ABSTRACT
Introduction and objectives: The need for complete coronary artery revascularization after acute coronary syndrome in diabetic patients with multivessel coronary artery disease was discussed, even more so if they reflect the routine clinical practice (“real world”). Therefore, the objective of this study is to analyze cardiovascular complications in diabetics with and without complete revascularization included in clinical trials and in the routine clinical practice.
Methods: This was a single-center retrospective study of diabetic patients with multivessel coronary artery disease. We analyzed 733 diabetic patients: 299 (40.8%) with compatible criteria to be included in clinical trials, and 434 real-world patients (59.2%).
Results: Real-world patients make up 59.2% of the sample. They are characterized by a higher percentage of risk factors, older mean age, and more comorbidities. Diabetics with multivessel coronary artery disease included in the trials have a lower risk of overall mortality (HR, 0.30; 95%CI, 0.16-0.57; P < .001), cardiac death (HR, 0.33; 95%CI, 0.15-0.71; P = .03), and major adverse cardiovascular events (HR, 0.58; 95%CI, 0.38-0.86; P = .008). On the other hand, receiving complete revascularization reduces the risk of cardiac death (HR, 0.32; 95%CI, 0.13-0.83; P = .019), and major adverse cardiovascular events (HR, 0.50; 95%CI, 0.29-0.89; P = .017) in real-world diabetic patients.
Conclusions: It is suggested that fully revascularizing real-world patients would improve survival prognosis. In addition, diabetics included in clinical trials present fewer complications compared to those not included.
Keywords: Diabetes. Revascularization. Real world. Multivessel coronary artery disease.
RESUMEN
Introducción y objetivos: Se debate la necesidad de realizar revascularización coronaria completa tras un síndrome coronario agudo en pacientes diabéticos con enfermedad coronaria multivaso, y más aún si estos son reflejo de los pacientes de la práctica clínica habitual (mundo real). Por ello, el objetivo de este trabajo es analizar las complicaciones cardiovasculares en pacientes diabéticos con y sin revascularización completa incluibles en ensayos clínicos como de la práctica clínica habitual.
Métodos: Estudio unicéntrico retrospectivo de pacientes diabéticos con enfermedad coronaria multivaso. Se analizaron 733 pacientes diabéticos: 299 (40,8%) con criterios compatibles de inclusión de ensayos clínicos y 434 (59,2%) del mundo real.
Resultados: Los pacientes del mundo real constituyen el 59,2% de la muestra. Se caracterizan por presentar mayor porcentaje de factores de riesgo, mayor edad media y comorbilidad. Los diabéticos con enfermedad coronaria multivaso incluibles en ensayos tienen menor riesgo de mortalidad total (HR = 0,30; IC95%, 0,16-0,57; p < 0,001), de mortalidad de causa cardiaca (HR = 0,33; IC95%, 0,15-0,71; p = 0,03) y de sufrir eventos cardiovasculares adversos mayores (HR = 0,58; IC95%, 0,38-0,86; p = 0,008). Por otro lado, recibir revascularización completa desciende el riesgo de mortalidad de causa cardiaca (HR = 0,32; IC95%, 0,13-0,83; p = 0,019) y de eventos cardiacos adversos mayores (HR = 0,50; IC95%, 0,29-0,89; p = 0,017) en los pacientes diabéticos del mundo real.
Conclusiones: Se sugiere que revascularizar completamente a los pacientes del mundo real mejoraría el pronóstico en cuanto a supervivencia. Asimismo, los diabéticos incluibles en ensayos clínicos presentan menos complicaciones que los diabéticos no incluibles.
Palabras clave: Diabetes. Revascularización. Mundo real. Enfermedad coronaria multivaso.
Abbreviations
CR: complete revascularization. IR: incomplete revascularization. MACCE: major adverse cardiovascular and cerebrovascular events. MACE: major adverse cardiovascular events. MCAD: multivessel coronary artery disease.
INTRODUCTION
Cardiovascular diseases—the most prominent of which is ischemic heart disease (IHD)—are a problem of global health and responsible for 1 out of every 3 premature deaths worldwide.1 In Spain, IHD is thought to increase health spending and morbidity due to the ageing of the population, and the greater number of survivors.2
Diabetes mellitus is closely associated with ischemic heart disease. It makes patients—most of them elderly patients—have a very high cardiovascular risk.3 Hypoglycemia and hyperinsulinemia are both associated with a higher risk of developing multivessel coronary artery disease (MCAD).4 In the long-term, this leads to a grim prognosis and more cardiovascular death in these diabetic patients.5
Due to the high incidence rate of MCAD, several studies have been conducted to see what type of revascularization is the most suitable one for the profile of these patients. It has been suggested that anatomic complete revascularization (CR) is associated with a lower rate of major adverse cardiovascular events (MACE)—a composite endpoint of death, non-fatal myocardial infarction, and need for new revascularization—compared to anatomic incomplete revascularization (IR).6 As a matter of fact, it has been reported that the risk of MACE increases significantly when performing IR with minimal residual disease in coronary vessels.7 Therefore, the treatment recommended is to perform anatomic CR. When this is not feasible, functional CR—currently widely used—is advised.
On the one hand, in patients with stable angina refractory to conservative treatment or non-ST-segment elevation acute coronary syndrome (NSTEACS), single-stage CR is advised through surgical coronary revascularization or percutaneous coronary intervention.8 On the other hand, in patients with ST-segment elevation acute coronary syndrome (STEACS) staged CR has been suggested by treating, first of all, the culprit coronary artery causing the clinical signs, and then the remaining stenotic arteries.9 However, in the routine clinical practice, it has been observed that patients with greater comorbidities and worse prognosis are often treated with IR, which worsens even more their clinical evolution since the survival associated with cardiac death, and MACE is lower.10
However, one of the main problems we face is passing scientific knowledge from clinical trials on to the routine clinical practice. It has been reported that most of the patients from cardiology units meet some of the exclusion criteria posed by these clinical trials. Such patients are highly heterogeneous, older, and have several cardiovascular risk factors and concomitant diseases, which worsens their prognosis. Therefore, the findings from clinical trials should be used with caution in the overall population.11,12
Thus, the objective of this study was to analyze whether there are significant differences regarding mortality and cardiovascular events between patients treated with CR or IR, which is why patients with clinical trial inclusion criteria and patients with characteristics from the routine clinical practice (real world) were included.
METHODS
This was a retrospective, single-center study that used data anonymization and included 733 diabetic patients with MCAD treated with coronary angiography from January 1, 2012 through December 31, 2014. Participants were divided into 2 groups based on whether or not they met the FREEDOM clinical trial inclusion criteria.13 In this study, those who met these criteria were considered participants eligible for clinical trials while the rest (the non-eligible ones) were categorized as patients from the routine clinical practice or real-world patients.
Due to data anonymization, it was not necessary to request any approval from the ethics committee since it had already been obtained by Chueca González et al.10 who used the same patient selection. The different informed consents authorize us to treat data to conduct this study.
Study population
Patients over 18 years old with an indication for revascularization—both percutaneous coronary intervention and surgery—due to acute coronary syndromes (STEACS, NSTEACS or unstable angina), refractory stable angina, refractory heart failure, valvular heart disease, cardiac arrest, new revascularization or cardiogenic shock were included in the study Patients with previous cardiac surgeries due to coronary artery disease and valvular heart disease, as well as patients with valvular heart diseases plus a surgical indication were excluded from the study.
The following were categorized as real-world patients (non-FREEDOM): those with STEACS within the 72 previous hours, those with a past medical history of percutaneous transluminal angioplasty, stroke or major bleeding within the previous 6 months, those with functional class III or IV according to the New York Heart Association, in-stent restenosis, known dementia or dependency, at least moderate, according to the Barthel index, and finally those with an extracardiac disease (chronic obstructive pulmonary disease, hepatopathies, chronic kidney disease) bringing survival under 5 years. All the criteria developed have been described previously.10
Definitions
When coronary angiography was performed, patients were considered diabetic if they had already been diagnosed as such in their health record or if they were on hypoglycemic treatments like diet, oral antidiabetic drugs or insulin.
MCAD consists of the existence of ≥ 70% luminal stenosis in 2 or more epicardial vessels covering, at least, 2 or more different coronary artery territories. Also, such lesions are prone to revascularization via angioplasty and surgery according to the clinical practice guidelines and the criterion of interventional cardiologists and cardiac surgeons.
Coronary lesions were treated with anatomic CR. Epicardial vessels > 2 mm in caliber with > 70% stenosis were treated regardless of whether the areas compromised were viable or necrotic.
The indication to perform the coronary angiography was given based on the patient’s clinical course that led to his admission. Acute coronary syndromes with and without ST-segment elevation according to the third universal definition of infarction were included.14 Also, this test was performed on other diseases like unstable angina, refractory stable angina to medical treatment, and other (decompensated heart failure, cardiogenic shock, cardiac arrest, ventricular arrhythmias).
Left ventricular ejection fraction was categorized as dichotomic with values ≥ 40% or < 40%.
To assess the stage of kidney failure the glomerular filtration rate was estimated using the CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) equation. It was defined as reduced with glomerular filtration rates < 45 mL/min/1.73 m3, which is consistent with stage 3B chronic kidney disease.
Regarding the variables that should be measure at the follow-up, events such as death, non-fatal myocardial infarction, and new revascularization were categorized as MACE. On the other hand, major adverse cardiovascular and cerebrovascular events (MACCE) were considered a composite endpoint of death, non-fatal myocardial infarction, new revascularization, and stroke.
Statistical analysis
All statistical analyses were conducted using the statistical software package SPSS version 21.0 for Windows. Quantitative variables were studied using the Student t test for independent samples, and expressed as mean ± standard deviation. Cualitative variables were compared using the chi-square test and expressed as percentages and absolute numbers. Also, the odds ratios (OR) were obtained too. Multivariate analysis was conducted through survival analysis using Cox regression method. Also, survival charts and hazard ratios (HR) with their corresponding 95% confidence intervals were obtained for the significant covariables of the univariate analysis. P values ≤ .05 were considered statistically significant.
RESULTS
A total of 733 diabetic patients met the inclusion criteria to participate in the study. A total of 299 of these patients (40.8%) had criteria that were compatible with the clinical trials, and 434 (59.2%) with the real world. The presence of CR was less common in both groups compared to participants treated with IR. Among the patients in whom CR was achieved, this type of revascularization turned out to be more common in those with criteria from the FREEDOM trial (43.5%).
Patients’ baseline characteristics
Multiple parameters collected at admission were analyzed to perform coronary angiography (table 1).
Table 1. Patients’ baseline characteristics based on compliance of the FREEDOM criteria
| Total | CR in patients from CT | IR in patients from CT | P | Total | CR in patients from the RCP | IR in patients from the RCP | P | |
|---|---|---|---|---|---|---|---|---|
| N | 40.8 (299) | 43.5% (130) | 56.5% (169) | < .001 | 59.2% (434) | 28.3% (123) | 71.7% (311) | < .001 |
| Age | 66.2 ± 9 | 64.1 ± 9.1 | 68 ± 8.4 | < .001 | 69.8 ± 9.6 | 67.5 ± 9.9 | 70.7 ± 9.3 | .002 |
| + 80 years | 6 (18) | 16.7 (3) | 83.3 (15) | .10 | 15.4 (67) | 17.9 (12) | 82.1 (55) | .364 |
| Woman | 30.1 (90) | 40 (36) | 60 (54) | .45 | 31.1 (135) | 28.1 (38) | 71.9 (97) | .95 |
| 3 vessels | 44.8 (134) | 30.6 (41) | 69.4 (93) | < .001 | 54.6 (171) | 35.3 (30) | 61.8 (141) | < .001 |
| Indication | .42 | .01 | ||||||
| STEACS | 2(6) | 16.7 (1) | 83.3 (5) | 32.5 (141) | 39 (55) | 61 (86) | ||
| NSTEACS | 35.5 (106) | 40.6 (43) | 59.4 (63) | 32 (139) | 19.4 (27) | 80.6 (112) | ||
| Unstable angina | 28.4 (85) | 47.1 (40) | 52.9 (45) | 15.7 (57) | 27.9 (19) | 72.1 (49) | ||
| Stable angina | 28.1 (84) | 47.6 (40) | 52.4 (44) | 13.1 (57) | 29.8 (17) | 70.2 (40) | ||
| LVEF < 40% | 14.4 (43) | 32.6 (14) | 67.4 (29) | .14 | 29.8 (129) | 21. (28) | 78.3 (101) | .048 |
| Hypertension | 84.3 (252) | 42.9 (108) | 57.1 (144) | .63 | 84.1 (365) | 26 (95) | 74 (270) | .046 |
| Dyslipidemia | 66.9 (200) | 45 (90) | 55 (110) | .46 | 61.1 (265) | 25.7 (68) | 74.3 (197) | .127 |
| Obesity | 28.1 (84) | 52.4 (44) | 47.6 (40) | .07 | 27.9 (121) | 27.3 (33) | 72.7 (88) | .813 |
| Tobacco use history | 46.5 (139) | 51.1 (71) | 48.9 (68) | .019 | 43.5 (189) | 29.1 (55) | 70.9 (134) | .078 |
| Treatment of DM | 43.5 (130) | 56.5 (169) | .67 | 28.3 (123) | 71.7 (311) | .83 | ||
| Diet | 7.7 (23) | 52.2 (12) | 47.8 (11) | 31.8 (7) | 68.2 (15) | |||
| Oral antidiabetic drugs | 65.9 (197) | 43.1 (85) | 56.9 (112) | 27.3 (73) | 72.7 (194) | |||
| Insulin | 26.4 (79) | 41.8 (33) | 58.2 (46) | 29.7 (43) | 70.3 (102) | |||
| Previous infarction | 12.7 (38) | 28.9 (11) | 71.1 (27) | .053 | 17.3 (75) | 32 (24) | 68 (51) | .439 |
| Heart failure | 4.3 (13) | 23.1 (3) | 76.9 (10) | .129 | 9.2 (40) | 7.5 (3) | 92.5 (37) | .002 |
| Peripheral arterial disease | 8.4 (25) | 32 (8) | 68 (17) | .227 | 13.8 (60) | 15 (9) | 85 (51) | .014 |
| Stroke | 6.4 (19) | 31.6 (6) | 68.4 (13) | .28 | 9.4 (41) | 22 (9) | 78 (32) | .34 |
| COPD | 13.7 (41) | 46.3 (19) | 53.7 (22) | .691 | 18.7 (81) | 21 (17) | 79 (64) | .103 |
| GFR < 45 | 7.4 (22) | 18.2 (4) | 81.8 (18) | .013 | 13.8 (60) | 16.7 (10) | 83.3 (50) | .031 |
| Previous PCI | 17.1 (51) | 35.3 (18) | 64.7 (33) | .195 | 22.1 (96) | 25 (24) | 75 (72) | .41 |
| EuroSCORE II | 2.27±2.27 | 1.84 ± 1.62 | 2.59 ± 2.63 | .004 | 7.57 ± 11.2 | 5.71 ± 7.98 | 8.39 ± 12.24 | .025 |
|
COPD, chronic obstructive pulmonary disease; CR, complete revascularization; CT, clinical trials; DM, diabetes mellitus; GFR, glomerular filtration rate; IR, incomplete revascularization; LVEF, left ventricular ejection fraction; NSTEACS, non-ST-segment elevation acute coronary syndrome; PCI, percutaneous coronary intervention; RCP, routine clinical practice; STEACS, ST-segment elevation acute coronary syndrome. Data are expressed as no. (%). |
||||||||
Differences were found when patients were compared based on their clinical characteristics (patients from clinical trials and from the real world) and type of revascularization received. The most significant differences were found in real-world patients. On the one hand, mean age (69.8 years) was older with more patients > 80 years compared to the group with clinical trial criteria (mean, 66.2 years). On the other hand, in this group there was a higher incidence rate of coronary artery disease with damage to 3 vessels (54.6%) compared to patients from clinical trials (44.8%). Regarding the indication of coronary angiography, a higher rate of acute coronary syndromes—both STEACS and NSTEACS—in such subgroup was reported. They were eventually treated with IR (61% and 80.6%; P < .001) more often. However, patients with characteristics from clinical trials had NSTEACS, and unstable and stable angina as the main indications for coronary angiography. In these patients, CR was achieved more often compared to real-world diabetics.
Major events at 30-day and 35-month follow-up
When it comes to patients with clinical trial inclusion criteria, achieving CR suggested the occurrence of fewer major events—both overall mortality and cardiovascular system-related mortality—especially at 35-month follow-up without any significant differences being reported (table 2).
Table 2. Major events at 30-day and 35-month follow-up in patients with criteria from the FREEDOM clinical trial
| Event | 30 days | P | 35 months | P | ||
|---|---|---|---|---|---|---|
| CR | IR | CR | IR | |||
| Mortality | 0.4 (1) | 0.4 (1) | .863 | 2.8 (5) | 6.7 (12) | .285 |
| Cardiac death | 0 | 0.4 (1) | .375 | 1.1 (2) | 4.5 (8) | .154 |
| Acute myocardial infarction | 0.4 (1) | 0.7 (2) | .715 | 2.4 (4) | 5.4 (9) | .359 |
| Stroke | 0 | 0.7 (2) | .209 | 1.2 (2) | 1.9 (3) | .883 |
| MACE | 0.7 (2) | 1.5 (4) | .601 | 9.7 (19) | 17.9 (35) | .348 |
| MACCE | 0.7 (2) | 2.2 (6) | .277 | 11.2 (22) | 18.9 (37) | .451 |
|
CR, complete revascularization; IR, incomplete revascularization; MACE, major adverse cardiovascular events (death, non-fatal myocardial infarction, and need for new revascularization); MACCE, major adverse cardiovascular and cerebrovascular events (death, non-fatal myocardial infarction, need for new revascularization and stroke). Data are expressed as no. (%). |
||||||
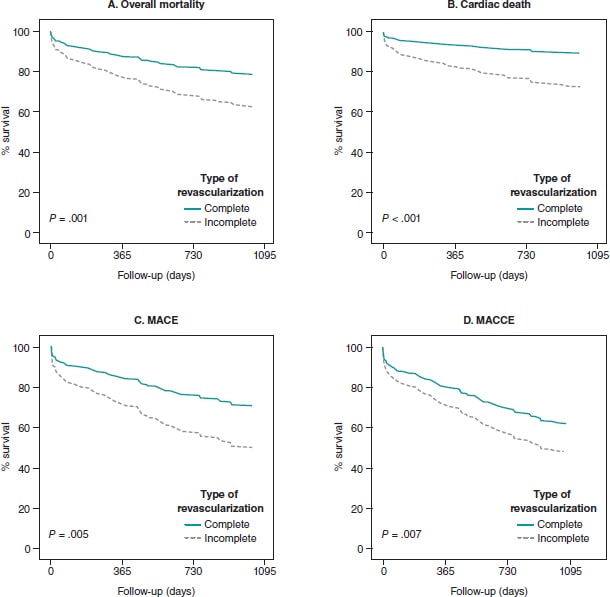
The same tendency was seen in real-world patients. Therefore, CR reduced the risk of overall mortality (OR, 0.84; 95%CI, 0.74-0.95; P = .006), cardiac death (OR, 0.81; 95%CI, 0.73-0.91; P = .002), and MACE (OR, 0.84; 95%CI, 0.74-0.96; P = .012) at 35-month follow-up (table 3). In the survival analysis, the same tendency was found in the said subgroup of participants at 35-month follow-up. CR reduced the risk of cardiac death (HR, 0.35; 95%CI, 0.13-0.90; P = .029), and MACE (HR, 0.5; 95%CI, 0.28-0.89; P = .019). Similarly, EuroSCORE-II > 5 increased the risk of cardiac death (HR, 2.74; 95%CI, 1.11-6.75; P = .028). Finally, a higher risk of MACE (HR, 2.08; 95%CI, 1.03-4.23; P = .042), and MACCE (HR, 2.36; 95%CI, 1.13-4.95; P = .023) was reported (figure 1).
Table 3. Major events at 30-day and 35-month follow-up in patients from the routine clinical practice
| Event | 30 days | P | 35 months | P | ||
|---|---|---|---|---|---|---|
| CR | IR | CR | IR | |||
| Mortality | 1.8 (6) | 8.5 (29) | .257 | 5.5 (14) | 38.4 (98) | .006 |
| Cardiac death | 1.5 (5) | 8.1 (27) | .195 | 3.2 (8) | 31.2 (78) | .002 |
| Acute myocardial infarction | 0.7 (3) | 1.7 (7) | .911 | 7.7 (21) | 17.2 (47) | .626 |
| Stroke | 0 | 0.3 (1) | .522 | 1.5 (3) | 4.9 (10) | .650 |
| MACE | 1.7 (5) | 7.9 (24) | .225 | 6.5 (15) | 40 (92) | .012 |
| MACCE | 1.7 (5) | 7.9 (24) | .225 | 8.3% (19) | 41.3 (95) | .089 |
|
CR, complete revascularization; IR, incomplete revascularization; MACE, major adverse cardiovascular events (death, non-fatal myocardial infarction, and need for new revascularization; MACCE, major adverse cardiovascular and cerebrovascular events (death, non-fatal myocardial infarction, need for new revascularization and stroke).Data are expressed as no. (%). |
||||||
Figure 1. Evolution of survival in diabetic patients from the routine clinical practice with multivessel coronary artery disease. MACE, major adverse cardiovascular events (death, non-fatal myocardial infarction, and need for new revascularization); MACCE, major adverse cardiovascular and cerebrovascular events (death, non-fatal myocardial infarction, need for new revascularization and stroke).
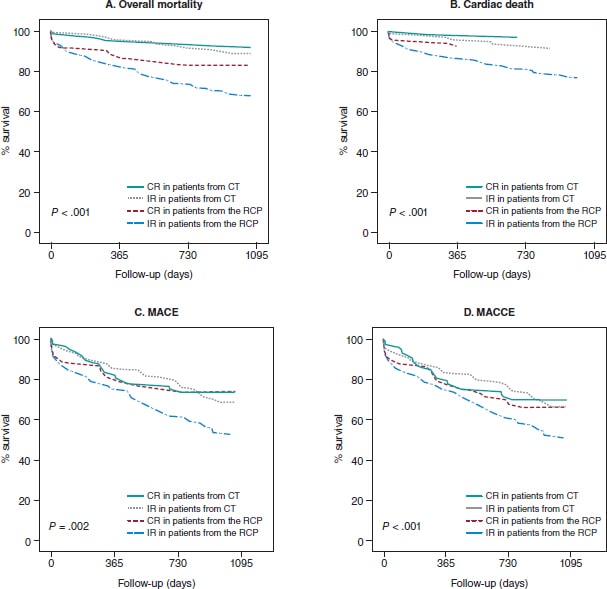
When survival was analyzed in the 4 groups of patients (figure 2), those with FREEDOM clinical trial inclusion criteria had a lower risk of overall mortality (HR, 0.30; 95%CI, 0.16-0.57; P < .001), cardiac death (HR, 0.33; 95%CI, 0.15-0.71; P = .03), MACE (HR, 0.58; 95%CI, 0.38-0.86; P = .008), and MACCE (HR, 0.59; 95%CI, 0.40-0.89; P = .01). On the one hand, achieving CR lowered the risk of cardiac death (HR, 0.32; 95%CI, 0.13-0.83; P = .019), and MACE (HR, 0.50; 95%CI, 0.29-0.89; P = .017). On the other hand, EuroSCORE > 5 when coronary angiography was performed was associated with higher rates of overall mortality (HR, 2.16; 95%CI, 1.06-4.41; P = .034), cardiac death (HR, 3.48; 95%CI, 1.49-8.16; P = .004), MACE (HR, 2.18; 95%CI, 1.26-3.78; P = .005), and MACCE (HR, 2; 95%CI, 1.18-3.40; P = .011). It was reported that if the patient had heart failure, this increased the risk of MACE (HR, 2.44; 95%CI, 1.25-4.74; P = .009), and MACCE (HR, 2.77; 95%CI, 1.39-5.53; P = .004). On the remaining variables, a lower overall mortality rate was confirmed if the patient was a non-smoker (HR, 0.46; 95%CI, 0.24-0.89; P = .02), and a higher risk of MACCE was reported if he had hypertension (HR, 1.50; 95%CI, 1.01-2.24; P = .049) or 3-vessel disease (HR, 1.44; 95%CI, 1.06-1.97; P = .022).
Figure 2. Evolution of survival in diabetic patients con multivessel coronary artery disease. CT, clinical trials; CR, complete revascularization; IR, incomplete revascularization; MACCE, major adverse cardiovascular and cerebrovascular events (death, non-fatal myocardial infarction, need for new revascularization and stroke); MACE, major adverse cardiovascular events (death, non-fatal myocardial infarction, and need for new revascularization); RCP, routine clinical practice.
Type of procedure received
Regarding the therapies received, we found a higher rate of percutaneous coronary interventions (80.8%) performed in all the study subgroups. Real-world patients were treated with coronary artery bypass graft more often compared to patients from clinical trials. Finally, conservative treatment was more common (9%) in real-world patients with IR (table 4).
Table 4. Type of procedures performed per group of patients
| Treatment | CR in patients from CT | IR in patients from CT | CR in patients from the RCP | IR in patients from the RCP | Total |
|---|---|---|---|---|---|
| Conservative | 0 | 4.1 (7) | 0 | 9 (28) | 4.8 (35) |
| PCI | 78.5 (102) | 87 (147) | 76.4 (94) | 80.1 (249) | 80.8 (592) |
| CABG | 21.5 (28) | 8.9 (15) | 23.6 (29) | 10.9 (34) | 14.5 (106) |
|
CABG, coronary artery bypass graft; CR, complete revascularization; CT, clinical trials; IR, incomplete revascularization; PCI, percutaneous coronary intervention; RCP, routine clinical practice.Data are expressed as no. (%). |
|||||
DISCUSSION
The main conclusions of this study are: a) although patients potentially eligible for clinical trials receive CR more often no significant differences have been found regarding survival or adverse cardiovascular events; b) real-world patients are treated with IR more often. In these patients, less mortality has been suggested, both overall and cardiac, as well as fewer MACE at 35-month follow-up have been reported if CR is achieved; c) patients with FREEDOM clinical trial criteria have higher survival rates compared to real-world diabetics; d) most patients are treated with percutaneous coronary intervention.
One of the main problems when analyzing the repercussions of CR is the lack of clinical trials with patients similar to those found in the routine clinical practice or the real word. This complicates the extrapolation of results to the overall population since, in most studies, homogeneous participants can be found often with a better clinical profile.11,12 This reality would explain why CR does not improve the survival rate of such patients who are younger and have fewer comorbidities and cardiovascular risk factors, while in diabetics from the routine clinical practice CR does provide improvements because these are older patients with more MCAD and comorbidities (reduced ejection fraction, arterial hypertension, heart failure, peripheral arterial disease, and chronic kidney disease with, at least, a 3B stage). However, the current scientific evidence available recommends performing a therapeutic effort to achieve CR. It has been suggested that it improves survival in both overall mortality and cardiac death in real-world patients, and avoids IR that is an independent predictor of mortality (HR, 2.46; 95%CI, 1.46-4.13; P = .001).10 On the other hand, The Complete Trial9 confirmed less cardiac death and fewer new reinfarctions (HR, 0.74; 95%CI, 0.60-0.91; P = .004) when CR was performed in patients with STEACS compared to patients in whom only the culprit vessel was treated. Finally, a recent metanalysis confirmed that CR also reduces the overall mortality rate (RR, 0.73; 95%CI, 0.66-0.81), the need for new revascularizations (RR, 0.77; 95%CI, 0.66-0.88), and the occurrence of new myocardial infarctions (RR, 0.74; 95%CI, 0.64-0.85).15
In the first place, this study included diabetic patients who would not be eligible for clinical trials because they are a too heterogeneous population whose characteristics and comorbidities resemble those of real-world patients too much. Secondly, the study deals with a discussed topic these days because cardiovascular diseases, ischemic heart disease among them, are the leading cause of death in developed countries. Diabetes is especially associated with it most often leading to MCAD. Therefore, it is necessary to assess whether CR provides benefits regarding survival always focusing on the patient and his clinical-functional status because, at times, there is controversy on whether to treat all lesions or only the culprit lesions causing the problem.
Finally, if CR provides the benefits suggested in this and other studies, it could improve the survival of diabetic patients and their quality of life and that of their relatives. Also, it would reduce the health spending and the years of life lost or the disability-adjusted years of life by reducing mortality, the need for reinterventions to treat new infarctions and strokes, as well as the need for new revascularizations.
Limitations
This study was conducted from a statistical analysis of a database already used by Chueca González et al.10. It was a retrospective, single-center registry, which limits the possibilities of establishing causality and extrapolating the results to the overall population. Similarly, since the population was designed for a different study, statistical power was probably lost since the size of the sample and the characteristics of the participants included are different from the ones a study like the present one would require.
Another aspect we should mention is the technology of the stents currently used compared to those used during this study recruitment process. Since they appeared, different types and generations of stents associated with different antiproliferative drugs have been manufactured. This has improved secondary survival and minimized the occurrence of in-stent stenosis. Therefore, the study results could be different compared to those obtained today.
Finally, the definitions of CR vary based on the study. Some recommend it in the presence of > 50% occlusions of luminal diameter. Others with occlusions > 70%. In some cases, only coronary vessels with minimum diameters of 2 mm are considered. In other cases, these diameters need to be 1.5 mm. Specifically, this study only considered vessels with stenosis > 70% with minimum calibers of 2 mm.
CONCLUSIONS
This study suggests that diabetics eligible for clinical trials have fewer complications compared to non-eligible diabetic patients. Also, this suggests that real-world diabetics have worse prognosis in case of MCAD. Under this circumstance, it is suggested that achieving CR would improve their long-term survival.
In conclusion, further studies, and clinical trials including real-world patients are advised. Also, they would need to include updated diagnostic criteria and new therapeutic techniques—both pharmacological and interventional—to obtain new evidence to guide us on the therapeutic effort needed to treat patients who require coronary artery revascularization whether through angioplasty or surgery.
FUNDING
This study was funded by the Cardiovascular Biomedical Research Center Network (CB16/11/00360), Instituto de Salud Carlos III. Also, it has been co-funded by the European Regional Development Fund.
The statistical analysis of this manuscript was funded by the Chair of Advanced Therapies in Cardiovascular Diseases at Universidad de Málaga, Spain (CIF Q-2918001-E).
AUTHORS’ CONTRIBUTIONS
F. Puyol-Ruiz: study design, data curation, and drafting of the manuscript. M. Jiménez-Navarro: study design, data curation, and critical review of the manuscript. EM. Chueca-González, F. Carrasco-Chinchilla, J. L. López-Benítez, J. H. Alonso-Briales, J. M. Melero- Tejedor, and J. M. Hernández-García: data curation.
CONFLICTS OF INTEREST
None reported.
ACKNOWLEDGEMENTS
We wish to thank María Jiménez Salva for her constant support and collaboration while drafting this manuscript.
WHAT IS KNOWN ABOUT THE TOPIC?
- Due to the ageing of the population, health spending and morbidity due to ischemic heart disease and diabetes are expected to grow.
- Diabetes increases the number of cases of MCAD, which is associated with a worse prognosis.
- Results from clinical trials should be applied to real-world patients with caution.
WHAT DOES THIS STUDY ADD?
- More than half of diabetic patients with MCAD had exclusion criteria to participate in the FREEDOM clinical trial
- Real-world diabetics have a worse prognosis against MCAD.
- Anatomic CR reduces the risk of cardiac death and MACE at 35-month follow-up.
- More studies and clinical trials are needed with real-world patients.
REFERENCES
1. Roth GA, Mensah GA, Johnson CO, et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76:2982-3021.
2. Dégano IR, Elosua R, Marrugat J. Epidemiología del síndrome coronario agudo en España: estimación del número de casos y la tendencia de 2005 a 2049. Rev Esp Cardiol. 2013;66:472-481.
3. Ruiz-García A, Arranz-Martínez E, García-Álvarez JC, et al. Prevalence of diabetes mellitus in Spanish primary care setting and its association with cardiovascular risk factors and cardiovascular diseases. SIMETAP-DM study. Clin Investig Arterioscler. 2020;32:15-26.
4. Adeva-Andany MM, Funcasta-Calderón R, Fernández-Fernández C, Ameneiros-Rodríguez E, Domínguez-Montero A. Subclinical vascular disease in patients with diabetes is associated with insulin resistance. Diabetes Metab Syndr Clin Res Rev. 2019;13:2198-2206.
5. Burgess S, Juergens CP, Yang W, et al. Cardiac mortality, diabetes mellitus, and multivessel disease in ST elevation myocardial infarction. Int J Cardiol. 2021;323:13-18.
6. Hosoyama K, Maeda K, Saiki Y. What does complete revascularization mean in 2021? – Definitions, implications, and biases. Curr Opin Cardiol. 2021;36:748-754.
7. Burgess SN, French JK, Nguyen TL, et al. The impact of incomplete revascularization on early and late outcomes in ST-elevation myocardial infarction. Am Heart J. 2018;205:31-41.
8. Gaba P, Gersh BJ, Ali ZA, Moses JW, Stone GW. Complete versus incomplete coronary revascularization: definitions, assessment and outcomes. Nat Rev Cardiol. 2021;18:155-168.
9. Mehta SR, Wood DA, Storey RF, et al. Complete Revascularization with Multivessel PCI for Myocardial Infarction. N Engl J Med. 2019;381:1411-1421.
10. Chueca González EM, Carrasco Chinchilla F, López Benítez JL, et al. Enfermedad coronaria multivaso en el paciente diabético en la vida real: ¿eficacia o efectividad? REC CardioClinics. 2019;54:81-90.
11. Wasilewski J, Polon´ski L, Lekston A, et al. Who is eligible for randomized trials? A comparison between the exclusion criteria defined by the ISCHEMIA trial and 3102 real-world patients with stable coronary artery disease undergoing stent implantation in a single cardiology center. Trials. 2015;16:1-7.
12. Laursen PN, Holmvang L, Lønborg J, et al. Comparison between patients included in randomized controlled trials of ischemic heart disease and real-world data. A nationwide study. Am Heart J. 2018;204:128-138.
13. Goel SS, Shishehbor MH. Strategies for multivessel revascularization in patients with diabetes. Cardiol Rev. 2013;29:2375-2384.
14. Thygesen K, Alpert JS, Jaffe AS, et al. Documento de consenso de expertos. Tercera definición universal del infarto de miocardio. Rev Esp Cardiol. 2013;66:1-15.
15. Zimarino M, Ricci F, Romanello M, Di Nicola M, Corazzini A, De Caterina R. Complete myocardial revascularization confers a larger clinical benefit when performed with state-of-the-art techniques in high-risk patients with multivessel coronary artery disease: A meta-analysis of randomized and observational studies. Catheter Cardiovasc Interv. 2016;87:3-12.