To the Editor,
Calcified coronary lesions remain a procedural and clinical challenge associated with higher rates of procedural complications such as stent underexpansion and malapposition leading to an increased risk of target lesion revascularization (TLR), stent thrombosis, myocardial infarction (MI), and death.1 While newer drug-eluting stents and advanced devices are considered safer and more effective, there is still a need for atherosclerotic plaque modification techniques that allow for adequate stent expansion and apposition when traditional techniques fail. Cutting and scoring balloons have been designed to treat complex lesions such as fibrotic plaque and calcified lesions.2,3 However, their use may have been limited by problems of crossability and limited evidence supporting their efficacy and safety.4 In addition, the available published literature is based on studies with noninferiority designs and small sample sizes,5 which may not provide adequately powered analyses to evaluate the clinical efficacy of cutting and scoring balloons in patients with native-vessel coronary artery disease (CAD). Therefore, we performed a systematic review and meta-analysis to compare cutting and scoring balloons with conventional balloons (semi- and non-compliant balloons) in patients with native vessel CAD.
This meta-analysis was conducted according to the PRISMA guidelines for the reporting of systematic reviews. Two reviewers independently identified relevant studies through an electronic search of the MEDLINE, Embase, Cochrane Central Register of Controlled Trials, and ClinicalTrials.gov databases (from inception to June 2023). Abstracts presented at major scientific conferences (American Heart Association, American College of Cardiology, European Society of Cardiology, EuroPCR, and Transcatheter Cardiovascular Therapeutics) were also reviewed. We also used backward snowballing (review of literature references within identified articles and relevant reviews). Inclusion criteria were: a) randomized controlled trials comparing percutaneous coronary intervention with cutting or scoring balloons with semi- or noncompliant balloons; b) study population including patients with native vessel CAD; c) the availability of clinical outcome data. This trial is registered with PROSPERO (CRD42023434007).
The primary endpoint was TLR. Secondary outcomes included MI, vessel perforation, and all-cause death.
Odds ratios (ORs) and 95% confidence intervals (95%CI) were calculated using the DerSimonian and Laird random effects model, and heterogeneity was estimated using the Mantel-Haenszel method. The presence of heterogeneity among studies was assessed using the Cochran Q chi-square test, and the I-squared test was used to assess inconsistency. A random-effects meta-regression analysis using the empirical Bayes method (Paule-Mandel) was performed to assess the interaction of percentage of drug-eluting stent (DES) use, percentage of intravascular ultrasound use, diabetes mellitus, and sex on treatment effects. We performed a subgroup analysis for the primary endpoint according to revascularization strategy (stent implantation or plain old balloon angioplasty [POBA]). The statistical significance level was 2-tailed P < .05.
A total of 1090 citations were screened and 8 studies with 2712 patients and a mean follow-up of 6.6 months were finally included.2-8 Of the 8 studies, 2 included only calcified lesions,2,3 while the remaining 6 included de novo lesions regardless of the severity of coronary calcification.4-8 In addition, 4 studies used POBA as definitive therapy.4-7 In all, 24.6% of patients were female, with a mean age of 61.6 years, of which 34.8% had a history of acute coronary syndrome. The most commonly treated artery was the left anterior descending artery (42.4%), and the mean vessel diameter of the target lesion was 2.8 mm. Intracoronary imaging was used in 18.8% of patients.
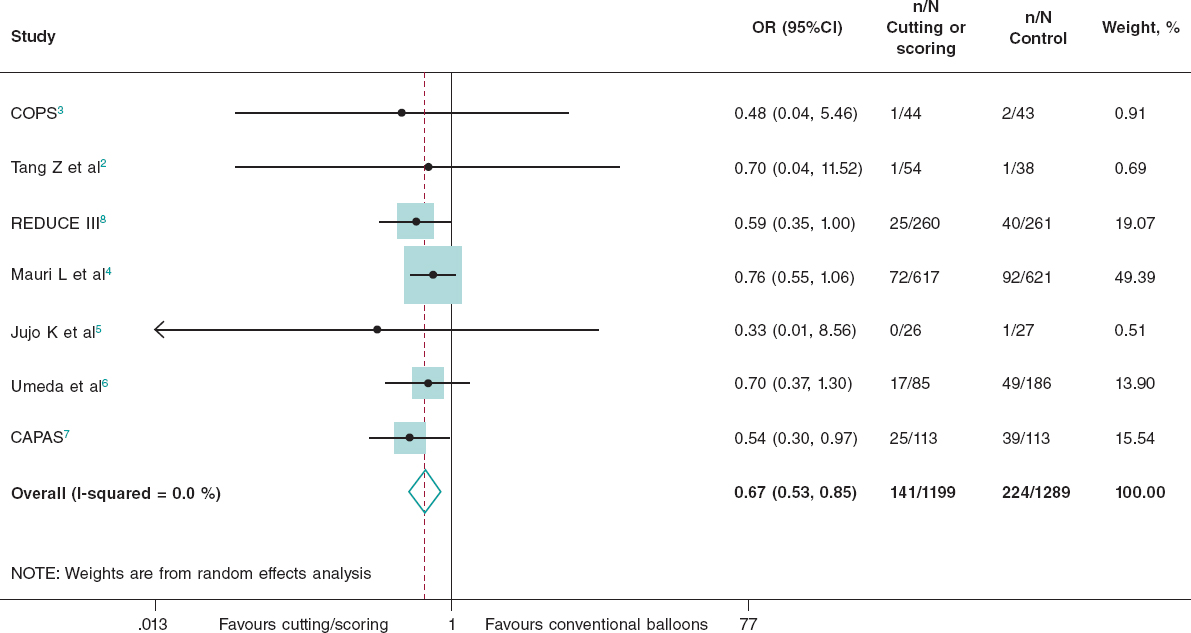
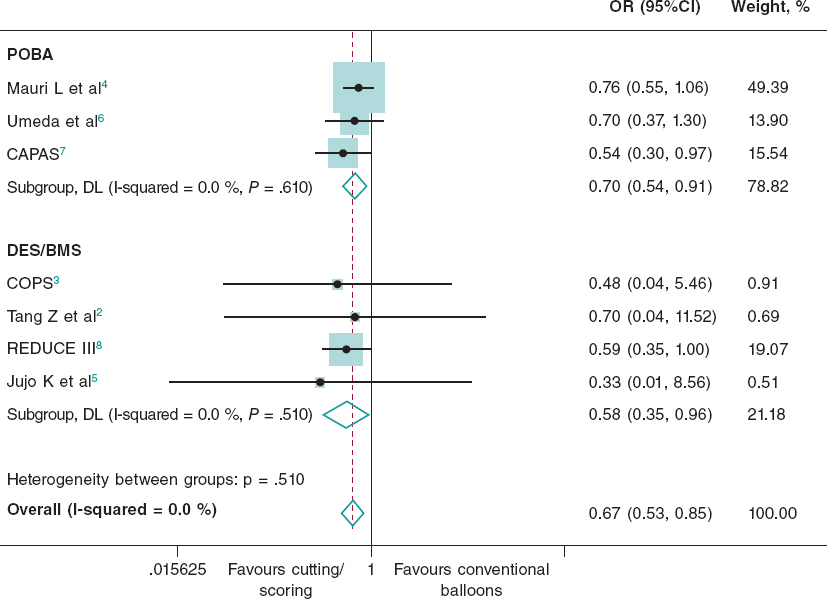
The use of cutting/scoring balloons was associated with a lower risk of TLR than that of conventional balloons (OR, 0.67; 95%CI, 0.53-0.85; I-squared, 0%) (figure 1). There were no differences between groups in the risk of all-cause death (OR, 1.31; 95%CI, 0.53-3.21; I-squared, 0%), MI (OR, 1.22; 95%CI, 0.48-3.08; I-squared, 50.1%), or vessel perforation (OR, 1.68; 95%CI, 0.37-7.74; I-squared, 0%). No significant effects were found for diabetes (P = .337), sex (P = .896), the percentage of intravascular ultrasound (P = .178), or the percentage of DES implantation (P = .721) on treatment effects. Our results remained consistent with the primary analysis after stratification by revascularization strategy (stenting or POBA) (figure 2).
Figure 1. Forest plot reporting trial-specific and summary OR with 95%CI for the primary endpoint of target lesion revascularization. 95%CI, 95% confidence interval; CAPAS, Cutting balloon angioplasty vs plain old balloon angioplasty randomized study in type B/C lesions; COPS, Cutting balloon to optimize predilatation for stent implantation; OR, odds ratio; REDUCE, Restenosis reduction by cutting balloon angioplasty evaluation.
Figure 2. Subgroup analysis according to the revascularization strategy (stent implantation or plain old balloon angioplasty [POBA]) for the primary endpoint of target lesion revascularization. 95%CI, 95% confidence interval; BMS, bare metal stent; CAPAS, Cutting balloon angioplasty vs plain old balloon angioplasty randomized study in type B/C lesions; COPS, Cutting balloon to optimize predilatation for stent implantation; DES, drug eluting stent; OR, odds ratio; REDUCE, Restenosis reduction by cutting balloon angioplasty evaluation; POBA, percutaneous old balloon angioplasty.
The present study provides the first critical analysis of the available evidence on the use of cutting and scoring balloons in patients with native-vessel CAD. The use of cutting/scoring balloons was associated with a lower risk of TLR without an increased risk of clinical adverse events compared with conventional balloons. This benefit may be explained by the improved lesion preparation achieved with the use of cutting/scoring balloons. In addition, cutting/scoring balloons create discrete longitudinal incisions in the atherosclerotic target coronary segment, which may enhance drug diffusion and penetration into the arterial wall. Interestingly, a recent meta-analysis showed no significant differences in clinical or imaging outcomes in patients treated with cutting balloons compared with other techniques, including the same risk of repeat revascularization.9 However, there are relevant differences with respect to this study that may explain the different outcomes: a) only patients with severely calcified lesions were included; b) studies comparing or combining cutting balloons with techniques such as rotational atherectomy or very high pressure balloons were included; and c) stent implantation was performed in all studies.
However, the present study should be interpreted in the light of several limitations. First, the lack of patient-level data prevented us from assessing the impact of baseline clinical characteristics (ie, degree of coronary calcification) on treatment effects. Second, some of the included older studies compared cutting/scoring balloon with POBA without stent implantation, which is not a contemporary strategy. Nevertheless, we found no effect of the percentage of DES implantation on treatment effects in the meta-regression analysis.
FUNDING
None.
ETHICAL CONSIDERATIONS
Ethics approval was not required for this meta-analysis as all data were collected and synthesized from previous studies and no informed consent was required as there were no patients involved in our work. The meta-analysis of RCTs was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2009 guidelines. We confirm that sex/gender biases have been taken into acount.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCE
No artificial intelligence software has been used.
AUTHORS’ CONTRIBUTIONS
J.A. Sorolla Romero, J. Martínez Solé, A. Teira Calderón, M. Calvo Asensio and J. Sanz Sánchez contributed to the idea, design, drafting, and revision of the article. J.L. Díez Gil contributed to the critical revision of the intellectual content.
CONFLICTS OF INTEREST
None.
REFERENCES
1. Angsubhakorn N, Kang N, Fearon C, et al. Contemporary Management of Severely Calcified Coronary Lesions. J Pers Med. 2022;12:1638.
2. Tang Z, Bai J, Su SP, et al. Cutting-balloon angioplasty before drug-eluting stent implantation for the treatment of severely calcified coronary lesions. J Geriatr Cardiol. 2014;11:44-49.
3. Mangieri A, Nerla R, Castriota F, et al. Cutting balloon to optimize predilation for stent implantation:The COPS randomized trial. Catheter Cardiovasc Interv. 2023;101:798-805.
4. Mauri L, Bonan R, Weiner BH, et al. Cutting balloon angioplasty for the prevention of restenosis:results of the Cutting Balloon Global Randomized Trial. Am J Cardiol. 2002;90:1079-1083.
5. Jujo K, Saito K, Ishida I, et al. Intimal disruption affects drug-eluting cobalt-chromium stent expansion:A randomized trial comparing scoring and conventional balloon predilation. Int J Cardiol. 2016;221:23-31.
6. Umeda H, Iwase M, Kanda H, et al. Promising efficacy of primary gradual and prolonged balloon angioplasty in small coronary arteries:a randomized comparison with cutting balloon angioplasty and conventional balloon angioplasty. Am Heart J. 2004;147:E4.
7. Izumi M, Tsuchikane E, Funamoto M, et al. Final results of the CAPAS trial. Am Heart J. 2001;142:782-789.
8. Ozaki Y, Yamaguchi T, Suzuki T, et al. Impact of cutting balloon angioplasty (CBA) prior to bare metal stenting on restenosis. Circ J. 2007;71:1-8.
9. Scalamogna M, Kuna C, Voll F, et al. Modified balloons to prepare severely calcified coronary lesions before stent implantation:a systematic review and meta-analysis of randomized trials. Clin Res Cardiol. 2024;113:995–1005.