ABSTRACT
In this article, we analyse the changes occurred over the last 20 years in the percutaneous treatment of bifurcation lesions based on our own experience. We also analyse the more relevant papers recently published, as well as the strategies and guidelines recommended for the percutaneous management of bifurcation lesions. Technical aspects are relevant in this field and, for this reason, a significant section of this manuscript is dedicated to the technique used together with some tips and tricks also provided here. The technical advances made over the last years have significantly increased the success rate in the management of these complex lesions. At the same time, the technique of treatment has been standardized allowing the management of all type of bifurcations including distal left main disease.
Keywords: Coronary heart disease. Coronary bifurcation lesions. Stents. Percutaneous treatment.
RESUMEN
En este artículo se revisan los cambios acaecidos durante los últimos 20 años en el tratamiento percutáneo de las lesiones en bifurcación bajo la perspectiva de nuestra experiencia. También se analizan los estudios más relevantes en este campo, así como las estrategias y las recomendaciones actuales. Los aspectos técnicos son fundamentales en el tratamiento de las lesiones en bifurcación, por lo que parte de la revisión se dedica a ellos. Las mejoras técnicas aparecidas en los últimos años han sido determinantes en el aumento de la tasa de éxito del tratamiento de este tipo de lesiones complejas. Al mismo tiempo, la estrategia terapéutica ha sido reglada y estandarizada, de modo que actualmente podemos abordar con seguridad todo tipo de lesiones en bifurcación, incluida la enfermedad del tronco común de la arteria coronaria izquierda.
Palabras clave: Enfermedad coronaria. Lesiones coronarias en bifurcación. Stents. Tratamiento percutáneo.
INTRODUCTION
Bifurcation lesions are a common group of lesions (20%-30%) we usually see at the cath. lab.1 Although they fall within the category of complex lesions, the management of these lesions has improved favorably over the last few years in such a way that today there is a new generation of stents and co-adjuvant techniques to angiography available that are very effective in the management of such lesions. At the same time, the therapeutic strategy has been standardized and regulated,2 with success rates that are higher compared to years ago. Thus, to this day it is possible to approach all sorts of bifurcations including bifurcations of the left main coronary artery disease.3 However, it has been a long 20-year-old road before reaching the actual standards of management that we have today.
HISTORIC PERSPECTIVE
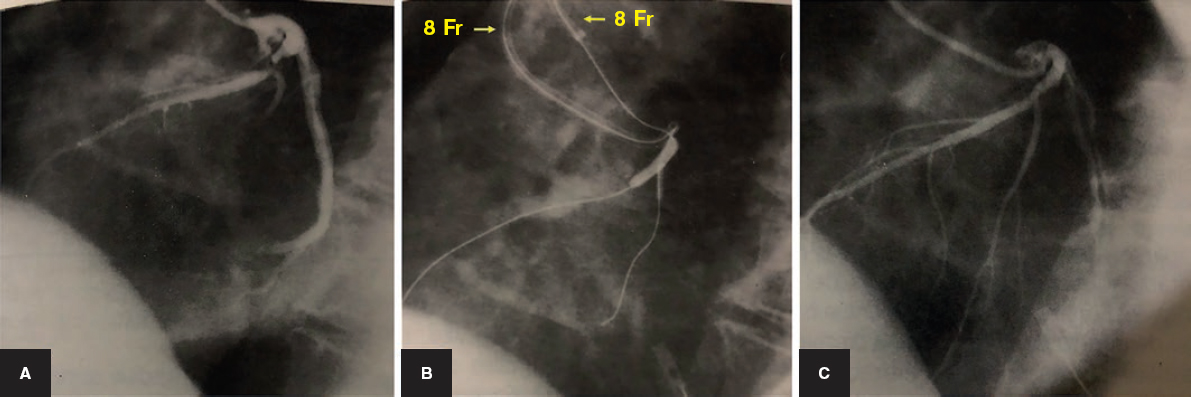
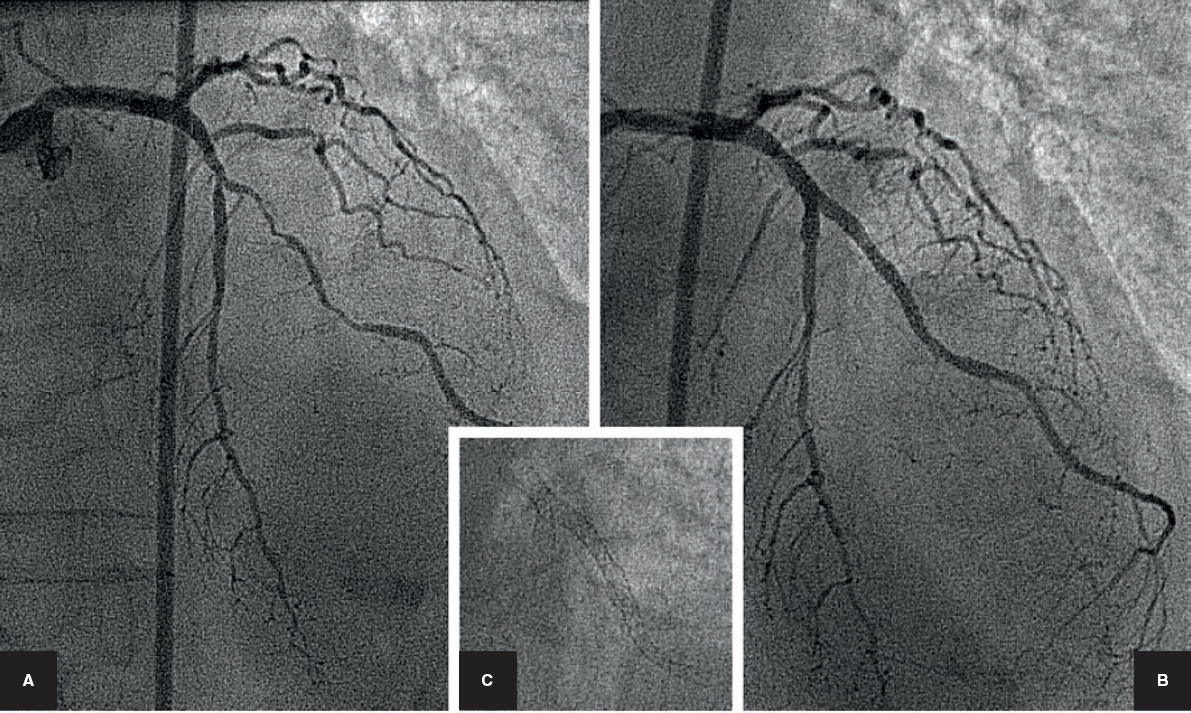
The percutaneous management of bifurcations started in the era of balloon angioplasty that was available before the arrival of coronary stents. At the time, there were already specific techniques available such as the use of two 8 Fr guiding catheters through which guidewires and balloons would be inserted independently in the main branch (MB) and side branch (SB) to proceed with simultaneous inflation (figure 1). However, the turning point in the percutaneous management of bifurcations came with the arrival of the Palmaz-Schatz stent. The was the first technique ever to describe a simple balloon dilation of the SB through the stent cells.4 After that, we would see a never-ending cascade of techniques for the management of both vessels using 1 or 2 stents. With the arrival of drug-eluting stents, all coronary procedures improved. When it comes to the management of bifurcations, the experience acquired during the era of bare-metal stents contributed to the development of new and complex techniques: the crush technique and its variants, the TAP (T with protrusion), and the simultaneous kissing stent (SKS) techniques.
Figure 1. Bifurcation in the anterior descending artery/diagonal branch branch. Percutaneous treatment prior to the era of stents. A: baseline angiography. B: balloon dilation of the anterior descending and diagonal arteries. Two 8 Fr femoral guiding catheters with guidewires and independent balloons for simultaneous balloon dilation (kissing balloon). C: final outcome.
DEFINITION OF BIFURCATION LESIONS
Coronary bifurcation lesions are lesions adjacent to the division of one major pericardial artery. The definition of significant SB is arbitrary and totally depends on the interventional cardiologist´s subjective criteria.5 Although in the very definition we can see the lack of consensus on what is considered significant and what is not, most studies talk about bifurcations with SB > 2.2 mm. The differential characteristic of these lesions compared to conventional lesions is that when we act on the MB, we can compromise the SB due to the displacement of the carina or the atherosclerotic plaque. That is why we need specific strategies to solve this situation.
CLASSIFICATION OF BIFURCATION LESIONS
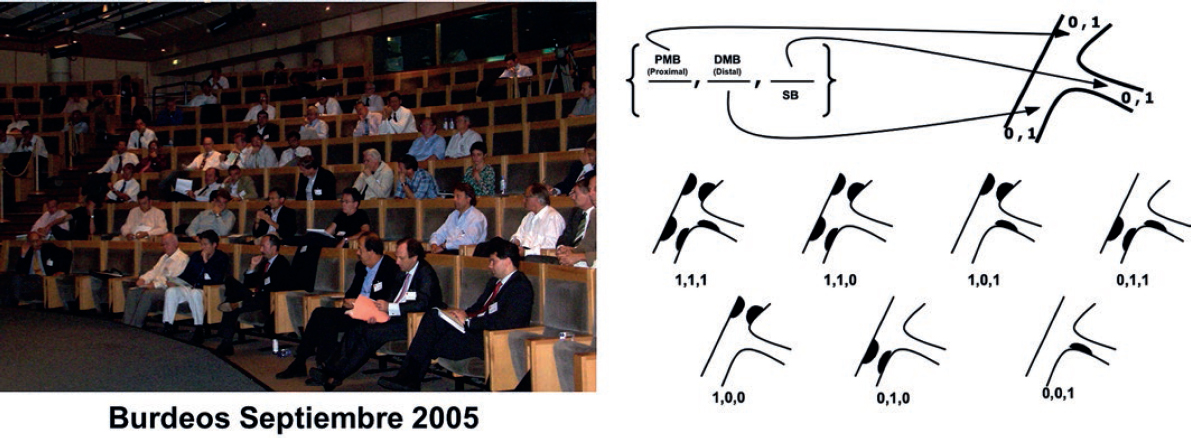
Several classifications have been proposed to define the baseline characteristics of bifurcations, some of them during the era of bare-metal stents. However, the most widely accepted of all is the classification established by Medina6 (figure 2). Its success is due to its simplicity when it comes to memorizing it. This classification was first accepted back in 2005 during the first congress held by the European Bifurcation Club in Bordeaux, France (figure 2). Here the authors of the Massy classification rejected their own classification for the adoption of the new one6 as the only proposal made by this group. This extraordinary event, the bith of a classification, was published in Revista Española de Cardiología and reached a record number of citations (actually it is the most cited article to this day).
Figure 2. To the left: Bordeaux congress from September 2005, where the Medina classification was established as the only accepted classification by the European Bifurcation Club. To the right: Medina classification reproduced with permission from Medina et al.6 DMB, distal main branch; PMB, proximal main branch; SB, side branch.
PERCUTANEOUS MANAGEMENT OF BIFURCATION LESIONS
Over the last few years, a great number of different techniques have appeared for the management of coronary bifurcation lesion with the use of stents. In an attempt to systematize them all, the European Bifurcation Club has proposed the MADS (Main, Across, Double, Side) classification.7 According to this classification, there are numerous different modalities of treatment. However, for simplification purposes, an easier classification has been proposed including simple (1 stent in MB) and complex (2 stents in MB and SB) techniques. Both strategies have been compared over and over again both in the era of bare-metal stents and the actual era of drug-eluting stents.
Description of simple techniques. The provisional stenting technique as a treatment philosophy
The provisional stenting approach basically consists of implanting 1 stent in the MB and then see what impact this has on the SB.2 The stent can be covered, dilated with balloon or it stented based on the actual flow and residual stenosis. To this end, 2 guidewires are introduced, one in the MB and another one in the SB. The size of the stent that will be implanted in the MB is picked based on the length of the diseased section and the reference diameter of the distal vessel. After the implantation, the POT (proximal optimization technique) should be used. The POT consists of the dilation of the stent proximal edge with a short balloon but with a wider diameter compared to the diameter of the release balloon and according to the proximal segment. By doing this, the proximal stent is adapted to a vessel that has a wider diameter compared to the distal component of the bifurcation which, if needed, facilitates the re-crossing of the SB. At this point, the state of the origin of the collateral branch should be assessed. In the absence of significant stenosis or if the vessel is small and with TIMI (Thrombolysis in Myocardial Infarction) flow 3, the procedure is considered finished. If the origin of a major branch has been compromised, a second guidewire should be passed towards the branch in order to treat it, and the jailed guidewire should be extracted. The inflation of the balloon can be performed simultaneously using a second balloon in the MB (the so-called kissing balloon) or in isolation.8 A second POT is recommended especially if the simultaneous inflation is not attempted. Most bifurcations have good outcomes when implementing these maneuvers. However, in a variable percentage of cases, the origin of the collateral branch maintains a suboptimal outcome and requires the implantation of a second stent followed by final kissing balloon inflation.2
The jailed guidewire technique
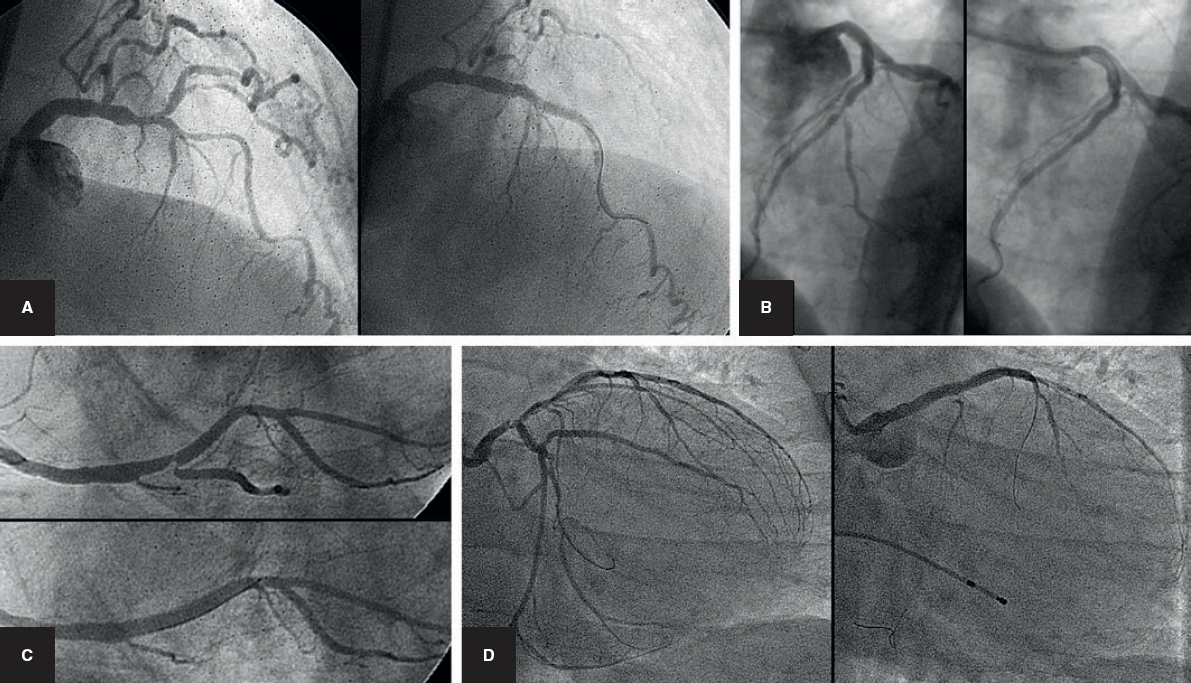
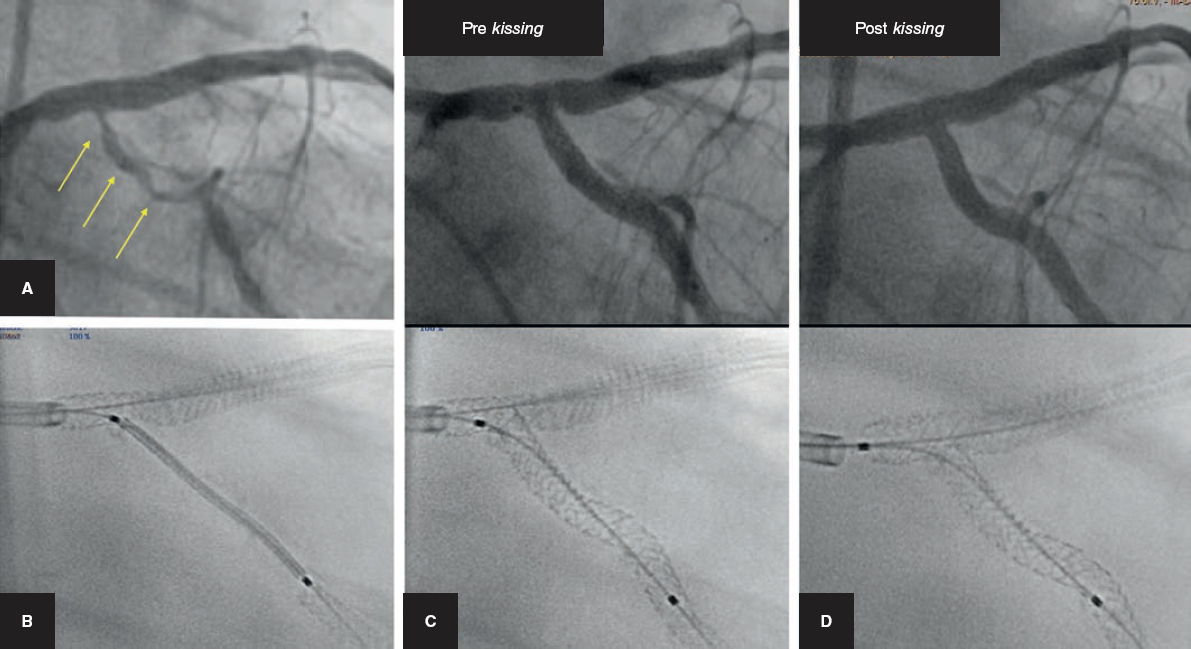
The provisional stenting technique is often called «simple technique», although there are times when it is not as simple as it seems especially when the SB becomes occluded after implanting the stent in the MB (figure 3). If unsolved, this situation will lead to the occurrence of an acute myocardial infarction. The jailed guidewire technique was described to help solve this situation. It consists of leaving a guidewire in the SB while a stent is implanted in the MB. By doing this, the guidewire is somehow jailed between the vessel wall and the metallic structure of the stent.
Figure 3. Four examples of side branch sudden occlusion following the implantation of the stent into the main branch. A and B: anterior descending artery/diagonal branch. C: right coronary artery/posterior descending artery. D: left main coronary artery with closure of circumflex artery.
Its advantages are:
-
The jailed guidewire helps keep the SB open and, in case of SB occlusion, the guidewire becomes the only marker of its position, which facilitates bailout maneuvers in the occluded vessel.
-
It facilitates access to the SB since it successfully modifies the bifurcation angle.
-
It produces a mechanism that anchors the guidewire which, in turn, facilitates the intubation of the guiding catheter by providing more solid support to attempt the crossing of the origin of the SB with the balloon.
-
Finally, in extreme situations, it can be used to introduce a low-profile balloon, for SB dilation purposes, and eventually to implement the inverted crush technique or re-dilate the stent crushed inside the MB once the occlusion of the branch has been solved.9
Risks involved when using the jailed guidewire technique. Since the MB stent is implanted using pressure against the arterial wall, the guidewire jailed between these 2 structures can be damaged and even break when removed.10 Although rare, cases of guidewire rupture have been reported during the extraction maneuvers; this is a serious complication of this procedure that sometimes requires urgent surgical extraction.11-13 Several recommendations have been made to prevent the rupture of the guidewire:14 a) avoid placing the distal portion of the guidewire in secondary vessels of small caliber; b) avoid high pressures when releasing the stent; c) avoid covering a large area of the jailed guidewire with a series of stents; and d) use the most traction-resistant guidewire. However, this last recommendation has been controversial over the last few years. Thus, initially, the use of non-polymeric guidewires was recommended following the experts’ opinions.15,16 However, a randomized trial conducted to study the damage sustained by the guidewire after being jailed using stereoscopic microscopy revealed that polymeric guidewires were more resistant and sustained less damaged.10 However, the new generation of guidewires should be put to the test for this indication.
Pre-dilation or not of the side branch prior to implanting the stent in the main branch
The pre-dilation of the side branch has also been controversial over the last few years. This maneuver has a series of advantages and disadvantages that we will be commenting now:
-
Possible advantages: the dilation of the SB would increase the vessel lumen and facilitate re-wiring (re-crossing); it could help maintain flow to the SB and avoid its occlusion after implanting stent into the MB; also, the implantation of the stent into the MB could be the ultimate procedure without having to post-dilate. This is how the procedure could be simplified and the production of deformities inside the MB stent avoided.
-
Disadvantages: the presence of one dissection at the origin of the SB could obstruct the passage of the guidewire which would be forced to cross the stent of the MB and the dissected segment of the SB. The luminal increase at the origin of the SB increases the chances of accessing this vessel through the proximal cell of the stent of the MB, which is associated with more deformity of the MB stent and lack of scaffold at the origin of the SB, thereby increasing the changes of a second stent inside the SB.17,18
In order to shed some light on the issue of SB pre-dilation when using the provisional stenting technique, our group conducted one randomized trial that compared patients with true bifurcations treated with this strategy plus pre-dilation, or not, of the SB.19 The primary endpoint of assessment (the presence of TIMI flow 0-1 in the SB right after the implantation of the stent inside the MB) was significantly lower (1% vs 10%; P < .001) in the pre-dilation arm. Also, 32% of predilated patients did not require additional treatment on the branch, which simplified the entire procedure. In the remaining patients who did require post-dilation, the pre-dilation was no problem at all for guidewire re-crossing purposes. After this study several registries appeared in favor of this maneuver20 or opposing it.21,22 In general, the pre-dilation of the SB is left at operator’s discretion and recommended when the SB shows a difficult- to-access, serious, calcified lesion at its origin or compromised coronary flow at baseline level or after the pre-dilation of the MB.2
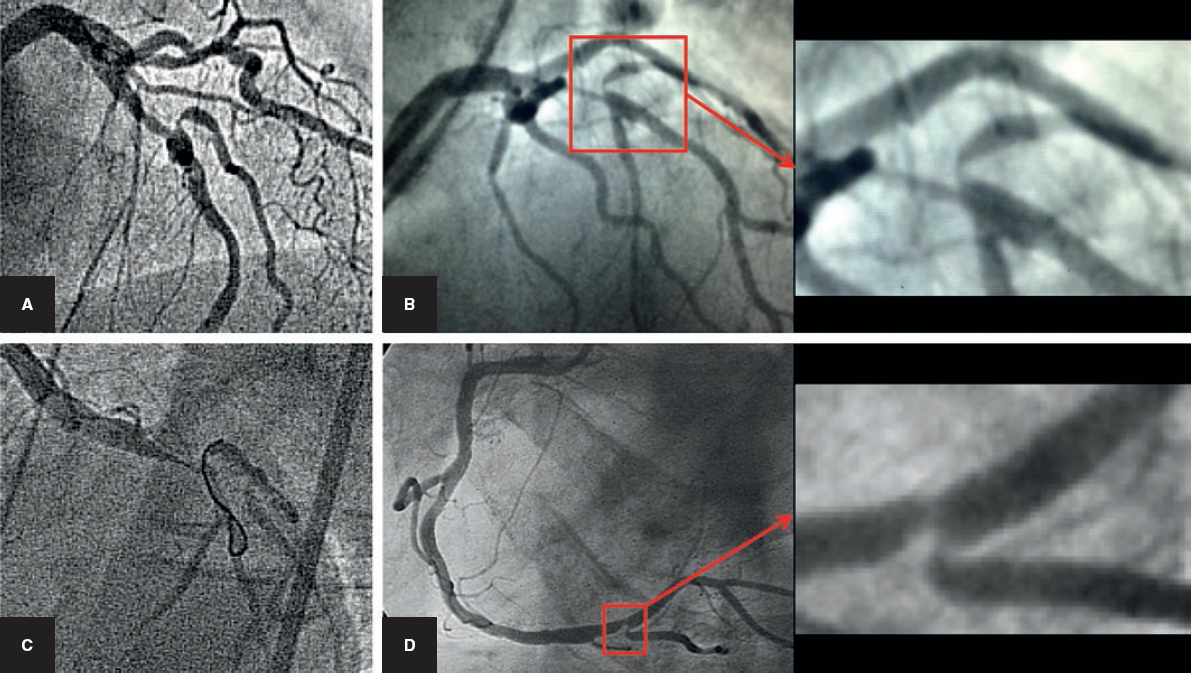
Difficult access to the side branch
This circumstance is still a problem in the management of bifurcations. Excessive angulations, calcifications, and diffuse lesions can obstruct the introduction of the guidewire into the SB (figure 4). And the situation becomes worse after implanting the stent into de MB due to the interposition of a metal layer, more stenosis or even its closure at the origin of the SB. In order to solve this, specific devices and ingenious techniques have been developed for wiring the SB. Deflectable tip catheters or catheters with highly-angulated tips are some of these new devices23 that can be oriented towards the origin of the SB. Double lumen catheters allow us to use highly-angulated guidewires through the lateral exit with the possibility of moving the entire system back and forth until reaching the origin of the SB.24 Sometimes this is very hard to do and it is an actual problem we have today in a small number of cases.
Figure 4. Difficult access to the side branch. A, B, and C: anterior descending artery/diagonal branch. D: right coronary artery/posterior descending artery. To the right: bifurcation angle in detail.
Description of complex techniques with 2 stents
The mini-crush, culotte, TAP, and T-stenting techniques starting at the sister branch are widely used techniques when planning 2-stent strategies. All of them were described in detail in a classical review conducted by Louvard et al.15. However, most recently, the double kissing crush (DK crush) technique has gained popularity following the results of a series of randomized clinical trials.25 In the double kissing crush technique, one guidewire is introduced into the MB and SB and then both vessels are predilated. While keeping the guidewire inside the MB, a stent is released into the SB with a 2-4 mm protrusion in the MB. One balloon is advanced into the MB and the stent is implanted into the SB. The balloon is extracted from the SB and the MB balloon is inflated crushing the entire proximal edge of the SB stent. A new re-wiring of the SB is attempted and 2 balloons are introduced for simultaneous inflation (first kissing balloon). The balloons and the SB guidewire are removed and the stent is implanted into the MB covering the SB. The balloon is then removed and a new re-wiring of the SB is attempted. Two balloons are introduced, and the second balloon is simultaneously inflated (second kissing balloon).
Comparison between simple and complex techniques
As mentioned before, this type of comparison has been drawn many times in the medical literature. First, during the era of non-drug-eluting stents,26 and even though no randomized clinical trials were conducted at the time, all observational comparisons suggested better results when using simple techniques.26 During the era of drug-eluting stents, the trials were conducted again, randomized trials this time,27-32 and they confirmed the previous findings on the non-superiority of complex techniques over the simple ones. These results also showed an abundance of meta-analyses that collected the same comparative studies and came to the same conclusions.33-37 Thus, the European Bifurcation Club and European guidelines both recommend the use of the provisional stenting technique for the management of most coronary bifurcation lesions.38 However, during the Transcatheter Cardiovascular Therapeutics Congress of 2017 the tables were turned after the presentation of the DKCRUSH-V25 trial that confirmed better results with the DK crush technique versus the provisional stenting technique for the management of left main coronary artery bifurcations. These findings contradicted all comparative studies published to that date. Also, the same group had already disclosed the same results for the management of bifurcations outside the left main coronary artery.39 If we take these findings into consideration, we would have to change entirely our strategy when it comes to the management of bifurcations. What has been the reaction of the international scientific community to this?
While some have accepted this with no questions asked, others have criticized the paper published by Chen et al.25. We believe it has important limitations. Thus, in the arm of the provisional stenting technique no POT was used after the implantation of the stent in the left main coronary artery prior to the re-wiring of the circumflex artery. The percentage of patients randomized to the provisional stenting technique who crossed to 2-stent techniques was high (47%) and the rate of stent thrombosis (3.3%) too; both percentages are much higher that the percentages reported by other recent studies. Finally, most target lesion reinterventions at follow-up happened annually during the systematic angiographic reevaluation period. Thus, the last guidelines published so far on the management of revascularization38 have issued a type IA recommendation to the provisional stenting technique (stronger recommendation than the one issued by former guidelines), while the DK crush technique has received a IIb recommendation only.
When should we plan a 2-stent technique right from the start?
Although, after all the studies published so far, there is general consensus on the use of the provisional stenting technique in most bifurcation lesions, there are special situations where 2 stent-techniques offer more advantages compared to the use of simple strategies:
-
The first obvious situation here is when we have suboptimal outcomes in the SB when using the provisional stenting technique. Although this situation may seem clear to us, there is still controversy on what these suboptimal outcomes actually are. In this sense, coronary flows in the SB below TIMI 3 or the presence of a type A dissection are considered poor outcomes. However, the percentage of crossing to 2 stents is highly variable from one series to the next (from 2% to > 50%),27-32,40 which may explain the lack of consensus on what poor outcomes in the SB really are.
-
Another situation that may be an indication for using the 2-stent technique from the beginning is the presence of a long or diffuse lesion in a major SB. In these cases, it is assumed that the balloon angioplasty will not be successful (figure 5).
-
Difficult access to the SB also seems like a good indication for stenting but only if the guidewire has been successfully inserted. Here the implantation of the stent into the MB may complicate things even more, which is why the 2-stent technique starting at the SB is recommended.
-
When one bifurcation lesion is associated with a coronary occlusion, we may have important dissections affecting the origin of the SB induced by the process of recanalization.41,42 Once again, in these case, the elective implantation of a stent into the SB prior to implanting another stent into the MB may be a good strategy.
-
Lastly, SB restenosis after performing one simple procedure should also be followed by a second stent implanted in the SB (figure 6).43
Figure 5. Bifurcation in the anterior descending artery with diffuse lesion in the side branch. Use of 2-stent technique from the beginning (cullotte). A: baseline angiography. B: final outcome. C: image obtained without contrast of the 2 stents.
Figure 6. A: diffuse restenosis of the origin of the circumflex artery after treatment using the provisional stenting technique of left main coronary artery. Treatment using a second stent (T with protrusion in 2 stages). B, C, and D: stent boost of left main coronary artery during the different steps of the technique.
ALTERNATIVES TO THE CORONARY ANGIOGRAPHY IN THE ASSESSMENT OF BIFURCATION LESIONS: IMAGING MODALITIES AND CORONARY PHYSIOLOGY
Intravascular ultrasound
The intravascular ultrasound (IVUS) is a useful tool to assess the lesion prior to treatment and the outcomes after the implantation of the stent. It provides information on the baseline anatomy of the lesion and the distribution of the plaque. This information allows us to make specific selections of the diameter and length of the stent we’ll use, and is of paramount importance in the bifurcation of the left main coronary artery.44 Additionally, the longitudinal withdrawal of IVUS allows us to look into the shape of the carina.45,46 One sharp carina (the so-called eyebrow sign described by Medina) predicts a high risk of compromise of the SB after the implantation of the stent into the MB.45,46
Once the stent has been implanted, the IVUS is useful for the identification of deformities, under expansions and dissection of the stent edges.47,48 All of these anomalies can be corrected and lead to immediate better outcomes, which has a positive impact on the follow-up of these patients.
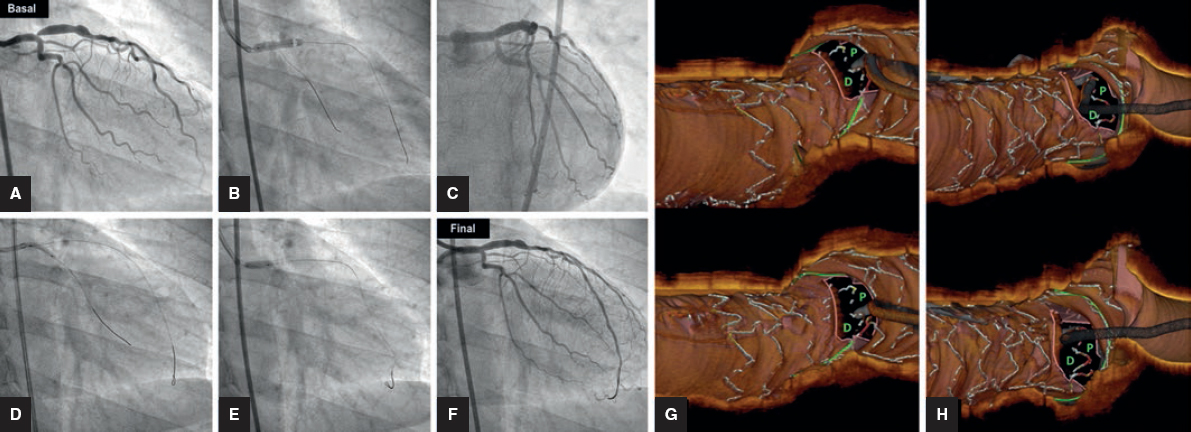
Optical coherence tomography
The optical coherence tomography is another recent imaging modality that is actually newer than the IVUS. It has more resolution compared to the IVUS but not so much power of penetration. Another setback is that to be able to actually see the artery, the blood from the lumen needs to be cleaned using contrast or dextran.
During pre-treatment assessment, the optical coherence tomography provides similar information to the IVUS with the aforementioned advantages and drawbacks. Helping in the visualization of stent struts has really been revolutionary. Its resolution added to a new software allow the reconstruction of the stent almost as if we were looking at an in vitro study. It is a highly sensitive imaging modality for the identification of deformations, malappositions, and no expansions of the stent. At the same time, it gives us accurate information on the vessel-stent correlation, especially among the different cells and the origin of the SB. Also, it is the only imaging modality capable of establishing this correlation. Therefore, it allows us to diagnose the access to the SB through the proximal or distal cell. The recommendation here based on in vitro studies is to access through the distal cell, which provides better scaffolding of the branch and less deformity of the stent implanted in the MB. Monitoring the procedure through optical coherence tomography allows us to identify a proximal access and correct it for a more distal one (figure 7). The utility of this imaging modality for the management of bifurcations has been established in a consensus document approved by the European Bifurcation Club.49
Figure 7. Treatment of an ostial lesion of the anterior descending artery using the provisional stenting technique. A: baseline angiography. B: stent in left main coronary artery/anterior descending artery. C: Compromise to the origin of the circumflex artery. D: dilation of the circumflex artery. E: proximal re-dilation (Re-POT). F: angiographic findings. G: optical coherence tomography, incorrect wiring of the circumflex artery through the proximal (P) cell. H: after a second attempt, the optical coherence tomography shows the guidewire through the distal cell (D) where dilation will finally occur.
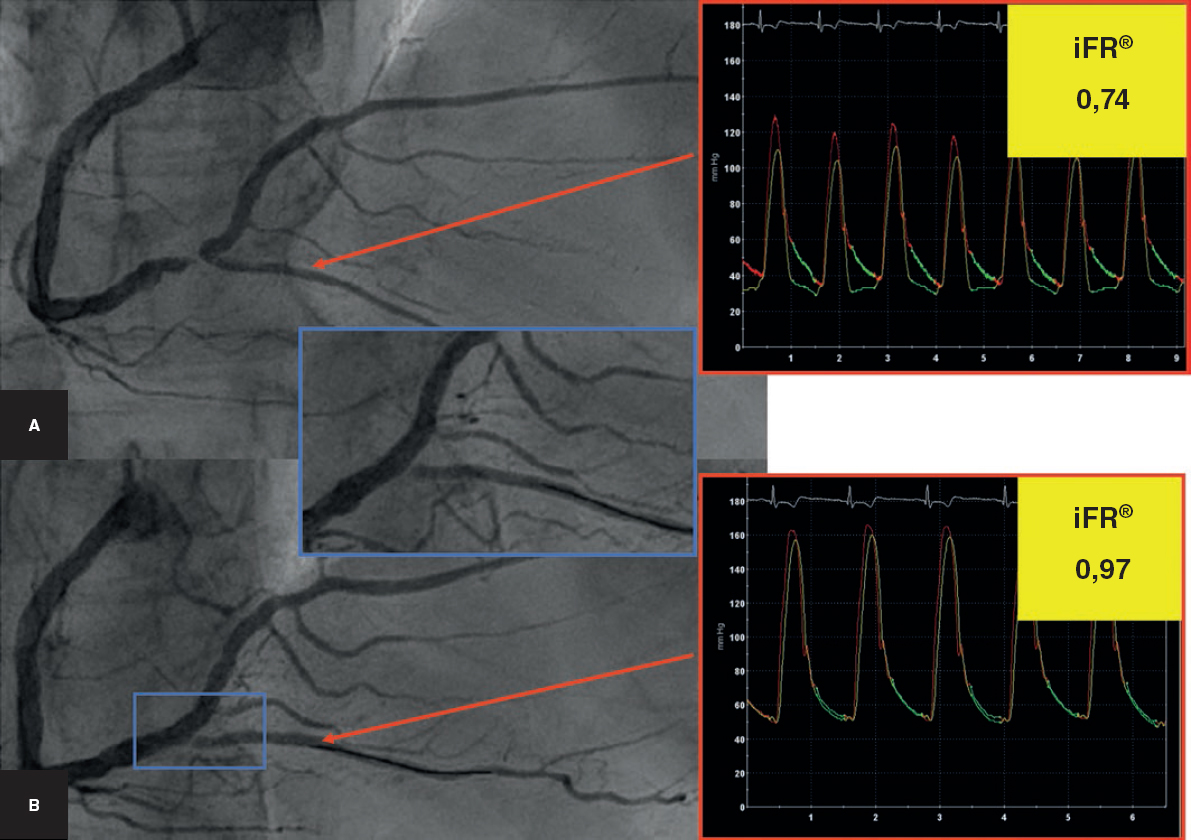
Study of coronary physiology in bifurcation lesions
The indices of coronary physiology have proven useful in the assessment of angiographically intermediate lesions. They have specifically been used in bifurcated lesions to assess the outcomes of the SB when using the provisional stenting technique. In this situation, the angiography is very much limited to assess the outcomes in a dissected segment after balloon dilation. Proof of this is the great variability of crossing to a second stent in the aforementioned different series published by the medical literature. Fractional flow reserve is used here as an interesting source of information versus the angiography. Therefore, apparently poor angiographic findings show fractional reserve flow values above the cut-off value for treatment.50 The arrival of new indices for the physiological assessment of coronary lesions opens a new field for the study of bifurcation lesions. The diastolic instantaneous wave-free ratio (iFR), an easy to obtain index that does not require the injection of adenosine, is promising for assessing the outcomes of the SB while using the provisional stenting technique51 (figure 8).
Figure 8. Monitoring of the outcome on the side branch (posterior descending artery) using the diastolic instantaneous wave-free ratio (iFR) diagnostic tool. A: baseline angiography. B: after the implantation of the stent into the main branch (right coronary artery). Angiographic compromise of the origin of the posterior descending artery with iFR values > 0.90, which is why further dilation will not be necessary.
CONCLUSIONS
The percutaneous management of coronary bifurcation lesions has changed dramatically over the last 20 years and the same thing has happened with the percutaneous management of non- bifurcated lesions. Significant advances have been made and strategies have been systematized for the management of most of these lesions. However, there are still some issued that we will have to solve in the years to come.
CONFLICTS OF INTEREST
M. Pan received minor payments for his contributions or consulting jobs for Abbott, Terumo, and Philips. S. Ojeda has received minor payments for her presentations for Terumo, and Philips. A. Lostalo declared no conflicts of interest whatsoever.
REFERENCES
1. Thomas M, Hildick-Smith D, Louvard Y, et al. Percutaneous coronary intervention for bifurcation disease. A consensus view from the first meeting of the European Bifurcation Club. EuroIntervention. 2006;2:149-153.
2. Lassen JF, Burzotta F, Banning AP, et al. Percutaneous coronary inte rvention for the left main stem and other bifurcation lesions:12th consensus document from the European Bifurcation Club. EuroIntervention. 2018;13:1540-1553.
3. Burzotta F, Lassen JF, Banning AP, et al. Percutaneous coronary intervention in left main coronary artery disease:the 13th consensus document from the European Bifurcation Club. EuroIntervention. 2018;14:112-120.
4. Caputo RP, Chafizadeh ER, Stoler RC, et al. Stent jail:a minimum-security prison. Am J Cardiol. 1996;77:1226-1229.
5. Louvard Y, Medina A. Definitions and classifications of bifurcation lesions and treatment. EuroIntervention. 2015;11:V23-V26.
6. Medina A, Suárez de Lezo J, Pan M. A new classification of coronary bifurcation lesions. Rev Esp Cardiol. 2006;59:183.
7. Louvard Y, Thomas M, Dzavik V, et al. Classification of coronary artery bifurcation lesions and treatments:time for a consensus!Catheter Cardiovasc Interv. 2008;71:175-183.
8. Pan M, Medina A, Suárez de Lezo J, et al. Coronary bifurcation lesions treated with simple approach (from the Cordoba &Las Palmas [CORPAL] Kiss Trial). Am J Cardiol. 2011;107:1460-1465.
9. Pan M, Romero M, Ojeda S, et al. Inverted crush technique for uncrossable side branch occlusion during provisional side branch stenting:a new role for the jailed wire. Rev Esp Cardiol. 2011;64:718-722.
10. Pan M, Ojeda S, Villanueva E, et al. Structural Damage of Jailed Guidewire During the Treatment of Coronary Bifurcation Lesions:A Microscopic Randomized Trial. JACC Cardiovasc Interv. 2016;9:1917-1924.
11. Owens CG, Spence MS. How should I treat a patient to remove a fractured jailed side branch wire?EuroIntervention. 2011;7:520-527.
12. Sezgin AT, Gullu H, Ermis N. Guidewire entrapment during jailed wire technique. J Invasive Cardiol. 2006;18:391-392.
13. Döring V, Hamm C. Delayed surgical removal of a guide-wire fragment following coronary angioplasty. Thorac Cardiovasc Surg. 1990;38:36-37.
14. Burns AT, Gutman J, Whitbourn R. Side-branch wire entrapment during bifurcation PCI:avoidance and management. Catheter Cardiovasc Interv. 2010;75:351-353.
15. Louvard Y, Lefevre T, Morice M-C. Percutaneous coronary intervention for bifurcation coronary disease. Heart. 2004;90:713-722.
16. Latib A, Colombo A. Bifurcation disease. What do we know, what should we do?JACC Cardiovasc Interv. 2008;1:218-226.
17. Stankovic G, Darremont O, Ferenc M, et al. Percutaneous coronary intervention for bifurcation lesions:2008 consensus document from the fourth meeting of the European Bifurcation Club. EuroIntervention. 2009;5:39-49.
18. Lefèvre T, Darremont O, Albiero R. Provisional side branch stenting for the treatment of bifurcation lesions. EuroIntervention. 2010;6:J65-J71.
19. Pan M, Medina A, Romero M, et al. Assessment of side branch predilation before a provisional T-stent strategy for bifurcation lesions. A randomized trial. Am Heart J. 2014;168:374-380.
20. Song PS, Song YB, Yang JH, et al. The impact of side branch predilatation on procedural and long-term clinical outcomes in coronary bifurcation lesions treated by the provisional approach. Rev Esp Cardiol. 2014;67:804-812.
21. Lee SH, Song YB, Lee JM, et al. Effect of Side Branch Predilation in Coronary Bifurcation Stenting With the Provisional Approach - Results From the COBIS (Coronary Bifurcation Stenting) II Registry. Circ J. 2018;82:1293-1301.
22. Burzotta F, Shoeib O, Aurigemma C, et al. Procedural Impact of a Kissing-Balloon Predilation (Pre-Kissing) Technique in Patients With Complex Bifurcations Undergoing Drug-Eluting Stenting. J Invasive Cardiol. 2019;31:80-88.
23. Ojeda S, Pan M, Mazuelos F, et al. Use of the venture wire-control catheter for accessing side branches during provisional stenting:an option for bifurcations with an unfavorable anatomy. Rev Esp Cardiol. 2010;63:1487-1491.
24. Burzotta F, De Vita M, Sgueglia G, Todaro D, Trani C. How to solve difficult side branch access?EuroIntervention. 2010;6:J72-J80.
25. Chen SL, Zhang JJ, Han Y, et al. Double Kissing Crush Versus Provisional Stenting for Left Main Distal Bifurcation Lesions:DKCRUSH-V Randomized Trial. J Am Coll Cardiol. 2017;70:2605-2617.
26. Pan M, Suárez de Lezo J, Medina A, et al. Simple and complex stent strategies for bifurcated coronary arterial stenosis involving the side branch origin. Am J Cardiol. 1999;83:1320-1325.
27. Pan M, de Lezo JS, Medina A, et al. Rapamycin-eluting stents for the treatment of bifurcated coronary lesions:a randomized comparison of a simple versus complex strategy. Am Heart J. 2004;148:857-864.
28. Colombo A, Moses JW, Morice MC, et al. Randomized study to evaluate sirolimus-eluting stents implanted at coronary bifurcation lesions. Circulation. 2004;109:1244-1249.
29. Steigen TK, Maeng M, Wiseth R, et al. Randomized study on simple versus complex stenting of coronary artery bifurcation lesions:the Nordic bifurcation study. Circulation. 2006;114:1955-1961.
30. Ferenc M, Gick M, Kienzle RP, et al. Randomized trial on routine vs. T-stenting in the treatment of de novo coronary bifurcation lesions. Eur Heart J. 2008;29:2859-2867.
31. Colombo A, Bramucci E, SaccàS, et al. Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations:the CACTUS (Coronary Bifurcations:Application of the Crushing Technique Using Sirolimus-Eluting Stents) Study. Circulation. 2009;119:71-78.
32. Hildick-Smith D, de Belder AJ, Cooter N, et al. Randomized trial of simple versus complex drug-eluting stenting for bifurcation lesions:the British Bifurcation Coronary Study:old, new, and evolving strategies. Circulation. 2010;121:1235-1243.
33. Zhang F, Dong L, Ge J. Simple versus complex stenting strategy for coronary artery bifurcation lesions in the drug-eluting stent era:a meta-analysis of randomised trials. Heart. 2009;95:1676-1681.
34. Hakeem A, Khan FM, Bhatti S, et al. Provisional vs complex stenting strategy for coronary bifurcation lesions:Meta-analysis of randomized trials. J Invasive Cardiol. 2009;21:589-595.
35. Katritsis DG, Siontis GC, Ioannidis JP. Double versus single stenting for coronary bifurcation lesions. A meta-analysis. Cir Cardiovasc Intervent. 2009;2:409-415.
36. Brar SS, Gray WA, Dangas G, et al. Bifurcation stenting with drug-eluting stents:a systematic review and meta-analysis of randomised trials. EuroIntervention. 2009;5:475-484.
37. Heras M, Avanzas P, Bayes-Genis A, Pan M, Pérez de Isla L, Sanchis J. Unplanned redundant publications:a consequence of too many cardiovascular journals?EuroIntervention 2010;6:179-181.
38. Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40:87-165.
39. Chen SL, Santoso T, Zhang JJ, et al. A randomized clinical study comparing double kissing crush with provisional stenting for treatment of coronary bifurcation lesions:results from the DKCRUSH-II (Double Kissing Crush versus Provisional Stenting Technique for Treatment of Coronary Bifurcation Lesions) trial. J Am Coll Cardiol. 2011;57:914-920.
40. Pan M, Suárez de Lezo J, Medina A, et al. Drug-eluting stents for the treatment of bifurcation lesions:a randomized comparison between paclitaxel and sirolimus stents. Am Heart J. 2007;153:15.1-7.
41. Ojeda S, Pan M, Gutiérrez A, et al. Bifurcation lesions involved in the recanalization process of coronary chronic total occlusions:Incidence, treatment and clinical implications. Int J Cardiol. 2017;230:432-438.
42. Ojeda S, Azzalini L, Chavarria J, et al. One Versus 2-stent Strategy for the Treatment of Bifurcation Lesions in the Context of a Coronary Chronic Total Occlusion. A Multicenter Registry. Rev Esp Cardiol. 2018;71:432-439.
43. Ojeda S, Pan M, Martín P, et al. Immediate results and long-term clinical outcome of patients with unprotected distal left main restenosis:the CORPAL registry (Córdoba and Las Palmas). JACC Cardiovasc Interv. 2014;7:212-221.
44. Mintz GS, Lefèvre T, Lassen JF, et al. Intravascular ultrasound in the evaluation and treatment of left main coronary artery disease:a consensus statement from the European Bifurcation Club. EuroIntervention. 2018;14:467-474.
45. Medina A, Martín P, Suárez de Lezo J, et al. Vulnerable carina anatomy and ostial lesions in the left anterior descending coronary artery after floating-stent treatment. Rev Esp Cardiol. 2009;62:1240-1249.
46. Suárez de Lezo J, Medina A, Martín P, et al. Predictors of ostial side branch damage during provisional stenting of coronary bifurcation lesions not involving the side branch origin:an ultrasonographic study. EuroIntervention. 2012;7:1147-1154.
47. Pan M, Suárez de Lezo J, Medina A, et al. Resultados del tratamiento de las lesiones en bifurcación con stents farmacoactivos. Papel de la ecografía intracoronaria. Rev Esp Cardiol Supl. 2007;7(E):49-56.
48. Lezo JS, Medina A, Martín P, et al. Ultrasound findings during percutaneous treatment of bifurcated coronary lesions. Rev Esp Cardiol. 2008;61:930-935.
49. Onuma Y, Katagiri Y, Burzotta F, et al. Joint consensus on the use of OCT in coronary bifurcation lesions by the European and Japanese bifurcation clubs. EuroIntervention. 2019;14:1568-1577.
50. Koo BK, Waseda K, Kang HJ, et al. Anatomic and functional evaluation of bifurcation lesions undergoing percutaneous coronary intervention. Circ Cardiovasc Interv. 2010;3:113-119.
51. Hidalgo F, Pan M, Ojeda S, et al. Feasibility and Efficacy of the Jailed Pressure Wire Technique for Coronary Bifurcation Lesions. JACC Cardiovasc Interv. 2019;12:109-111.