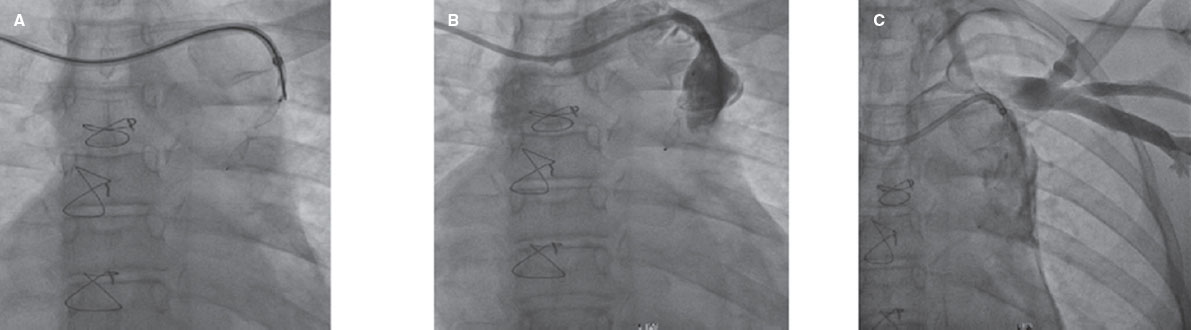
QUESTION: What would you say is the current state of the evidence on the closure of the patent foramen ovale (PFO)?
ANSWER: Recent randomized clinical trials show greater benefits with the closure of the PFO compared to the medical therapy in patients with PFO-related cryptogenic stroke (CS).1-4 Despite a 64% risk reduction this benefit is only applicable to “high-risk patients” and requires a high number needed to treat (130 patients).5 Also, there are several gaps that prevent the generalization of its therapeutic indication and required individual indications for every patient.
In spite of everything, to this day there is enough body of knowledge for the reasoned indication of medical therapy or the percutaneous closure of the PFO in patients with PFO-related CS. In this context, the European take on this issue may help. A document signed by 8 scientific societies including the European Association of Percutaneous Cardiovascular Interventions (EAPCI), the European Heart Rhythm Association (EHRA), the European Association for Cardiovascular Imaging (EACVI), and the European Stroke Organisation (ESO).6
The arrival of a new technology or therapy is often like a rollercoaster and the closure of the PFO is not an exception. New discoveries and therapies are followed by unjustified euphoria based on intuition, which eventually leads to overuse. Also, there is no real evidence of its effectiveness followed by a significant risk for iatrogenic disease and, at best, a considerable futile investment. This is precisely what happened during the years when observational and cohort studies were conducted (from 1995 to 2011 approximately). Years of “disbelieve and denial” followed the appearance of the first results of clinical trials, all of which were negative.7-9 The generalized refusal of the percutaneous closure of the PFO that followed these studies (from 2012 through 2018) was not justified either as the positive results of 4 clinical trials recently published show.1-4
Q.: Why do you think it has taken so many years since the first trial was conducted to show the benefits of the closure of the PFO? What is the difference between the first studies that were not positive and the latest ones that are?
A.: The problem with PFO-related CS is that it is not a very aggressive type of stroke with 2 key aspects that make it difficult to obtain solid results in the studies conducted:
-
- The PFO is very prevalent in healthy populations where it is not a relevant risk factor, which is a significant confounding factor.
-
- In patients with PFO-related CS, the risk of recurrence is low (annual 0.20% to 1.27%),5,6 and both the traditional antiplatelet therapy and the percutaneous closure are effective.
The mere fact of showing traditional vascular risk factors like smoking, hypertension, diabetes or old age involves a higher risk of an early stroke and a higher risk of recurrence compared to the presence of PFO. This adds extra difficulty to the routine clinical practice since traditional vascular risk factors coexist with the presence of PFO.
The main problem here is to identify the subgroup of patients in whom the PFO is the direct cause for the stroke. Also, if the study design is assessing the effectiveness of a therapy regarding the risk of recurrence—since it is low—it requires, at best, a large sample and long follow-up. As an added difficulty, preemptive therapy with antiplatelet drugs is effective for the prevention of stroke recurrences in this context. Also, all clinical studies should be compared to this control group since it is already receiving effective treatment.
These aspects can be easily seen in 1 of the 3 negative studies published in 2012 (RESPECT),8 which becomes 1 of the 4 positive studies after the 9-year follow-up of the original population who participated in the clinical trial was published back in 2017.3
Q.: From the clinical perspective and imaging modality standpoint, what patients are good candidates to benefit from the closure of the PFO?
A: The presence of septal aneurysm or the detection of moderate-acute shunt have been strongly associated with the PFO as the cause for the CS both in clinical and observational studies6,7 and with the benefits of closure compared to medical therapy.
The therapeutic decision and, in particular, the option to perform the closure of the PFO in patients who have suffered from a CS should be based on how we answer to these 2 questions:
-
- What are the chances that the PFO identified in the patient is the cause for the stroke and not just an innocent witness?
-
- If the PFO is the probable cause for the stroke, what is the risk of recurrence?
The most relevant utility factors to confirm the probability that the PFO is the direct cause for the CS are:
-
- Septal aneurysm.
-
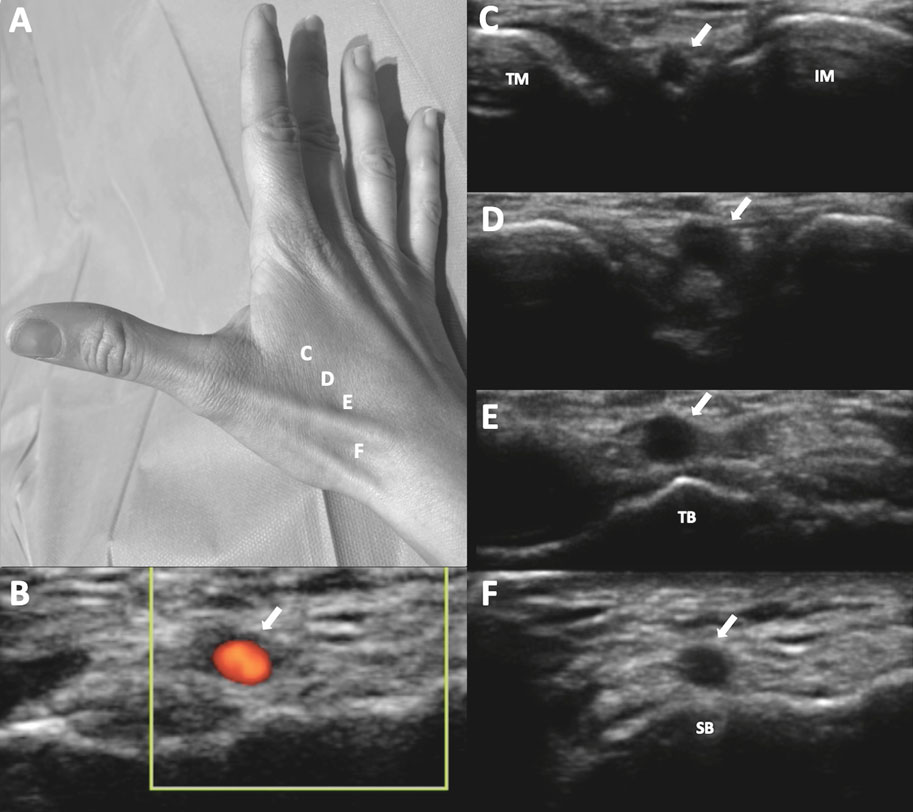
- Moderate-acute right-to-left shunt (corresponding to the shower and curtain patterns on the transcranial Doppler ultrasound).
-
- Presence of deep vein thrombosis.
Other less relevant factors identified given the lack of prospective studies are:
-
- The presence of Eustachian valve, Chiari network or PFO extensive channel.
-
- Clinical aspects indicative of paradoxical embolism: consistent with the Valsalva maneuver, prolonged immobilization, tourist class syndrome, thrombophilic status, etc.
-
- Age < 55 years old.
-
Score obtained in the RoPE grading system10 as an additional tool in this evaluation and in association with previous parameters.
-
- Lack of traditional cardiovascular risk factors.
No neuroimaging patterns have been identified consistently associated with the causal role played by the PFO in the development of CS.
Regarding the assessment of the risk of recurrence, no variable per se facilitates any quantitative predictions.
The high-risk patients of clinical trials should be candidates for the closure of the PFO because they are the subgroup in which the analysis of results shows clinical and statistically significant differences (relative risk, 0.27; 95% confidence interval [95%CI], 0.11-0.70).5
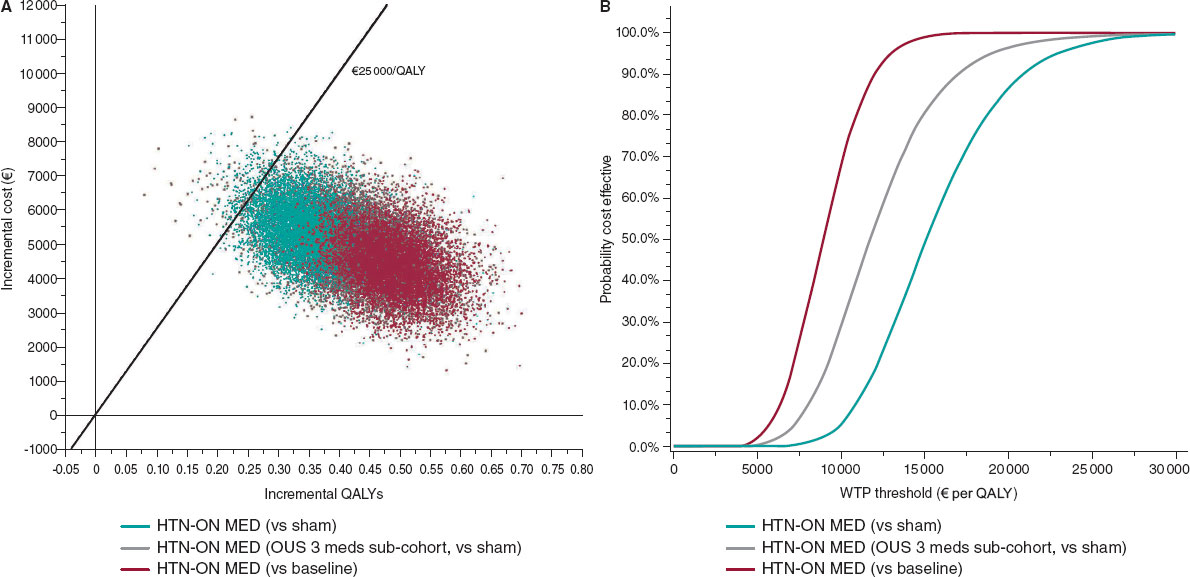
Old age does not exclude a causal PFO-related CS. As a matter of fact, a similar risk has been reported in young patients. However, to this day we should not consider the percutaneous closure of the PFO given the relatively low risk of recurrence, the profile of patients in the clinical trials (18-60 years old), and the long-term benefit shown with an unfavorable cost-effectiveness ratio for the percutaneous closure in this age group.
To indicate the closure of the PFO these factors are especially important:
-
- Interatrial septal aneurysm (odds ratio [OR], 3.0; 95%CI, 1.8-4.8).
-
- PFO of a large size or right-to-left shunt (OR, 3.0; 95%CI, 1.9-4.6).
-
- In particular, the association between interatrial septal aneurysm and acute shunt.
Other factors identified that should be taken into account are:
-
- Thrombophilic status (OR, 2.75; 95%CI: 1.17-6.49).
-
- Previous treatment with acetylsalicylic acid vs oral anticoagulants (OR, 2.5; 95%CI, 1.1-6.1).
-
- Infarction vs transient ischemic attack as clinical presentation including infarction seen on neuroimages (OR, 3.0; 95%CI, 1.4-6.5).
Q.: What is the best medical therapy after the closure of the PFO?
A.: There is significant controversy among the different guidelines and there are no solid pieces of evidence. Considering that the endothelization process can extend for up to 5 years after the implantation,6 that clinical trials kept antiplatelet therapy for, at least, 2 years (5 years in 2 of them), and the overall behavior of ischemic stroke and, in particular, CS the pattern should be: keep dual antiplatelet therapy for a month and continue with single antiplatelet therapy (acetylsalicylic acid, 100 mg/day) for, at least, 2 years (5 years if we follow the European recommendation).
At 5 years, before withdrawing antiplatelet therapy, the patient should be assessed by a stroke expert to decide on the withdrawal of the treatment based on the patient’s clinical profile (age, coexisting factors of vascular risk, PFO total occlusion or residual shunt, life habits, tolerance to treatment, etc.).
Q.: Which should be the next trial in this setting?
A.: These are some of the aspects that are still under discussion and should be taken into consideration in future trials:
-
- Better identification of the profile of high-risk patients including the analysis of additional or current risk factors (older age, severity of shunt in baseline conditions, size of interatrial septal aneurysm, presence of Chiari network or Eustachian valve, etc.).
-
- Conduct adequately designed clinical trials to see the potential benefits of direct-acting oral anticoagulants compared to the percutaneous closure of the PFO.
-
- Obtain long-term follow-up information since the potential benefit of the closure of the PFO is cumulative over time and the long-term risk of medical therapy is not very well known.
-
- Assess not only the risk of recurrence, but also quality of life including the degree of disability in basic activities of daily living after recurrence (eg, routine use of the Rankin modified scale in acute stroke studies).
Additionally, observational prospective registries should be conducted in the clinical practice.
In conclusion, to this day we have enough scientific evidence to conclude that the closure of the PFO is superior to antithrombotic therapy regarding the risk of recurrence in patients with PFO-related CS. Patients with interatrial septal aneurysm or massive shunt could benefit the most from this intervention. Future studies should analyze the closure of the PFO in patients not included in the trials like patients > 60 years and patients with other associated cardiovascular risk factors.
CONFLICTS OF INTEREST
None reported.
REFERENCES
1. Søndergaard L, Kasner SE, Rhodes JF, et al. Patent Foramen Ovale Closure or Antiplatelet Therapy for Cryptogenic Stroke. N Engl J Med. 2017;377:1033-1042.
2. Mas JL, Derumeaux G, Guillon B, et al.;CLOSE Investigators. Patent Foramen Ovale Closure or Anticoagulation vs. Antiplatelets after Stroke. N Engl J Med. 2017;377:1011-1021.
3. Saver JL, Carroll JD, Thaler DE, et al.;for the RESPECT Investigators. Long-Term Outcomes of Patent Foramen Ovale Closure or Medical Therapy after Stroke. N Engl J Med. 2017;377:1022-1032.
4. Lee PH, Song JK, Kim JS, et al. Cryptogenic Stroke and High-Risk Patent Foramen Ovale:The DEFENSE-PFO Trial. J Am Coll Cardiol. 2018;71:2335-2342.
5. Turc G, Calvet D, Guérin P, et al.;CLOSE Investigators. Closure, Anticoagulation, or Antiplatelet Therapy for Cryptogenic Stroke With Patent Foramen Ovale:Systematic Review of Randomized Trials, Sequential Meta?Analysis, and New Insights From the CLOSE Study. J Am Heart Assoc. 2018;7:e008356.
6. Pristipino C, Sievert H, D'Ascenzo F, et al. European position paper on the management of patients with patent foramen ovale. General approach and left circulation thromboembolism. Eur Heart J. 2019;40:3182-3195.
7. Furlan AJ, Reisman M, Massaro J, et al.;CLOSURE I Investigators. Closure or medical therapy for cryptogenic stroke with patent foramen ovale. N Engl J Med. 2012;366:991-999.
8. Carroll JD, SaverJL, Thaler DE, et al.;RESPECT Investigators. Closure of patent foramen ovale versus medical therapy after cryptogenic stroke. N Engl J Med. 2013;368:1092-1100.
9. Meier B, Kalesan B, Mattle HP, et al.;PC Trial Investigators. Percutaneous closure of patent foramen ovale in cryptogenic embolism. N Engl J Med. 2013;368:1083-1091.
10. Kent DM, Ruthazer R, Weimar C, et al. An index to identify stroke-related vs incidental patent foramen ovale in cryptogenic stroke. Neurology. 2013;81:619-625.
Corresponding author: Unidad de Ictus, Servicio de Neurología, Hospital Universitario de Girona Dr. Josep Trueta, Avda. Francia s/n, 17007 Girona, Spain.
E-mail address: jserena.girona.ics@gencat.cat (J. Serena Leal).