ABSTRACT
Introduction and objectives: Noncompliant balloon postdilatation of coronary stents improves clinical results. Regular noncompliant balloons (RegNC) have less crossability and a tapered-tip that can complicate successful stent postdilatation. The mechanical conditions of a new spherical tip non-compliant balloon (SphNC) could facilitate stent postdilatation. We tried to evaluate the effectiveness of a new SphNC in the routine percutaneous coronary intervention (PCI) practice.
Methods: Prospective multicenter technical registry to assess the effectiveness of a new SphNC for stent postdilatation with 2 study arms: use of SphNC as the first choice or as the secondary choice after RegNC failure. The primary endpoint was technical success defined as advancing the SphNC across the stent segment. Secondary endpoints were angiographic success defined as technical success and residual stenosis < 30% with final TIMI grade-3 flow, and procedural success defined as angiographic success without mechanical stent complications or any perioperative major adverse cardiovascular events.
Results: The SphNC was used in 263 lesions (177 lesions as first choice, and 86 after RegNC failure) in 250 procedures. The use of the complex technique to advance the SphNC was low (9.9%). Technical, angiographic, and procedural success rates were 98.9%, 98.3%, and 98.3%, respectively, as the first choice, and 98.8%, 97.7%, and 96.5%, respectively, after RegNC failure. SphNC had similar size (3.39 mm ± 0.6 mm vs 3.34 mm ± 0.6 mm; P = nonsignificant), and shorter lengths (11 mm ± 2 mm vs 12 mm ± 3 mm; P = .005) compared to RegNC. No stent-related mechanical complications were reported.
Conclusions: SphNC for coronary stent postdilatation in the routine PCI clinical practice has a very high technical success rate as the first choice (98.9%), as well as in cases of RegNC failure (98.8% with low complex technique requirements, and a safe profile).
Keywords: Complex PCI. Stent postdilatation. Tapered-tip balloon. Spherical tip balloon.
RESUMEN
Introducción y objetivos: La posdilatación de stents coronarios con balones no distensibles mejora los resultados clínicos. Los balones no distensibles normales (RegNC) presentan peor navegabilidad y tienen una punta cónica que puede dificultar la posdilatación exitosa. Las condiciones mecánicas de un nuevo balón no distensible con punta esférica (EsfNC) podrían facilitar la posdilatación del stent. Evaluamos la efectividad del EsfNC en la posdilatación coronaria para la intervención coronaria percutánea en la práctica clínica habitual.
Métodos: Registro técnico prospectivo y multicéntrico para evaluar la efectividad de un nuevo EsfNC en posdilatación coronaria, con 2 grupos de estudio: uso de EsfNC como primera opción o uso de EsfNC ante el fracaso de RegNC. El evento primario fue el éxito técnico, definido como conseguir avanzar el EsfNC hasta el segmento que posdilatar dentro del stent. Los eventos secundarios fueron el éxito angiográfico, definido como éxito técnico junto con estenosis residual < 30% con flujo final TIMI 3, y el éxito del procedimiento, definido como éxito angiográfico sin complicación mecánica del stent ni eventos cardiovasculares mayores periprocedimiento.
Resultados: Se usó EsfNC en 263 lesiones (en 177 como primera opción y en 86 tras el fracaso de RegNC), en 250 procedimientos. Se usaron técnicas complejas para avanzar el EsfNC en el 9,9% de los procedimientos. Los porcentajes de éxito técnico, angiográfico y de procedimiento fueron del 98,9%, el 98,3% y el 98,3% como primera opción, y del 98,8%, el 97,7% y el 96,5% tras fracaso de RegNC, respectivamente. Los EsfNC tuvieron similar calibre (3,39 ± 0,6 frente a 3,34 ± 0,6 mm; p = no significativo) y longitud más corta (11 ± 2 frente a 12 ± 3 mm; p = 0,005) que los RegNC. No se comunicaron complicaciones mecánicas del stent.
Conclusiones: La posdilatación coronaria con EsfNC para la intervención coronaria percutánea en la práctica clínica habitual muestra un porcentaje muy alto de éxito técnico, tanto en primera opción (98,9%) como en casos de fracaso de RegNC (98,8%), con baja necesidad de técnicas complejas y buen perfil de seguridad.
Palabras clave: Intervención coronaria percutánea compleja. Posdilatación coronaria. Balón no distensible. Balón no distensible punta esférica.
Abbreviations
NC: noncompliant balloon. PCI: percutaneous coronary intervention. RegNC: regular noncompliant balloon. SphNC: spherical tip noncompliant balloon.
INTRODUCTION
Optimal stenting is crucial in the long-term clinical outcomes while proper stent expansion and apposition reduce the risk of thrombosis and restenosis.1 Coronary stent postdilatation increases luminal area while reducing stent strut malapposition.2,3
Unlike semicompliant balloons, noncompliant (NC) balloon postdilatation allows uniform dilatation at higher pressures, which reduces the risk of damage to the vessel wall (edge dissection or coronary perforation),4 and is associated with greater stent expansion and a lower rate of target lesion revascularization.5 Therefore, postdilatation using NC balloons is a common strategy to increase the luminal area of underexpanded stents or increase the stent proximal caliber in long lesions or in bifurcation techniques like the proximal optimization technique (POT) or the conventional kissing-balloon technique in a safe and predictable way.6,7
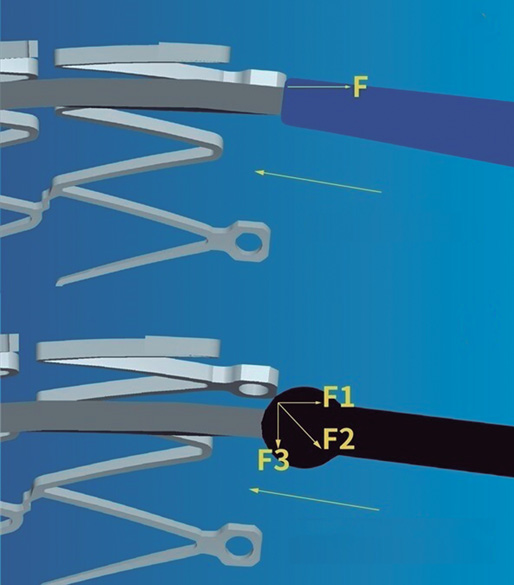
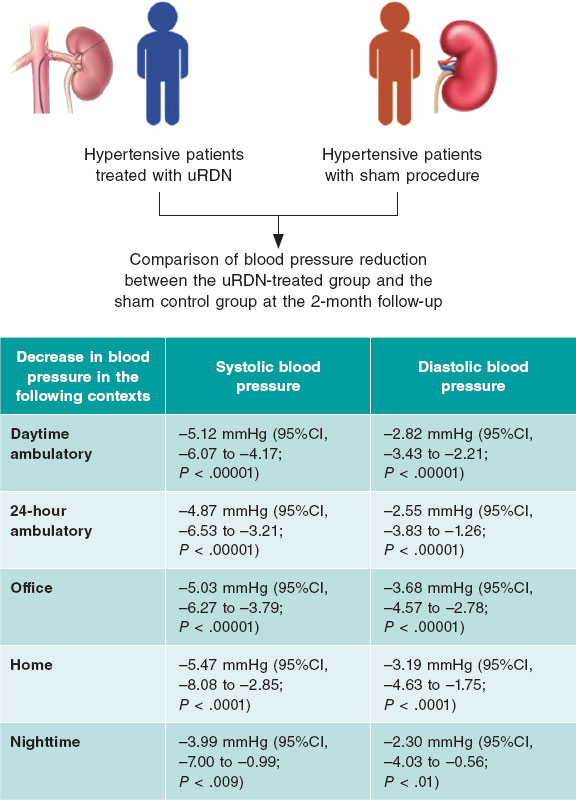
The navigability of NC balloons is more limited, a significant setback in cases of coronary tortuosity, calcified lesions or proximal stent edge malapposition. Regular noncompliant balloons (RegNC) include a cone-shaped tip that can collide with the struts or with the proximal stent edge, thus conditioning a force vector opposed to the push force that can potentially interfere with its advancement (figure 1A), and eventually lead to mechanical stent failure in cases of inadequate coaxiality. In these cases, the use of complex techniques (buddy-wire, buddy-balloon, anchoring...) or specific devices (guide catheter extension systems) are often needed to advance the balloon, which increases the cost of the procedure.
Figure 1. A: the cone-shaped tip of a regular noncompliant balloon can collide with the stent struts thus conditioning a force (F) vector opposed to the push force that can potentially interfere with its advancement. B: the spherical tip contributes to decomposing and reducing the resistance force vector opposed to the push vector, thus facilitating the balloon advancement towards the inside of the stent. Courtesy of APT Medical, China.
The cone-shaped tip has been replaced by a spherical tip in a new NC balloon (NC Conqueror Spherical tip, APT Medical, China) (SphNC). Despite its greater crossing profile (0.039 in), the spherical tip contributes to decomposing and reducing the resistance force vector opposed to the push vector (figure 1B), facilitating the advancement of the balloon until reaching the inside of the stent and the post-dilatable segment.
Figure 2. Actual appearance of the spherical tip noncompliant balloon used in the study. Courtesy of APT Medical, China.
Our objective is to assess the effectiveness of this new SphNC in coronary postdilatation during percutaneous coronary intervention (PCI) in the routine clinical practice.
METHODS
The RECONQUISTHA trial is a prospective and multicenter technical registry conducted in 16 high volume PCI-capable centers (> 500 PCIs/year)8 designed to assess the effectiveness of SphNC in coronary postdilatation during PCI in the routine clinical practice. Since it is a technical registry that used no personal or clinical data on a device approved with CE marking no ethics committee approval or informed consent forms were required.
Inclusion and exclusion criteria
The only inclusion criterion was the indication for coronary postdilatation with the SphNC according to the operator (long, calcified, ostial lesion, bifurcation and angiographic or stent balloon underexpansion). The exclusion criteria were the use of a ≤ 5-Fr guide catheter, vessel size < 2mm or > 5mm, jailed branch postdilatation without previous opening of the stent struts of the main vessel towards such branch or finding 1 of the following scenarios before postdilatation: mechanical stent failure, stent edge dissection ≥ C, coronary perforation or TIMI grade ≤ 2 flow in the main vessel or lateral branch.
Procedure
All lesions were treated with stenting according to the operator’s criterion and according to the routine clinical practice (arterial access, guide catheter caliber, predilatation or plaque modification, and intracoronary imaging). Also, they should be treated with standard antithrombotic treatment (dual antiplatelet therapy with acetylsalicylic acid, and P2Y12 receptor inhibitors prior to the PCI plus weight-adjusted unfractionated heparin at doses of 100 IU/kg with further boluses to achieve activated coagulation times between 250 s and 300 s).
The use of the SphNC was considered in 2 different clinical settings that categorized the lesions into 2 study groups: use of SphNC as first-line treatment, and use of SphNC as a second choice after failed RegNC advancement. Complex techniques like the buddy-wire, buddy-balloon, anchoring or guide catheter extension system were allowed to advance both the RegNC and the SphNC. In cases where the second choice after failed RegNCn advancement was used despite the use of a complex technique, the same complex technique with the SphNC was advised too.
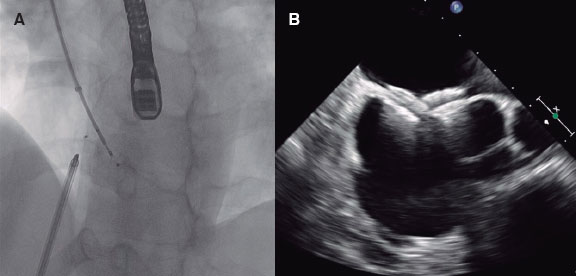
The spherical tip noncompliant balloon
The NC Conqueror Spherical tip balloon (APT Medical, China) is a rapid exchange balloon catheter for percutaneous coronary interventions that is compatible with a 0.014 in intracoronary guidewire. This device has a distinctive tungsten radiopaque spherical tip (0.039 in crossing profile) designed to minimize resistance while advancing the balloon towards the inside of the stent (figure 2). It is available in calibers ranging from 2 mm to 5 mm in intervals of 0.25 mm to 0.5 mm, and lengths of 6 mm, 8 mm, 12 mm, 15 mm, 20 mm, and 30 mm. Nominal pressure stands at 12 atm, and rated pressure burst at around 20 atm (18 atm in 4.5 mm to 5 mm calibers). The device has the CE marking.
Definition of endpoints
The study primary endpoint was technical success defined as the successful advancement of the SphNC until reaching the stent post-dilatable segment. Secondary endpoints were angiographic success—defined as technical success with residual stenosis < 30% with final TIMI grade-3 flow—and procedural success defined as angiographic success without mechanical stent failure or perioperative major adverse cardiovascular events like myocardial infarction—based on the criteria established by the Academic Research Consortium [ARC]-29—stroke, coronary perforation, need for emergency heart surgery or death.
The hypothesis was to consider the study positive if technical success was achieved in > 80% of the lesions regarding the use of the SphNC as the go-to option (according to data published on technical success rates with postdilatation balloons10), and in > 30% regarding the use of the SphNC after failed RegNC advancement (random criterion based on the success of the new balloon in 1 out of 3 cases of failed RegNC advancement).
Data curation
The characteristics of the lesion and the PCI, the indication for postdilatation, any information on the devices used, and quantitative and procedural angiographic results were collected prospectively. Data was introduced in an anonymized electronic database specifically designed for the purpose of the study. Lesions were categorized based on the classification established by the American College of Cardiology and the American Heart Association (ACC/AHA).11 Coronary calcification was defined as moderate whenever coronary radiopacities would be found prior to the injection of contrast or severe whenever these radiopacities would damage both sides of the arterial lumen.12 Coronary tortuosity was defined as moderate if ≥ 3 consecutive curvatures between 45° and 90° were found during diastole or severe if any previous curvatures between 90° and 180° would be found or that encompassed the lesion.13 Angulation inside the lesion was measured as the angle between the start and the end of stenosis. The presence of ostial stenosis > 50% in the branch lateral to the lesion or the need to place the protection guidewire in the lateral branch was considered bifurcation. The stent suboptimal expansion was defined as residual stenosis ≥ 10% on the coronary quantitative angiography after the PCI. Residual stenosis ≥ 30% was considered stent underexpansion (the use of intracoronary imaging was not mandatory). Mechanical stent failure was defined as longitudinal stent deformation or fracture. The patients’ personal or clinical data were not collected.
Statistical analysis
In each of the study groups the overall and individual data were analyzed (SphNC as the go-to option, and as the second choice after failed RegNC advancement). Data was expressed as percentages regarding the categorical variables or as mean and standard deviation regarding the continuous ones. Categorical variables were compared using the chi-square test (or Fisher’s exact test when appropriate). Continuous variables were compared using the Student t test. P values < .05 were considered statistically significant.
RESULTS
From February through June 2021, the SphNC was used in 263 lesions (in 177 lesions as the go-to option, and in 86 lesions after failed RegNC advancement) in a total of 250 procedures. All the lesions were treated with state-of-the-art drug-eluting stents. The characteristics of the lesions and the PCIs, and the immediate angiographic results—both overall and with the use of the SphNC as the first choice or after failed RegNC advancement—are shown on table 1 and table 2. A total of 9.9% of the lesions required complex techniques to move the SphNC forward. Lesions in the failed RegNC group were more unfavorable with a lower rate of direct stenting, greater tortuosity and angulation inside the lesion, more need for cutting balloon during predilatation, shorter SphNC length, and a higher rate of angiographic data of suboptimal stent expansion.
Table 1. Characteristics of the lesions
| Total (N = 263) |
SphNC as the go-to option (N = 177) |
SphNC after failed RegNC (N = 86) |
P* | Total (N = 263) |
SphNC as the go-to option (N = 177) |
SphNC after failed RegNC (N = 86) |
P* | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Target vessel | .27 | AHA classification | .1 | ||||||||
| LAD | 40.7% (107) | 41.8% (74) | 38.4% (33) | A | 2.7% (7) | 4% (7) | 0% (0) | ||||
| LCx | 20.5% (54) | 17.5% (31) | 26.7% (23) | B1 | 23.6% (62) | 26% (46) | 18.6% (16) | ||||
| RCA | 30% (79) | 31.1% (55) | 27.9% (24) | B2 | 45.2% (119) | 44.1% (78) | 47.7% (41) | ||||
| LMCA | 7.6% (20) | 8.5% (15) | 5.8% (5) | C | 26.4% (57) | 26% (46) | 33.7% (29) | ||||
| CABG | 1.2% (3) | 1.1% (2) | 1.2% (1) | Baseline TIMI flow | .65 | ||||||
| Location | .98 | 0 | 21.7% (57) | 20.9% (37) | 23.3% (20) | ||||||
| Proximal | 42.6% (112) | 42.9% (76) | 41.9% (36) | 1 | 1.1% (3) | 1.7% (3) | 0% (0) | ||||
| Medial | 43.3% (114) | 42.9% (76) | 44.2% (38) | 2 | 8.4% (22) | 8.5% (15) | 8.1% (7) | ||||
| Distal | 14.1% (37) | 14.1% (25) | 12% (12) | 3 | 68.8% (181) | 68.9% (122) | 68.6% (59) | ||||
| Calcification | .54 | Bifurcation | 29.7% (78) | 27.7% (49) | 33.7% (29) | .31 | |||||
| Moderate | 39.5% (104) | 41.2% (73) | 36% (31) | 2 stents | 7.6% (20) | 5.6% (10) | 11.6% (10) | .16 | |||
| Severe | 18.6% (49) | 16.9% (30) | 22.1% (19) | Ostial | 11.1% (24) | 13% (23) | 8.1% (7) | .24 | |||
| Tortuosity | <.001 | CTO | 5.7% (15) | 7.9% (14) | 1.2% (1) | .03 | |||||
| Moderate | 35.7% (94) | 35% (62) | 37.2% (32) | STEMI | 16.3% (43) | 13.6% (24) | 22.1% (19) | .08 | |||
| Severe | 6.1% (16) | 1.7% (3) | 15.1% (13) | Lesion on the QCA | |||||||
| Lesion angulation | <.001 | MLD (mm) | 1.01 ± 1.04 | 1.05 ± 1.06 | 0.9 ± 1 | .27 | |||||
| <30 ° | 62.4% (164) | 70.1% (124) | 46.5% (40) | VRD (mm) | 3.34 ± 0.62 | 3.3 ± 0.59 | 3.44 ± 0.65 | .09 | |||
| 30º-70 ° | 30.8% (81) | 26% (46) | 40.7% (35) | Percent diameter stenosis (%) | 83 ± 17 | 82 ± 17 | 84 ± 16 | .48 | |||
| > 70 ° | 6.8% (18) | 4% (7) | 12.8% (11) | Stenotic area (%) | 88 ± 13 | 87 ± 14 | 89 ± 12 | .13 | |||
|
AHA, American Heart Association; CABG, coronary artery bypass graft; CTO, chronic total coronary occlusion; LAD, left anterior descending coronary artery; LCx, left circumflex artery; LMCA, left main coronary artery; MLD, minimal lumen diameter; QCA, quantitative coronary angiography; RCA, right coronary artery; RegNC, cone-shaped tip regular noncompliant balloon; SphNC, spherical tip noncompliant balloon; STEMI, ST-segment elevation myocardial infarction; TIMI, Thrombolysis in Myocardial Infarction; VRD, vessel reference diameter. * P between SphNC groups as the go-to option, and SphNC after failed RegNC. |
|||||||||||
Table 2. Characteristics of percutaneous coronary intervention and angiographic outcomes
| Total (N = 263) |
SphNC as the go-to option (N = 177) |
SphNC after failed RegNC (N = 86) |
P* | Total (N = 263) |
SphNC as the go-to option (N = 177) |
SphNC after failed RegNC (N = 86) |
P* | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Plaque modification | Kissing balloon | 1.9% (5) | 2.3% (4) | 1.2% (1) | ||||||
| Noncompliant balloon | 44.9% (118) | 47.5% (84) | 39.5% (34) | .45 | Other | 1.5% (4) | 1.1% (2) | 2.3% (2) | ||
| Scoring balloon | 12.5% (33) | 9% (16) | 19.8% (17) | .14 | SphNC | |||||
| Cutting balloon | 4.9% (13) | 2.3% (4) | 10.5% (9) | .01 | Caliber (mm) | 3.36 ± 0.55 | 3.34 ± 0.53 | 3.39 ± 0.6 | .5 | |
| Lithotripsy balloon | 1.9% (5) | 1.7% (3) | 2.3% (2) | .66 | Length (mm) | 12 ± 3 | 13 ± 2 | 11 ± 2 | <.001 | |
| Rotational atherectomy | 1.9% (5) | 1.1% (2) | 3.5% (3) | .33 | Atm | 18 ± 3 | 18 ± 2 | 18 ± 3 | .09 | |
| Direct stenting | 14.1% (37) | 16.9% (30) | 8.1% (7) | .05 | Complex technique | .52 | ||||
| Stent | Guide catheter extension system | 7.6% (20) | 7.9% (14) | 7% (6) | ||||||
| Caliber (mm) | 3.07 ± 0.52 | 3.04 ± 0.49 | 3.12 ± 0.57 | .3 | Buddy-wire | 1.9% (5) | 1.1% (2) | 3.5% (3) | ||
| Length (mm) | 27 ± 11 | 27 ± 10 | 27 ± 11 | .95 | Anchoring | 0.4% (1) | 0.6% (1) | 0% (0) | ||
| Atm | 14 ± 2 | 15 ± 2 | 14 ± 2 | .02 | Intracoronary imaging | 9.5% (27) | 9.1% (16) | 10.4% (9) | .51 | |
| Number of stents in the lesion | .47 | QCA after PCI | ||||||||
| 1 | 81.4% (214) | 81.4% (144) | 81.4% (70) | MLD (mm) | 3.23 ± 0.58 | 3.19 ± 0.56 | 3.29 ± 0.61 | .21 | ||
| 2 | 13.7% (36) | 12.4% (22) | 16.3% (14) | Percent diameter stenosis (%) | 4 ± 5 | 3 ± 5 | 4 ± 5 | .18 | ||
| 3 | 5% (13) | 6.2% (11) | 2.3% (2) | Stenotic area (%) | 6 ± 8 | 5 ± 8 | 7 ± 8 | .05 | ||
| Overall stent length (mm) | 32 ± 18 | 32 ± 18 | 32 ± 16 | .96 | Stent expansion | .03 | ||||
| Postdilatation indication | .29 | Optimal | 97.7% (257) | 99.4% (176) | 94.2% (81) | |||||
| Long lesion | 39.9% (105) | 44.6% (79) | 30.2% (26) | Suboptimal | 1.9% (5) | 0.6% (1) | 4.7% (4) | |||
| Suboptimal expansion | 30.8% (81) | 28.2% (50) | 36% (31) | Underexpansion | 0.4% (1) | 0% (0) | 1.2% (1) | |||
| POT | 16% (42) | 13% (23) | 22.1% (19) | Final TIMI grade-3 flow | 99.6% (262) | 99.4% (176) | 100% (86) | 1 | ||
| Calcified lesion | 6.8% (18) | 7.3% (13) | 5.8% (5) | |||||||
| Aorto-ostial lesion | 3% (8) | 3.4% (6) | 2.3% (2) | |||||||
|
Atm, balloon inflation atmospheres; MLD, minimal lumen diameter; PCI, percutaneous coronary intervention; POT, proximal optimization technique in bifurcation; QCA, quantitative coronary angiography; RegNC, cone-shaped tip regular noncompliant balloon; SphNC, spherical tip noncompliant balloon; TIMI, Thrombolysis in Myocardial Infarction. * P between SphNC groups as the go-to option, and SphNC after failed RegNC. |
||||||||||
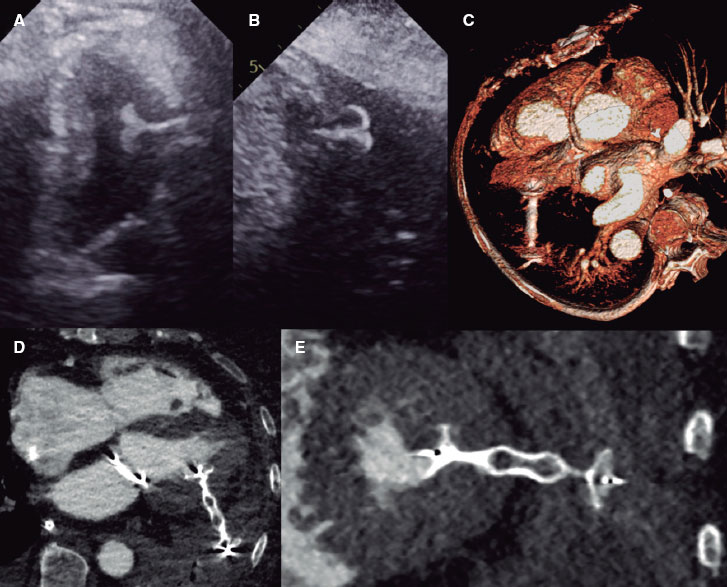
The overall rates of technical, angiographic, and procedural success were very high and similar between both groups (table 3).
Table 3. Rates of primary and secondary endpoints
| Total (N = 63) | SphNC as the go-top option (N = 177) | SphNC after failed RegNC (N = 86) | P* | |
|---|---|---|---|---|
| Primary endpoint | ||||
| Technical success | 98.9% (260) | 98.9% (175) | 98.8% (85) | 1 |
| Secondary endpoint | ||||
| Angiographic success | 98.1% (258) | 98.3% (174) | 97.7% (84) | .66 |
| Procedural success | 97.7% (257) | 98.3% (174) | 96.5% (83) | .33 |
| Mechanical stent failure | 0% (0) | 0% (0) | 0% (0) | N/A |
| Perioperative complications | 0.4% (1) | 0% (0) | 1.2% (1) | .32 |
|
N/A, non-applicable; RegNC: cone-shaped tip regular noncompliant balloon; SphNC, spherical tip noncompliant balloon. * P between SphNC groups as the go-to option, and SphNC after failed RegNC. |
||||
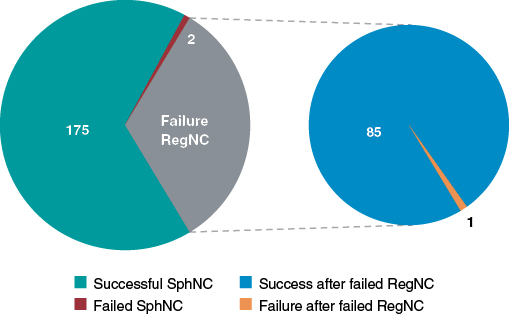
The rate of technical success in the same lesion where the RegNC had failed was very high (98.8%): only 1 SphNC failed too (figure 3). The SphNC and the RegNC had a similar mean caliber (3.39 ± 0.6 mm vs 3.34 ± 0.6 mm; P = .06) while the SphNC had a shorter mean length (11 ± 2 mm vs 12 ± 3 mm; P = .005). The length of the SphNC was shorter, similar or longer in 36%, 46.5%, and 17.5% of the lesions, respectively. The same complex techniques were used to advance the RegNC and the SphNC in 7 lesions (the guide catheter extension system and the buddy-wire technique were used in 6 and 1 cases, respectively). The buddy-wire technique was used in 2 lesions to advance the SphNC, but not previously with the RegNC. In 1 lesion where the RegNC could not be advanced despite anchoring, the SphNC was moved forward without the need for a complex technique. Both the RegNC and the SphNC had been previously used on 3 and 9 occasions, respectively for predilatation purposes.
The description of failed primary and secondary endpoints with the SphNC is shown on table 4. In 2 of the 3 cases without technical success regarding the SphNC, a shorter RegNC was eventually advanced. No instances of mechanical stent failure were reported. One proximal fracture of the catheter hypotube was reported due to excessive resistance during push in 1 SphNC. Nonetheless, the device could be retrieved uneventfully. Only 1 major adverse cardiovascular event was reported: 1 distal branch perforation due to an angioplasty guidewire unrelated with the use of the SphNC that occurred while unsuccessfully trying to advance the RegNC. However, according to the definitions of the study protocol, it was adjudicated as lack of procedural success.
Table 4. Description of cases of failed spherical tip noncompliant balloon
| Case of failed SphNC | Failed event | Use of SphNC | Postdilatation indication | Success of other NC balloons | Complex technique | Complication |
|---|---|---|---|---|---|---|
| Lesion #46 | Technical success | Go-to option | Suboptimal expansion | Yes | No | No |
| Lesion #71 | Technical success | Go-to option | Long lesion | No | No | No |
| Lesion #83 | Technical success | Failed RegNC | POT | Yes | No | Hypotube rupture |
| Lesion #84 | Angiographic success (QCA) | Failed RegNC | Suboptimal expansion | N/A | Guide catheter extension system | No |
| Lesion #224 | Angiographic success (TIMI flow) | Go-to option | Suboptimal expansion | N/A | No | No |
| Lesion #258 | Procedural success | Failed RegNC | POT | N/A | No | Coronary perforation |
|
NA, non-applicable; POT, proximal optimization technique in bifurcation; QCA, quantitative coronary angiography; RegNC, cone-shaped tip regular noncompliant balloon; SphNC, spherical tip noncompliant balloon; TIMI, Thrombolysis in Myocardial Infarction. |
||||||
Figure 3. Overall technical success and failure of the spherical tip noncompliant balloon (SphNC), as well as in cases of failed regular noncompliant balloon (RegNC); section chart on the right.
DISCUSSION
As far as we know, it is the first time that a clinical trial—the REPIC02-RECONQUISTHA—reports on the most extensive experience using SphNC for coronary stent postdilatation. The registry included 16 high volume PCI-capable centers and collected data from 263 lesions where SphNCs were used at the operator’s discretion both as the go-to and second choice after failed RegNC advancement in the same lesion. Based on the initial hypothesis, the study can be considered positive; findings can be summarized as follows: a) very high rates of technical, angiographic and procedural success defined, respectively, as the capacity to move forward towards the inside of the stent and reach an adequate expansion without mechanical stent failure or periprocedural complications; b) very high rates of technical, angiographic and procedural success in the same lesions where the RegNC failed; and c) lower need for complex techniques to achieve technical success.
Over the last few years, the arrival of new techniques and modern devices has facilitated the performance of successful PCIs on more complex lesions in the routine clinical practice. Although the operators were not specifically encouraged to include complex lesions in the study, our data show this reality where over 70% of the lesions were type B2/C, and nearly 50% showed significant calcification, tortuosity or angulation inside the lesion. These characteristics reduce the success of the PCI14,15 and can eventually lead to stent malapposition16 and underexpansion17 or difficulties advancing the devices until reaching such stents, which means that the availability of effective and safe postdilatation balloons is essential to perform successful PCIs.
There is no data in the medical literature to compare or discuss our findings. Our study can be considered positive as it exceeded 80% of the success anticipated in the initial hypothesis. Despite the complexity of the lesions reported, the overall and subgroup outcomes of use of the SphNCs as the go-to option are nothing new since they can be expected in the assessment of any NC balloons (rate of success and proper stent expansion > 90%)10 since it is rare to find difficulties or impossibilities if complex techniques are used to advance these devices. However, these maneuvers can lead to severe complications like mechanical stent deformation.18,19 The lack of mechanical stent failure in our series places the SphNC as an effective and safe device for coronary postdilatation.
After the first 200 procedures, the percentage of cases where the SphNC was used in lesions where the RegNC would have failed was low. Since focus was on assessing the SphNC performance in this context, only inclusions in this subgroup were allowed later on. As already mentioned, the rate of RegNC failure is rare, and the rhythm of inclusion of the next 50 procedures was a slower. We designed this study group considering that the sequential use of a SphNC in the same lesion where a RegNC had failed would show the potential benefit of this new device. The SphNC achieved technical success in 98.8% of the lesions in this subgroup and validated its superiority in the exact same lesions where the RegNC had failed, which can be considered the most valuable piece of information from our study. The mean SphNC length was shorter compared to the RegNC (a 1 mm difference, which is statistically significant due to similar and narrow standard deviations, yet of uncertain practical significance). However, the operators used SphNCs and RegNCs of similar length in most of the lesions. In this study subgroup, lesions were more unfavorable, which may explain the rate of failure with RegNCs, the discretely low rate of angiographic and procedural success reported, and the presence of the complications described (fracture of the SphNC hypotube or coronary perforation).
It has been reported that the tortuosity and angulation seen until the lesion are predictors of failed PCI or perioperative complications.14,15,20 In our series, their prevalence was high—around 40%—and up to 50% in lesions where the RegNC failed. Several complex techniques for the management of these anatomies have been described,21 but they increase procedural time and cost. Eddin et al.22 determined that tortuosity and angulation were the main predictors for the use of a guide catheter extension system. Also, angulations > 45° proximal to the lesion predict its use with a 73% sensitivity and a 74% specificity. In different series, tortuosity and angulation justify the use of a guide catheter extension system in 22% to 43% of the cases.18 Despite the significant tortuosity and angulation of our series, the need for a guide catheter extension system or any other kind of complex technique to advance the SphNC was low (< 8% and 10% respectively), which is why this device emerges as a useful tool in the coronary tortuosity setting with potential to reduce procedural costs.
The study design was moderately ambitious since we hypothesized that if the SphNC were successful in 1 out of 3 lesions where the RegNC had failed this outcome would have been good enough for the new device. The fact that it exceeded the success rate of 30% proposed in the hypothesis makes us think of the results as positive. To better understand these outcomes, 5 videos have been provided as supplementary data including examples of failed RegNCs and succesful SphNCs in the same lesion.
Limitations
Despite its prospective design, the study has several limitations. The indication of postdilatation with SphNC based only on the operator’s criterion may have conditioned selection biases, thus preventing the inclusion of very unfavorable lesions. The study design does not allow us to assess the superiority of the SphNC over the RegNC regarding the lower need for complex techniques, mechanical stent failure or better angiographic and procedural outcomes. The use of intracoronary imaging was low, and a more comprehensive assessment of stent expansion with imaging techniques could have changed the data of the PCI final outcomes and, consequently, the secondary endpoints. The SphNC recrossing after first inflation was anecdotal and is, therefore, ill-advised. We should mention that our results cannot be extrapolated to coronary predilatation because the device has not been tested prior to stenting. Finally, the lack of follow-up to monitor the patients’ clinical course does not allow us to assess the clinical impact derived from the use of SphNC.
CONCLUSIONS
Coronary postdilatation with the SphNC during PCI in the routine clinical practice has a very high rate of technical success both as first choice (98.9%), and in cases of failed RegNC advancement (98.8%) with a lower need for complex techniques, and a good safety profile.
FUNDING
RECONQUISTHA is an investigator-initiated trial promoted and developed by Fundación EPIC, Spain as the clinical research organization sponsored by IZASA Medical, Spain. All the authors received research grants for their participation in the study.
AUTHORS’ CONTRIBUTIONS
J. A. Linares Vicente: design, data curation, analysis, and interpretation, and manuscript drafting. A. Pérez de Prado, and J. R. Rumoroso Cuevas: design, data curation, manuscript drafting, and critical review of its content. K. García San Román, F. Lozano Ruiz-Póveda, G. Veiga Fernández, A. Gómez Menchero, G. Moreno Terribas, G. Miñana Escrivà, J. Sánchez Gila, C. Arellano Serrano, G. Martín Cáceres, P. Bazal Chacón, P. Martín Lorenzo, F. Rebollal Leal, and J. Moreu Burgos: data curation, critical review of the content of the manuscript, and final approval.
CONFLICTS OF INTEREST
A. Pérez de Prado is an associate editor of REC: Interventional Cardiology; the journal’s editorial procedure to ensure impartial handling of the manuscript has been followed. J. A. Linares has received lecture fees from IZASA Medical, Spain.
WHAT IS KNOWN ABOUT THE TOPIC?
- Coronary stent postdilatation with NC balloons is associated with better clinical outcomes. The complexity of PCIs in the routine clinical practice is on the rise. The navigability of RegNCs is limited, and their cone-shaped tip can complicate moving forward inside of the stent. Therefore, success could be limited in in complex lesions.
WHAT DOES THIS STUDY ADD?
- In the routine clinical practice, coronary postdilatation using SphNC while performing a PCI has a very high rate of technical success even in complex clinical settings where the RegNC has failed (especially in coronary tortuosity), a lower need for complex techniques, and a good safety profile. Therefore, it could be considered as the go-to option for coronary postdilatation when performing complex PCIs.
SUPPLEMENTARY DATA
Vídeo 1. Linares Vicente J.A. DOI: 10.24875/RECICE.M22000289
Vídeo 2. Linares Vicente J.A. DOI: 10.24875/RECICE.M22000289
Vídeo 3. Linares Vicente J.A. DOI: 10.24875/RECICE.M22000289
Vídeo 4. Linares Vicente J.A. DOI: 10.24875/RECICE.M22000289
Vídeo 5. Linares Vicente J.A. DOI: 10.24875/RECICE.M22000289
REFERENCES
1. Takano Y, Yeatman LA, Higgins JR, et al. Optimizing stent expansion with new stent delivery systems. J Am Coll Cardiol. 2001;38:1622-1627.
2. Romagnoli E, Sangiorgi GM, Cosgrave J, Guillet E, Colombo A. Drug-Eluting Stenting. The Case for Post-Dilation. JACC: Cardiovasc Interv. 2008;
1:22-31.
3. Brodie BR, Cooper C, Jones M, Fitzgerald P, Cummins F. Is adjunctive balloon postdilatation necessary after coronary stent deployment? Final results from the POSTIT trial. Catheter Cardiovasc Interv. 2003;59:184-192.
4. Seth A, Gupta S, Singh VP, Kumar V. Expert Opinion: Optimising stent deployment in contemporary practice: The role of intracoronary imaging and non-compliant balloons. Interv Cardiol. 2017;12:81-84.
5. Pasceri V, Pelliccia F, Pristipino C, et al. Clinical effects of routine postdilatation of drug-eluting stents. Catheter Cardiovasc Interv. 2014;83:898-904.
6. Mylotte D, Hovasse T, Ziani A, et al. Non-compliant balloons for final kissing inflation in coronary bifurcation lesions treated with provisional side branch stenting: A pilot study. EuroIntervention. 2012;7:1162-1169.
7. Park TK, Lee JH, Song YB, et al. Impact of non-compliant balloons on long-term clinical outcomes in coronary bifurcation lesions: Results from the COBIS (COronary BIfurcation Stent) II registry. EuroIntervention. 2016;12:456-464.
8. Moreno R, Ojeda S, Romaguera R, et al. Actualización de las recomendaciones sobre requisitos y equipamiento en cardiología intervencionista. REC Interv Cardiol. 2021;3:33-44.
9. Garcia-Garcia HM, McFadden EP, Farb A, et al. Standardized End Point Definitions for Coronary Intervention Trials: The Academic Research Consortium-2 Consensus Document. Circulation. 2018;137:2635-2650.
10. Secco GG, Buettner A, Parisi R, et al. Clinical Experience with Very High-Pressure Dilatation for Resistant Coronary Lesions. Cardiovasc Revasc Med. 2019;20:1083-1087.
11. Ryan TJ, Faxon DP, Gunnar RM, et al. Guidelines for percutaneous transluminal coronary angioplasty. A report of the American College of Cardiology/American Heart Association Task Force on Assessment of Diagnostic and Therapeutic Cardiovascular Procedures (Subcommittee on Percutaneous Transluminal Coronary Angioplasty). Circulation. 1988;78:486-502.
12. Madhavan MV, Tarigopula M, Mintz GS, Maehara A, Stone GW, Généreux P. Coronary Artery Calcification. J Am Coll Cardiol. 2014;63:1703-1714.
13. Jakob M, Spasojevic D, Krogmann ON, Wiher H, Hug R, Hess OM. Tortuosity of coronary arteries in chronic pressure and volume overload. Cathet Cardiovasc Diag. 1996;38:25-31.
14. Ellis SG, Vandormael MG, Cowley MJ, et al. Coronary morphologic and clinical determinants of procedural outcome with angioplasty for multivessel coronary disease. Implications for patient selection. Multivessel Angioplasty Prognosis Study Group. Circulation. 1990;82:1193-1202.
15. Moushmoush B, Kramer B, Hsieh AM, Klein LW. Does the AHA/ACC task force grading system predict outcome in multivessel coronary angioplasty? Cathet Cardiovasc Diag. 1992;27:97-105.
16. Wang B, Mintz GS, Witzenbichler B, et al. Predictors and Long‐Term Clinical Impact of Acute Stent Malapposition: An Assessment of Dual Antiplatelet Therapy With Drug‐Eluting Stents (ADAPT‐DES) Intravascular Ultrasound Substudy. J Am Heart Assoc. 2016;5:e004438.
17. Komaki S, Ishii M, Ikebe S, et al. Association between coronary artery calcium score and stent expansion in percutaneous coronary intervention. Int J Cardiol. 2021;334:31-36.
18. Fabris E, Kennedy MW, di Mario C, et al. Guide extension, unmissable tool in the armamentarium of modern interventional cardiology. A comprehensive review. Int J Cardiol. 2016;222:141-147.
19. Arnous S, Shakhshir N, Wiper A, et al. Incidence and mechanisms of longitudinal stent deformation associated with Biomatrix, Resolute, Element, and Xience stents: Angiographic and case-by-case review of 1,800 PCIs. Catheter Cardiovasc Interv. 2015;86:1002-11.
20. Ellis SG, Topol EJ. Results of percutaneous transluminal coronary angioplasty of high-risk angulated stenoses. Am J Cardiol. 1990;66:932-7.
21. Saeed B, Banerjee S, Brilakis ES. Percutaneous Coronary Intervention in Tortuous Coronary Arteries: Associated Complications and Strategies to Improve Success. J Interv Cardiol. 2008;21:504-511.
22. Eddin MJ, Armstrong EJ, Javed U, Rogers JH. Transradial interventions with the GuideLiner catheter: Role of proximal vessel angulation. Cardiovasc Revasc Med. 2013;14:275-279.
* Corresponding author.
E-mail address: jalinares@salud.aragon.es (J.A. Linares Vicente).