QUESTION: What is the current status of percutaneous coronary interventions to treat functional mitral regurgitation (MR)?
ANSWER: To this date, transcatheter mitral valve repair therapies are backed by the highest scientific evidence. This has been confirmed by the new clinical practice guidelines1 on the management of patients with valve disease published by the American Heart Association (AHA) where transcatheter repair (class IIa-Level of Evidence BR) is recommended for patients with functional MR and severe ventricular dysfunction. However, surgery is spared for cases that require concomitant coronary revascularization. We should not forget that transcatheter repair is the only technique on which there are randomized clinical trials available.2,3 That is why it is indicated as the first-line therapy by the clinical practice guidelines. We should put the old sayings «regarding a case» or «in my hands, results are better» to sleep. Multicenter randomized clinical trials assess the reproducibility of the technique, and that is the key to generalize this or that therapy. In my opinion, the clinical cardiologist should place transcatheter mitral valve repair in the same level as cardiac resynchronization therapy. And, same as it happens with resynchronization, the right selection of patients is of paramount importance. When should repair be considered? In patients on optimal medical therapy who still remain symptomatic with severe functional MR, ventricular dysfunction, left ventricular end-diastolic diameter ≤ 70 mm, and with a suitable valvular anatomy as seen on the transesophageal echocardiography.
Q.: In your opinion, which would be the potential niche to combine techniques that target the leaflets or the annulus in this context?
A.: Winston Churchill used to say: « However beautiful the strategy, you should occasionally look at the results». Combined therapy is a very appealing idea, yet the experienced reported on this procedure is very limited with very few cases published to this date. It has probably encountered 2 main limitations so far: edge-to-edge mitral valve repair can alter the anteroposterior diameter of the mitral annulus and has a 5-year durability time limit compared to surgery; on the other hand, the combined procedure significantly increases risk, complexity, and the cost of the procedure.
With this mind and taking into consideration that in the future low-risk patients with primary MR will be treated, it is likely that we’ll be seeing more reports on combined cases always with the objective of increasing the repair durability.
Q.: What does interventional cardiology have to offer to patients with organic MR who are not eligible for surgery? And what about the mitral annulus?
A.: The main advantage for patients with many comorbidities is that with transcatheter repair recovery is almost immediate (to this date, the average hospital stay is 48 hours) and the rate of complications is very low; the worst thing that can happen is unsuccessful repairs. That is why the main limitation is the impossibility of valvular replacement conversion with suboptimal results (actually something cardiac surgery allows).
Mitral annular calcification does not exclude transcatheter repair, but it can make it difficult due to the presence of less flexible leaflets, thus predisposing to a higher risk of leaflet tear and a greater final transmitral gradient. However, the wide array of devices available allows us to take on situations that we would have discarded in the past. In any case, this seems like the most interesting niche for transcatheter mitral valve repair.
Q.: What degree of clinical development have transcatheter mitral valves reached so far? In your opinion, which should be their indication with respect to repair techniques?
A.: The first series with over 100 patients have already been published with positive results.4 The main limitation here is the excessive selection of patients to guarantee positive results and avoid complications like left ventricular outflow tract obstruction. Over 60% of the patients assessed are eventually considered not eligible to undergo the procedure. Regarding the indication, for the time being, it should be spared for patients in whom the repair is not feasible or may be difficult. We still need data on valvular dysfunction and thrombosis at the follow-up.
Q.: Tricuspid regurgitation (TR) is a complex condition of often unsatisfactory management. What techniques are already available for the interventional cardiologist?
A.: That is true. Unfortunately, the mortality rate of isolated surgery on the tricuspid valve is high; actually, even higher regarding its repair (mortality rate > 10%). On the other hand, medical therapy is often limited by renal function. Also, if we consider that most TRs are functional, it seems like a perfect disease to use transcatheter techniques. That is why several devices we use nowadays to treat the mitral valve are also valid to treat tricuspid regurgitation.
For repair purposes, in the MitraClip device (Abbott Vascular, United States) the delivery sheath has been changed to approach the valve easier. The Triluminate study5 used this version of the device (Triclip), and confirmed that TR was reduced by, at least, 1 grade in 86% of the patients with a 4% rate of adverse events at the 6-month follow-up. This possibility is also being explored with the Pascal device6 (Edwards Lifesciences, United States), primarily with its ACE version, and the early results are similar to those published on the Triclip. The Cardioband7 (Edwards Lifescience, United States) is also available for this use and the early experience with 30 patients reduced TR to less than moderate in 73% of the patients at the 6-month follow-up
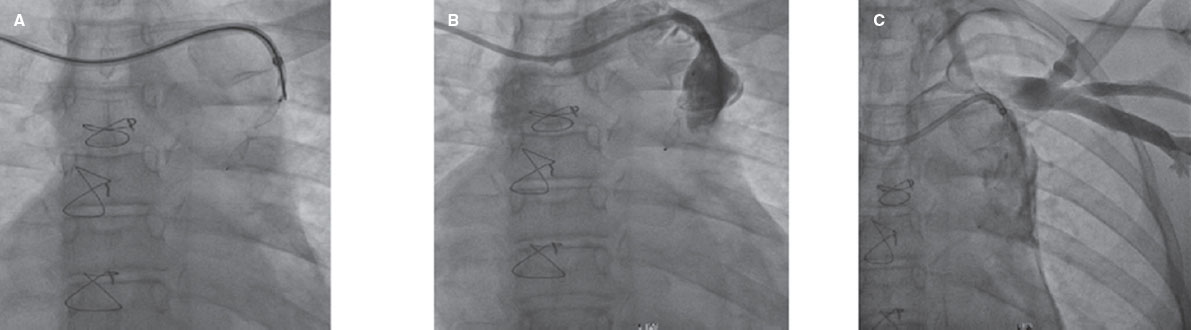
On the other hand, the field of tricuspid valve replacement is clearly heading towards the use of the femoral access almost exclusively (currently, in the mitral valve, the most consolidated valve is the Tendyne [Abbott, United States] that is implanted via transapical access). Many of the valves intended for the mitral valve are also being used in the tricuspid one where right ventricular outflow tract obstruction does not seem be a problem.
Finally, we also have heterotopic valves available that are implanted outside the thoracic cavity. The main advantage of these devices is a relatively easy implantation, and the fact that they can be used when the etiology of TR is interference with wires coming from other devices such as pacemakers, automatic implantable cardioverter-defibrillators, etc.
Q.: Which is the optimal clinical indication and anatomical context to use these techniques?
A.: The main clinical indication is patients with severe TR with signs or symptoms of right congestion that are persistent despite medical therapy and without signs of severe pulmonary arterial hypertension. In our case, the typical subject is a patient operated on the mitral valve (probably due to atrial fibrillation) who has been dilating the tricuspid annulus for years and now has severe TR that he did not have when he underwent surgery.
With respect to the anatomical context, maybe the main limiting factor regarding repairs is the echocardiographic window. It is important to know whether we will be able to achieve good projections to guarantee a proper device implantation. There are times that multimodal images including transthoracic, transesophageal or intracardiac echocardiography are required. The main limitation of edge-to-edge repair devices is the size of coaptation defect (in the Triluminate, the cut-off value was 2 cm, but the truth is that in defects > 1 cm it is already assumed that we’ll be needing more than 1 device), and in the case of the Cardioband the size of the annulus should be < 52 mm. Regarding valves, screening is performed through computed tomography scan and the limiting factor here is often the annular size. Heterotopic valves usually have very few limiting criteria.
Q.: What does the future of interventional cardiology have in store with respect to heart surgery? Where should we look into from one specialty and the other?
A.: From the medical point of view, we should probably not pay too much attention to which is the possible survival rate of this or that specialty, but where is the therapy heading to. Today’s medicine favors prevention over intervention, and the least invasive procedures over the most aggressive ones. For example, let’s look at the evolution surrounding the management of rheumatic mitral stenosis. We went from open commissurotomy as the early therapy to percutaneous valvuloplasty when it became available. However, thanks to early antithrombotic treatment there are fewer cases of mitral stenosis. This is the same path we should expect to follow with the remaining valve diseases we treat today.
We should focus on obtaining the most effective treatments causing the least possible damage to the patients. Therefore, it is our responsibility to work in order to a) use the least invasive access routes to boost the patients’ early recovery; b) minimize the impact of the learning curve of this or that therapy through early focus and the proper dissemination; c) consistently assess the results of a new therapy while being patient at the same time (and not trying to know if it is effective with the first 10 cases at the 1-month follow-up); d) be actively involved in improving the procedures (whether through patient selection, device improvement or further medical management); and finally as Hippocrates used to say «foolish the doctor who despises the knowledge acquired by the ancients», in other words, let us benefit from the cumulative experience acquired over time to avoid making the same mistakes over again.
Once a therapy has become consolidated the proper training criteria should be established to be able to perform it, which leads us directly to accreditation. The proper criteria should be established and then incorporated to the proper training, and the corresponding legal validity achieved for accreditation purposes. This can be extrapolated to all the super-specialties within the different fields of medicine. Training is well regulated from college throughout the Internal Medicine Residency (MIR) program. However, once the specialty training is over, it is necessary to regulate further training.
Maybe we should work on how to approach cardiovascular disease from an overall perspective. We should have teams working on prevention, others on diagnosis, and other teams on therapeutics. Interventional cardiology and surgery should be included in the latter group.
FUNDING
None whatsoever.
CONFLICTS OF INTEREST
D. Arzamendi is a proctor for Mitraclip and Triclip (Abbott), and Pascal (Edwards Lifescience).
REFERENCES
1. Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease:A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;14:e35-e71.
2. Stone GW, Lindenfeld J, Abraham WT, et al. Transcatheter Mitral-Valve Repair in Patients with Heart Failure. N Engl J Med. 2018;379:2307-2318.
3. Obadia J-F, Messika-Zeitoun D, Leurent G, et al. Percutaneous Repair or Medical Treatment for Secondary Mitral Regurgitation. N Engl J Med. 2018;379:2297-2306.
4. Badhwar V, Sorajja P, Duncan A, et al. Mitral regurgitation severity predicts one-year therapeutic benefit of Tendyne transcatheter mitral valve implantation. EuroIntervention. 2019;15:e1065-e1071.
5. Lurz P, Stephan von Bardeleben R, Weber M, et al. Transcatheter Edge-to-Edge Repair for Treatment of Tricuspid Regurgitation. J Am Coll Cardiol. 2021;77:229-239.
6. Lim DS, Kar S, Spargias K, et al. Transcatheter Valve Repair for Patients With Mitral Regurgitation:30-Day Results of the CLASP Study. JACC Cardiovasc Interv. 2019;12:1369-1378.
7. Nickenig G, Weber M, Schüler R, et al. Tricuspid valve repair with the Cardioband system:two-year outcomes of the multicentre, prospective TRI-REPAIR study. EuroIntervention. 2021;16:e1264-e1271.
* Corresponding author: Servicio de Cardiología, Hospital de la Santa Creu i Sant Pau, Sant Antoni Maria Claret 167, 08025 Barcelona, Spain
E-mail address: darzamendi@santpau.cat (D. Arzamendi).