QUESTION: Although we will discuss the aspects of 2 plaque modification techniques, please explain when you resort to intravascular imaging modalities in cases of calcified lesions and how that helps you.
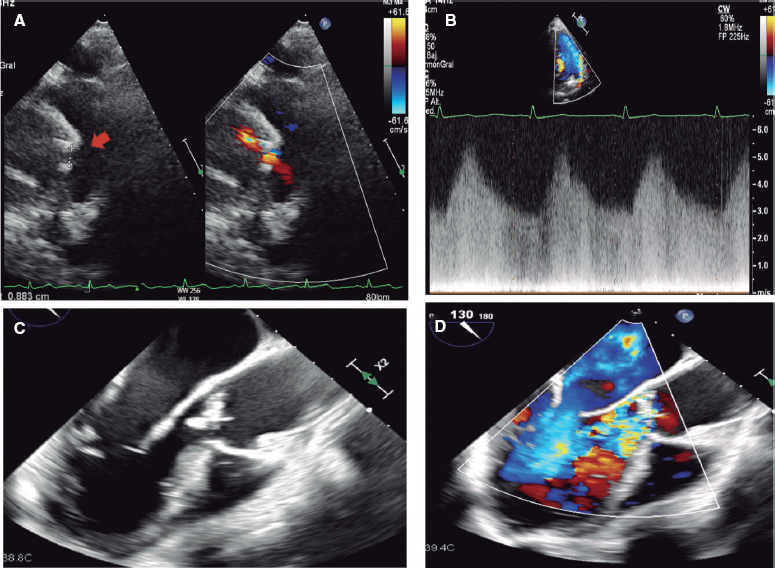
ANSWER: Intracoronary imaging modalities (optical coherence tomography [OCT] and intravascular ultrasound [IVUS]) allow us to optimize percutaneous coronary interventions, and their use in complex lesions improves the patient’s prognosis.1 They facilitate the following aspects:2
- – Calcification detection and assessment: they have higher sensitivity and specificity than angiography for detecting calcium.3 Also, they allow the evaluation of calcification characteristics, and various scores4,5 have been developed that integrate variables associated with stent underexpansion.
- – Selection of plaque modification technique: intracoronary imaging findings have an impact on the strategy used, which is why the use of advanced imaging modalities is advised in the presence of risk criteria for stent underexpansion.2
- – Optimization of stent deployment: this is especially relevant in calcified lesions, which are the lesions most frequently associated with stent underexpansion, the parameter most often associated with stent failure.2 Other parameters that should also be assessed are proper stent apposition, lesion coverage, the absence of dissection, and significant hematoma around the edges.6
Q.: In your opinion, what are the advantages and disadvantages of ablation, whether rotational or orbital?
A.: Ablation therapies, such as rotational atherectomy (RA), or orbital atherectomy (OA), and Excimer laser coronary angioplasty (ELCA), offer several advantages over intracoronary lithotripsy (ICL):
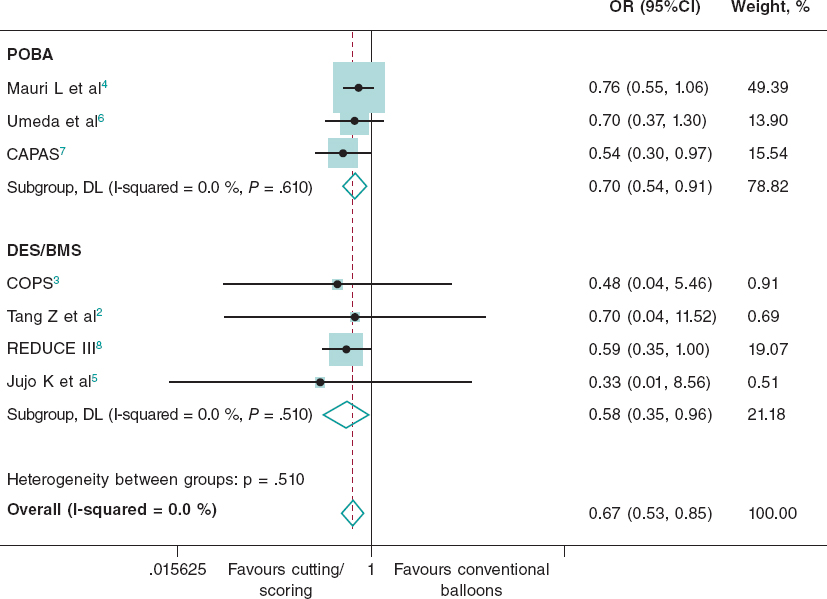
- – Greater crossing ability: calcified lesions that result in very severe stenosis can be uncrossable with a balloon. In these lesions, the use of ablation techniques improves the rate of procedural success,7,8 and probably, costs and safety.
- – Ability to reduce plaque volume: an aspect that can be essential to optimize results.
- – Treatment of long lesions and multivessel disease: ICL balloons are short in length, and display a maximum of 120 pulses per balloon. Also, balloons should be sized in a 1:1 ratio with respect to the vessel diameter, which complicates their use in multiple lesions. With RA, and especially with OA and ELCA, we can safely and effectively treat segments of different calibers without increasing costs.
- The potential disadvantages of ablation therapies are:
- – A longer learning curve: despite having specific technical aspects, ICL does not significantly differ from the plain old balloon angioplasty. Consequently, since it became available, the use of ICL has grown exponentially.9 Ablation techniques require more operator (and nursing) training, which can limit their use.
- – Need for specific angioplasty guidewires: ELCA can be used with 0.014-inch angioplasty guidewires, but both RA and OA require specific guidewires, whose characteristics have been improved to allow their use throughout the entire procedure, as with conventional guidewires. However, they can lead to more difficulties in directly crossing lesions and make the procedure more cumbersome due to their greater length and lower support.
- – Side branch protection: although it can be performed using specific techniques, placing a side branch protection guidewire at a bifurcation during RA or OA is ill-advised. However, this is possible with ICL and ELCA.
- – Distal embolization: debris following the use of ablation techniques can be associated with slow-no reflow.
Q.: In which cases do you use ablation as a first-line approach? Are there any distinctions between rotational and orbital atherectomies?
A.: We usually use these techniques as the first-line approach in lesions so severely stenosed that they complicate balloon crossing or simply make it impossible (uncrossable lesions). The information provided by intracoronary imaging also plays a role in the decision to use ablation techniques as the first option. For some operators, the mere fact of being unable to cross the lesion with an IVUS or OCT probe is, per se, a criterion for using these ablation techniques. If intracoronary images are available, the presence of severity criteria, or the desire to reduce plaque volume encourages the use of advanced plaque modification therapies. Superficial concentric calcification with a very reduced luminal area would favor their use.
In terms of the differences among ablation techniques, in my opinion, the crossing ability of RA and ELCA is superior to that of OA, which therefore makes RA the preferred option to treat critical or uncrossable lesions. On the other hand, OA provides additional advantages over RA.2,10 In the first place, we can treat vessels from 2.5 mm to 4 mm due to its mechanism of action (rotation associated with elliptical orbits) with a single 1.25 mm crown (compatible with 6-Fr) without increasing the size of the guide catheter. Also, the elliptical motion of this crown not only allows for superficial calcium shaving (like RA), but also exerts pulsatile forces against the wall that can modify deeper calcium deposits.10,11 This orbital movement reduces wire bias compared with AR. Wire bias limits ablation, which is contact-dependent, to the vessel sector where the guide is located. In eccentric or nodular plaques, the guidewire may be displaced toward the opposite side of the vessel, thus minimizing the effect of RA on the plaque. Another interesting feature of OA is that the crown has a diamond coating across its entire surface (not just on the distal end, like RA crowns), allowing atherectomy to make forward and backward motions. The pullback mode modifies the ablation vector, potentially reducing wire bias even further. Furthermore, the debris produced by OA is theoretically smaller than those produced by RA. This, along with the fact that the crown does not impede coronary flow during atherectomy, reduces the risk of slow-no reflow and endothelial thermal injury.10
The main difference among ELCA, RA, and OA is that the former is the only ablation technique that is compatible with conventional coronary guidewires. Also, ELCA is compatible with 6-Fr guide catheters and allows for side branch protection. Also, it has beneficial effects in reducing thrombus and has proven to be safe and effective in peristent calcified lesions (restenosis or underexpansion).
Q.: Which calcified lesions benefit more from ablation compared with intracoronary lithotripsy?
A.: The calcified lesions that benefit the most from initial ablation rather than ICL are the most severely stenotic lesions, which are rarely crossable with a lithotripsy balloon as a first-line approach, and those with a large volume of plaque that we intend to reduce. Ablation techniques facilitate crossing these stenoses and are sufficient in many cases (when calcification is superficial, without significant thickness, and when calcified nodules are not involved) to allow adequate balloon or stent expansion, and complete the angioplasty. In addition, diffuse lesions in multiple segments, or vessels of different calibers can benefit more from ablation because they can be treated with a single RA, AO, or ELCA catheter.
Finally, although ICL can be safely performed in left main lesions, some patients (especially those with ventricular dysfunction or right coronary artery disease) can tolerate prolonged ICL balloon inflations poorly, and benefit from ablation techniques as a first option.
Q.: How do you integrate both ablation techniques into your protocol to treat calcified lesions?
A.: There are several algorithms for plaque modification techniques based on expert opinion. Evidence from comparative trials among the various techniques is scarce. Although randomized clinical trials are under way,12 the lesion characteristics, clinical context, available resources, and operator capabilities should always be taken into consideration.
Intracoronary imaging modalities are essential to select the strategy. In general, it is useful to apply the rule of 5N:2 advanced plaque modification techniques are advised to treat lesions where calcium occupies > 50% of the calcium arc (180°), extends longitudinally > 5 mm, is > 0.5 mm thick, or has calcified nodules. Additionally, the depth of calcium is important since some techniques, such as RA, can only modify superficial calcium.
Lesions that cause stenosis so severe that they cannot be crossed by IVUS or OCT probes will likely require RA, OA, or ELCA. RA may be the preferred choice for very stenotic lesions with superficial circumferential calcification, especially if they are uncrossable with a balloon and involve a nontortuous coronary segment. OA may be preferred to treat ostial, nodular lesions, or angulated segments. OA can also be useful in long lesions with significantly different proximal and distal vessel calibers. ELCA would be the preferred choice in lesions that cannot be crossed even with a microcatheter that allows exchange with RA or OA-specific guidewires. Also, ELCA could be the first option to treat peristent calcified lesions and those that combine calcium and thrombus.
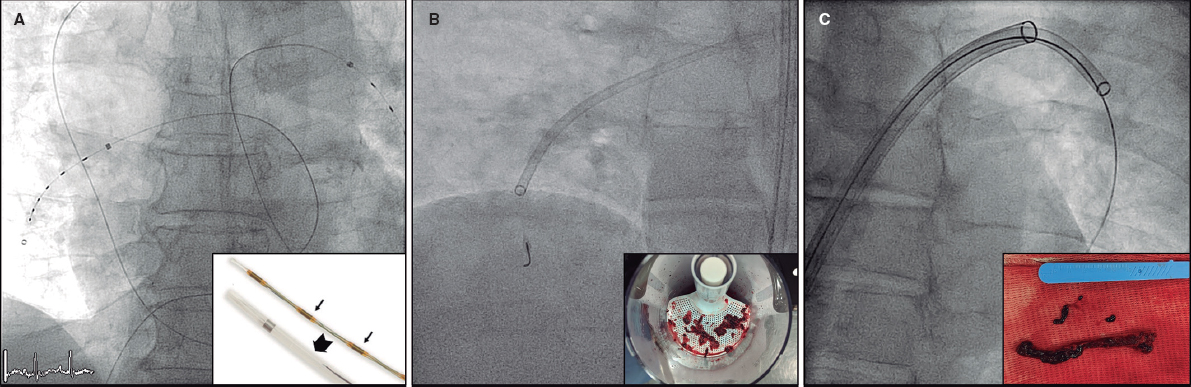
ICL has the advantage of being a simpler technique and being able to modify deep calcium. ICL allows side branch protection without causing distal embolization of material. ICL can be the first choice if the lesion is crossable with a balloon, calcification is deep or thick, or it affects a true bifurcation. Additionally, ICL is an optimal technique for use in combination with ablation techniques when these do not allow adequate balloon expansion, or in complex lesions such as calcium nodules. Volume reduction and superficial calcium shaving with ablation techniques allows balloon ICL crossing. This completes plaque modification by fracturing deeper calcium deposits. This technique, initially described as rotatripsy13 (RA and ICL), is increasingly being used. Combinations of ELCA and ICL,14 or OA and ICL15 are less common, but have also been reported.
FUNDING
None declared.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCE
Artificial intelligence was not used in the preparation of this article.
CONFLICTS OF INTEREST
A. Jurado-Román is a proctor for Boston Scientific, Cardiovascular Systems, Inc., World Medica, and Philips-Biomenco.
REFERENCES
1. Lee JM, Choi KH, Song YB, et al. Intravascular Imaging–Guided or Angiography-Guided Complex PCI. N Engl J Med.2023;388:1668-1679.
2. Jurado-Román A, Gómez-Menchero A, Gonzalo N, et al. Plaque modification techniques to treat calcified coronary lesions. Position paper from the ACI-SEC. REC Interv Cardiol. 2023;5:46-61.
3. Wang X, Matsumura M, Mintz GS, et al. In Vivo Calcium Detection by Comparing Optical Coherence Tomography, Intravascular Ultrasound, and Angiography. JACC Cardiovasc Imaging. 2017;10:869-879.
4. Fujino A, Mintz GS, Matsumura M, et al. A new optical coherence tomography-based calcium scoring system to predict stent underexpansion. EuroIntervention. 2018;13:e2182-e2189.
5. Zhang M, Matsumura M, Usui E, et al. Intravascular Ultrasound-Derived Calcium Score to Predict Stent Expansion in Severely Calcified Lesions. Circ Cardiovasc Interv. 2021;14:e010296.
6. Räber L, Mintz GS, Koskinas KC, et al. Clinical use of intracoronary imaging. Part 1:guidance and optimization of coronary interventions. An expert consensus document of the European Association of Percutaneous Cardiovascular Interventions. EuroIntervention. 2018;14:656-677.
7. Abdel-Wahab M, Richardt G, Joachim Büttner H, et al. High-speed rotational atherectomy before paclitaxel-eluting stent implantation in complex calcified coronary lesions:the randomized ROTAXUS (Rotational Atherectomy Prior to Taxus Stent Treatment for Complex Native Coronary Artery Disease) trial. JACC Cardiovasc Interv. 2013;6:10-19.
8. Abdel-Wahab M, Toelg R, Byrne RA, et al. High-Speed Rotational Atherectomy Versus Modified Balloons Prior to Drug-Eluting Stent Implantation in Severely Calcified Coronary Lesions. Circ Cardiovasc Interv. 2018;11:e007415.
9. Jurado-Román A, Freixa X, Cid B, et al. Spanish cardiac catheterization and coronary intervention registry. 32nd official report of the Interventional Cardiology Association of the Spanish Society of Cardiology (1990-2022). Rev Esp Cardiol. 2023;76(12):1021-1031.
10. Yamamoto MH, Maehara A, Karimi Galougahi K, et al. Mechanisms of Orbital Versus Rotational Atherectomy Plaque Modification in Severely Calcified Lesions Assessed by Optical Coherence Tomography. JACC Cardiovasc Interv. 2017;10:2584-2586.
11. Yamamoto MH, Maehara A, Kim SS, et al. Effect of orbital atherectomy in calcified coronary artery lesions as assessed by optical coherence tomography. Catheter Cardiovasc Interv. 2019;93:1211-1218.
12. Jurado-Román A, Gómez-Menchero A, Amat-Santos IJ, et al. Design of the ROLLERCOASTR trial:rotational atherectomy, lithotripsy or laser for the management of calcified coronary stenosis. REC Interv Cardiol. 2023;5:279-286.
13. Jurado-Román A, Gonzálvez A, Galeote G, et al. RotaTripsy:Combination of Rotational Atherectomy and Intravascular Lithotripsy for the Treatment of Severely Calcified Lesions. JACC Cardiovasc Interv. 2019;12:e127-e129.
14. Jurado-Román A, García A, Moreno R. ELCA-Tripsy:Combination of Laser and Lithotripsy for Severely Calcified Lesions. J Invasive Cardiol. 2021;33:E754-E755.
15. Yarusi BB, Jagadeesan VS, Hussain S, et al. Combined Coronary Orbital Atherectomy and Intravascular Lithotripsy for the Treatment of Severely Calcified Coronary Stenoses:The First Case Series. J Invasive Cardiol. 2022;34:E210-E217.