnosis and the appearance of adverse events is not easy to explain. However, a plausible hypothesis can be the higher number of out-of-hospital sudden deaths reported due to mechanical complications or malignant arrhythmias followed by the corresponding selection bias since this study included hospitalized patients only.
Therapeutic strategies: percutaneous coronary intervention and surgical revascularization
No differences were found regarding the percutaneous invasive management of patients with ACS before, during or after lockdown. This data is consistent with most studies published on the management of ACS during the pandemic.12,22
However, we should mention the significant decrease of myocardial revascularization procedures despite the non-negligible number of patients with left main coronary artery disease or 3-vessel disease. A total of 17.7% of these patients were treated with myocardial revascularization 1 month before the lockdown, only 5.5% during the lockdown, and 34.5% the following month. Although some registries confirm the lower number of coronary artery bypass grafts performed,23 this tendency has not been confirmed in other studies.18,23
The fact that fewer myocardial revascularization procedures were performed during the lockdown can be explained by the overall tendency to delay any surgical acts as much as possible during these months, something already hypothesized in other studies.24
Limitations
This study has some limitations associated with the analysis of multicenter and observational data. Also, the study short follow-up period may have prevented the finding of potential consequences or differential events among the study groups. The lack of information on cases of ACS treated during the pandemic that never really made it to tertiary care centers also casts a shadow over the conclusions that can be drawn.
CONCLUSIONS
Significantly fewer admissions due to ACS were reported during the lockdown. Also, although time between symptom onset and the first medical contact was longer during this period in patients with STEACS, the mortality rate was similar among the 3 study groups.
FUNDING
None reported.
AUTHORS’ CONTRIBUTIONS
J. Echarte-Morales: clinical data mining, manuscript drafting, project design, and management of the study. C. Minguito-Carazo: data analysis, manuscript drafting and revision process. PL Cepas-Guillén, V. Vallejo García, ID. Poveda Pinedo, A. Salazar Rodríguez, E. Arbas Redondo, J. Guzmán Bofarull, and D. Tebar Márquez: data mining and manuscript revision process. E. Sánchez Muñoz: data mining. E. Martínez Gómez: data mining, manuscript drafting and revision process. T. Benito-González: statistical counselling, and manuscript revision process. M. López Benito, A. Viana Tejedor, I. Cruz-González, PL Sánchez Fernández, M. Sabaté, and F. Fernández-Vázquez: project organization. Authors submitting this manuscript accept full responsibility for its content as defined by the International Committee of Medical Journal Editors (ICMJE).
CONFLICTS OF INTEREST
None whatsoever.
WHAT IS KNOWN ABOUT THE TOPIC?
- Admissions due to STEACS decreased during the lockdown.
- More mechanical complications were reported during the pandemic due to delayed treatments.
WHAT DOES THIS STUDY ADD?
- Unlike former studies that mainly focused on patients with STEACS, this study includes patients admitted before, during, and 1 month after lockdown with a diagnosis of ACS (including STEACS and non-ST-segment elevation acute coronary syndrome).
- Fewer myocardial revascularization procedures were performed during the lockdown despite the growing number of patients with left main coronary artery disease or 3-vessel disease.
- Although time between symptom onset and the first medical contact was longer in the group of patients with STEACS, the mortality rate was similar before, during, and after lockdown, as it happened with mechanical complications.
REFERENCES
1. WHO. World Health Organization. Pneumonia of Unknown Cause –China. 2020. Available online:https://www.who.int/emergencies/disease-outbreak-news/item/2020-DON229. Accessed 20 Sep 2021.
2. Zhu N, Zhang D, Wang W, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382:727-733.
3. Morelli N, Rota E, Terracciano C, et al. The Baffling Case of Ischemic Stroke Disappearance from the Casualty Department in the COVID-19 Era. Eur Neurol. 2020;83:213-215.
4. Babu N, Kohli P, Mishra C, et al. To evaluate the effect of COVID-19 pandemic and national lockdown on patient care at a tertiary-care ophthalmology institute. Indian J Ophthalmol. 2020;68:1540-1544.
5. De Vincentiis L, Carr RA, Mariani MP, Ferrara G. Cancer diagnostic rates during the 2020 âlockdown', due to COVID-19 pandemic, compared with the 2018-2019:An audit study from cellular pathology. J Clin Pathol. 2021;74:187-189.
6. De Rosa S, Spaccarotella C, Basso C, et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;41:2083-2088.
7. Rodríguez-Leor O, Cid-Álvarez B, Ojeda S, et al. Impacto de la pandemia de COVID-19 sobre la actividad asistencial en cardiología intervencionista en España. REC Interv Cardiol. 2020;2:82-89.
8. Romaguera R, Cruz-González I, Jurado-Román A, et al. Consideraciones sobre el abordaje invasivo de la cardiopatía isquémica y estructural durante el brote de coronavirus COVID-19. REC Interv Cardiol. 2020;2:112-117.
9. Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-Segment Elevation Cardiac Catheterization Laboratory Activations in the United States During COVID-19 Pandemic. J Am Coll Cardiol. 2020;75:2871-2872.
10. Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19:The pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41:1852-1853.
11. Pessoa-Amorim G, Camm CF, Gajendragadkar P, et al. Admission of patients with STEMI since the outbreak of the COVID-19 pandemic:A survey by the european society of cardiology. Eur Heart J Qual Care Clin Outcomes. 2020;6:210-216.
12. Salinas P, Travieso-González A, Vergara-Uzcategui CE, Macaya F, Núñez-Gil IJ, Fernández-Ortiz A. Relación temporal entre ingresos por síndrome coronario agudo con tratamiento invasivo y confinamiento durante la pandemia de COVID-19. REC Interv Cardiol. 2020;2:307-309
13. Laura E. Wong;MD;PhD;Jessica E. Hawkins;MSEd;Simone Langness;Karen L. Murrell;Patricia Iris;MD &Amanda Sammann;MPH. Where Are All the Patients?Addressing Covid-19 Fear to Encourage Sick Patients to Seek Emergency Care. NEJM Catal. 2020. Available online:https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0193. Accessed 20 Sep 2021.
14. Lai PH, Lancet EA, Weiden MD, et al. Characteristics Associated with Out-of-Hospital Cardiac Arrests and Resuscitations during the Novel Coronavirus Disease 2019 Pandemic in New York City. JAMA Cardiol. 2020;5:1154-1163.
15. Marijon E, Karam N, Jost D, et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France:a population-based, observational study. Lancet Public Health. 2020;5:e437-e443.
16. Baldi E, Sechi GM, Mare C, et al. Out-of-Hospital Cardiac Arrest during the Covid-19 Outbreak in Italy. N Engl J Med. 2020;383:496-498.
17. Tam CCF, Cheung KS, Lam S, et al. Impact of Coronavirus Disease 2019 (COVID-19) Outbreak on ST-Segment-Elevation Myocardial Infarction Care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13:e006631.
18. Gluckman TJ, Wilson MA, Chiu ST, et al. Case Rates, Treatment Approaches, and Outcomes in Acute Myocardial Infarction during the Coronavirus Disease 2019 Pandemic. JAMA Cardiol. 2020;5:1419-1424.
19. Wu J, Mamas M, Rashid M, et al. Patient response, treatments, and mortality for acute myocardial infarction during the COVID-19 pandemic. Eur Heart J Qual Care Clin Outcomes. 2021;7:238-246.
20. Franchini S, Spessot M, Landoni G, et al. Stranger months:How SARS-CoV-2, fear of contagion, and lockdown measures impacted attendance and clinical activity during February and March 2020 at an urban Emergency Department in Milan. Disaster Med Public Health Prep. 2020;15(5):e33-e42.
21. Baldi E, Savastano S. Fear of contagion:One of the most devious enemies to fight during COVID-19 pandemic. Disaster Med Public Health Prep. 2021;15:e8-e9.
22. Rodríguez-Leor O, Cid-Álvarez B, Pérez de Prado A, et al. Impact of COVID-19 on ST-segment elevation myocardial infarction care. The Spanish experience. Rev Esp Cardiol. 2020;73:994-1002.
23. Mafham MM, Spata E, Goldacre R, et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;39:381-389.
24. Álvarez Gallego M, Gortázar de las Casas S, Pascual Migueláñez I, et al. SARS-CoV-2 pandemic on the activity and professionals of a General Surgery and Digestive Surgery Service in a tertiary hospital. Cir Esp. 2020;98:320-327.
* Corresponding author:
E-mail address: juliocecharte@gmail.com (J. Echarte Morales).