ABSTRACT
Introduction and objectives: Current expert consensus guidelines recommend dual antiplatelet therapy (DAPT) with aspirin and clopidogrel as antithrombotic strategy after transcatheter aortic valve implantation (TAVI) in patients without an indication for long-term oral anticoagulation. However, these recommendations have not been developed based on the results of large randomized clinical trials. The objective of this study is to compare single antiplatelet therapy (SAPT) to DAPT in patients without an indication for long-term anticoagulation after TAVI.
Methods: The PubMed, Embase, and the main international conference proceedings were reviewed in the search for randomized controlled trials comparing SAPT to DAPT after TAVI. Data were pooled using a meta-analysis and a random-effects model. The primary endpoint was life-threatening or major bleeding.
Results: Four trials enrolling 1086 patients were included. Compared to patients treated with DAPT, those treated with SAPT showed a lower risk of life-threatening or major bleeding (OR, 0.44; 95%CI, 0.27-0.70), and any bleeding (OR, 0.51; 95%CI, 0.36-0.71). No differences were observed between patients treated with SAPT compared to those treated with DAPT regarding all-cause mortality (OR, 1.01; 95%CI, 0.61-1.68), myocardial infarction (OR, 0.50; 95%CI 0.17-1.41), and stroke (OR, 0.98; 95%CI, 0.54-1.77).
Conclusions: In patients without an indication for long-term anticoagulation undergoing TAVI, single antiplatelet therapy with aspirin compared to DAPT is associated with a lower risk of life-threatening or major bleeding and a comparable risk of all-cause mortality, myocardial infarction, and stroke.
Keywords: Antithrombotic therapy. TAVI. Antiplatelet therapy. Aspirin. Bleeding.
RESUMEN
Introducción y objetivos: Las guías de práctica clínica actuales recomiendan la terapia antiagregante plaquetaria doble con ácido acetilsalicílico y clopidogrel como estrategia antitrombótica tras el implante percutáneo de válvula aórtica (TAVI) en pacientes sin indicación de anticoagulación oral a largo plazo. Sin embargo, estas recomendaciones no se han desarrollado de acuerdo con los resultados de grandes ensayos aleatorizados. Por ello, el objetivo de esta investigación es comparar la terapia antiplaquetaria en monoterapia con el tratamiento antiagregante doble en pacientes sin indicación de anticoagulación a largo plazo después de un TAVI.
Métodos: Se realizaron búsquedas en PubMed, Embase y los principales congresos internacionales para encontrar ensayos clínicos aleatorizados que compararan el tratamiento antiagregante único con la doble terapia antiplaquetaria después de un TAVI. Los datos se agruparon en un metanálisis mediante un modelo de efectos aleatorios. El objetivo principal del estudio fue la hemorragia grave o potencialmente mortal.
Resultados: Se incluyeron cuatro ensayos que en total reclutaron 1086 pacientes. Los pacientes bajo tratamiento antiagregante en monoterapia, en comparación con aquellos con doble terapia antiplaquetaria, tuvieron menor riesgo de hemorragia grave o potencialmente mortal (odds ratio [OR] = 0,44; intervalo de confianza del 95% [IC95%], 0,27-0,70) y de cualquier sangrado (OR = 0,51; IC95%, 0,36-0,71). No se observaron diferencias entre los pacientes tratados con monoterapia y los tratados con doble terapia antiagregante en cuanto a muerte por cualquier causa (OR = 1,01; IC95%, 0,61-1,68), infarto de miocardio (OR = 0,50; IC95%: 0,17-1,41) y accidente cerebrovascular (OR = 0,98; IC95%, 0,54-1,77).
Conclusiones: En los pacientes sin indicación de anticoagulación a largo plazo sometidos a TAVI, la monoterapia con ácido acetilsalicílico en comparación con la doble terapia antiagregante se asocia con un menor riesgo de hemorragia grave o potencialmente mortal y con un riesgo comparable de muerte por cualquier causa, infarto de miocardio y accidente cerebrovascular.
Palabras clave: Tratamiento antitromb ótico. TAVI. Tratamiento antiagregante. Ácido acetilsalicílico. Sangrado.
Abbreviations DAPT: dual antiplatelet therapy. PCI: percutaneous coronary intervention. RCT: randomized clinical trial. SAPT: single antiplatelet therapy. TAVI: transcatheter aortic valve implantation.
INTRODUCTION
Over the last 20 years, transcatheter aortic valve implantation (TAVI) has emerged as a successful therapeutic alternative strategy to surgery to treat aortic valve stenosis in patients of high, intermediate, and low surgical risk.1-6
Ischemic and bleeding complications are not rare after TAVI and can be life-threatening. Recently, the PARTNER 3 and Evolut Low Risk clinical trials have shown low, yet non-negligible, incidence rates of both stroke, and major bleeding within 30 days after TAVI.5,6
As of today, dual antiplatelet therapy (DAPT) with aspirin and clopidogrel is the most commonly used antithrombotic regimen after TAVI in patients without an indication for long-term oral anticoagulation enrolled in clinical studies. Indeed, the recommendations from different societal guidelines suggest 1 to 3, 3 to 6 or 6 months of therapy with clopidogrel plus low doses of aspirin. However, such recommendations have not been developed based on the results of large randomized clinical trials.7-10 Indeed, reports on course duration over the last decade have suggested a neutral or beneficial effect of single antiplatelet therapy (SAPT) compared to early DAPT followed by SAPT regarding vascular complications and major or life-threatening bleeding and no higher risk for myocardial infarction, and stroke.11-13 Recently, aspirin alone proved superior compared to a 3-month course of aspirin plus clopidogrel followed by aspirin in terms of bleeding alone and combined with thromboembolic complications at the 1-year follow-up.14
We conducted a meta-analysis of available randomized clinical studies to provide a comprehensive and quantitative assessment of the evidence available on the safety and efficacy profile of SAPT compared to DAPT after TAVI in patients with no indication for long-term oral anticoagulation.
METHODS
Search strategy and selection criteria
Randomized clinical trials (RCTs) including patients undergoing TAVI were evaluated to be included in this meta-analysis. Eligible studies had to meet the following prespecified inclusion criteria: a) RCTs comparing SAPT to DAPT after TAVI, and b) availability of clinical outcome data. The exclusion criteria were these: a) RCTs including patients requiring oral anticoagulation, b) lack of randomized design, c) lack of any clinical outcome data.
The search strategy, study selection, data extraction, and data analysis were performed based on The Cochrane Collaboration and the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines.15
Back in August 31, 2020, we searched the PubMed and Embase databases. We also searched abstracts presented at relevant scientific meetings (American Heart Association, American College of Cardiology, European Society of Cardiology, EuroPCR, and Transcatheter Cardiovascular Therapeutics). We also used backward snowballing (ie, review of references from identified articles and pertinent reviews). The search strategy is available in the supplementary data.
Data extraction
Three investigators (J. Sanz-Sánchez, C. A. Pivato, and P. P. Leone) independently assessed studies with potential to be included. The senior investigator (G. G. Stefanini) resolved the discrepancies. Non-relevant articles were excluded based on title and abstract. The same investigators independently extracted data on the study design, measurements, patient characteristics, and outcomes, using a standardized data-extraction form. Data extraction conflicts were discussed and resolved with the senior investigator (G. G. Stefanini).
Data about the authors, year of publication, inclusion, and exclusion criteria, sample size, the patients’ baseline characteristics, endpoint definitions, effect estimates, and follow-up time were collected.
Outcomes of interest
The prespecified primary endpoint was life-threatening or major bleeding. The secondary clinical endpoints were all-cause mortality, myocardial infarction, stroke, and any bleeding. Each endpoint was assessed according to the definitions reported in the original study protocols as shown on table 1 of the supplementary data.
| Study | Year of publication | Study design | N of patients | Multicentre | Follow-up | DAPT duration | ||
|---|---|---|---|---|---|---|---|---|
| Overall | DAPT | SAPT | ||||||
| POPular TAVI14 | 2020 | RCT | 665 | 334 | 331 | Yes | 12 months | 3 months |
| ARTE11 | 2017 | RCT | 222 | 111 | 111 | Yes | 3 months | 3 months |
| SAT-TAVI12 | 2014 | RCT | 120 | 60 | 60 | No | 6 months | 6 months |
| Ussia et al.13 | 2011 | RCT | 79 | 40 | 39 | No | 6 months | 3 months |
|
DAPT, dual antiplatelet therapy; RCT, randomized clinical trial; SAPT, single antiplatelet therapy. |
||||||||
Risk of bias
The risk of bias in each study was assessed using the revised Cochrane risk-of-bias tool (RoB 2.0).16 Three investigators (J. Sanz- Sánchez, C. A. Pivato, and P. P. Leone) independently assessed 5 domains of bias in the RCTs: 1) randomization process, 2) deviations from intended interventions, 3) missing outcome data, 4) outcome measurements, and 5) selection of reported results (table 2 of the supplementary data).
Table 2. Baseline clinical characteristics of the patients included
| Study | Age (years) | Male | Diabetes | Hypertension | Atrial fibrillation | NYHA ≥ III | LVEF | STS-PROM score | Previous stroke | Previous MI | Transfemoral access | Valve-in-valve | TAVI indication: aortic stenosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| POPular TAVI14 | 80 | 50 | 24 | 75 | – | 65 | – | 2.5 | 4 | 9 | 89 | 6 | 98 |
| ARTE11 | 79 | 58 | 35 | 79 | – | – | 54 | 6.3 | – | 21 | 69 | – | – |
| SAT-TAVI12 | 81 | 37 | 27 | 95 | – | 89 | 52 | 10.0 | – | – | 100 | – | 100 |
| Ussia et al.13 | 81 | 46 | 27 | 84 | 13 | 62 | 52 | 7.3 | 8 | 14 | 97 | 0 | 100 |
| Overall | 80 | 50 | 27 | 79 | – | 68 | 53 | 4.4 | – | 12 | 87 | – | 98 |
|
LVEF, left ventricular ejection fraction; MI, myocardial infarction; NYHA, New York Heart Association; STS-PROM, Society of Thoracic Surgeons Predicted Risk Of Mortality; TAVI, transcatheter valve implantation. Data are expressed as %. |
|||||||||||||
Statistical analysis
The odds ratios (OR) and the 95% confidence intervals (CI) were calculated using the DerSimonian and Laird random-effects model with the estimate of heterogeneity being taken from the Mantel-Haenszel method. The number needed to treat (NNT) to prevent 1 event was calculated from weighted estimates of pooled ORs using the random-effects meta-analytic model. The presence of heterogeneity among the studies was evaluated using Cochran Q test based on a chi-square distribution with P values ≤ .10 considered statistically significant, and the I2 test to evaluate inconsistencies. A value of 0% indicates no observed heterogeneity, and values of ≤ 25%, ≤ 50%, > 50% are indicative of low, moderate, and high heterogeneity, respectively. The presence of publication bias was investigated by visual estimation through funnel plots. We conducted a leave-one-out sensitivity analysis for the primary endpoint by iteratively removing 1 study at a time to confirm that our findings were not driven by any single study. Further sensitivity analyses were conducted by calculating the ORs with a 95%CI using a fixed-effects model with the Mantel and Haenszel method and the risk ratios with a 95%CI using both fixed-effects and random-effects models. The statistical level of significance was 2-tailed P values < .05. Statistical analyses were performed using the Stata software version 13.1 (StataCorp LP, College Station, United States).
RESULTS
Search results
Figure 1 shows the PRISMA study search and selection process. A total of 4 RCTs were identified and included in this analysis. The main features of the studies included are shown on table 1.
Figure 1. Flowchart of the study selection process.
A total of 541 patients treated with aspirin and 545 patients treated with DAPT after TAVI were included.
Baseline characteristics
The main baseline characteristics of the patients included are shown on table 2. Most patients underwent TAVI due to aortic stenosis. The Society of Thoracic Surgeons mean predicted risk of mortality was 4.4% and most of the procedures were performed via transfemoral access.
Publication bias and asymmetry
The funnel-plot distributions of the prespecified outcomes are indicative of lack of publication bias for all the outcomes (figures 1-5 of the supplementary data).
Outcomes
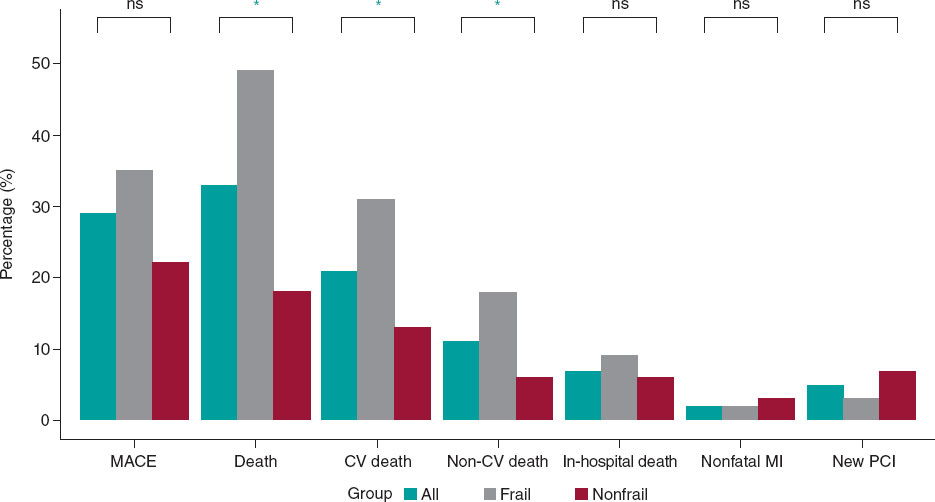
Compared to patients treated with DAPT, those treated with SAPT had a lower risk of life-threatening or major bleeding (OR, 0.44; 95%CI, 0.27-0.70; I2 = 0%), and any bleeding (OR, 0.51; 95%CI, 0.36-0.71; I2 = 0%) (figure 2). No differences were seen between patients treated with SAPT compared to those treated with DAPT in terms of all-cause mortality (OR, 1.01; 95%CI, 0.61-1.68; I2 = 0%), myocardial infarction (OR, 0.50; 95%CI, 0.17-1.41; I2 = 0%), and stroke (OR, 0.98; 95%CI, 0.54-1.77; I2 = 0%) (figure 3). The NNT to prevent 1 life-threatening or major bleeding was 17 patients and the NNT to prevent any bleeding was 11 patients.
Figure 2. Bleeding outcomes in patients treated with SAPT compared to DAPT after TAVI. DAPT, dual antiplatelet therapy; SAPT, single antiplatelet therapy; TAVI, transcatheter aortic valve implantation.
Figure 3. All-cause mortality and efficacy outcomes in patients treated with SAPT compared to DAPT after TAVI. DAPT, dual antiplatelet therapy; SAPT, single antiplatelet therapy; TAVI, transcatheter aortic valve implantation.
Risk of bias assessment
Table 2 of the supplementary data shows the results of the risk of bias assessment using the RoB 2.0 tool. Two trials were considered at a low overall risk of bias11,14 and 2 presented some concerns.12,13
Sensitivity analyses
Findings remained consistent with the main analysis after calculating the ORs using a fixed effects model and risk ratios with both fixed and random-effects models (table 3 of the supplementary data).
The leave-one-out sensitivity analysis results remained consistent with the primary analysis (table 4 of the supplementary data).
DISCUSSION
The current meta-analysis evaluated available RCTs comparing SAPT with aspirin to DAPT in patients undergoing TAVI with no indication for long-term oral anticoagulation. The main findings were these:
-
1) The risk of life-threatening or major bleeding, and any bleeding is reduced in patients treated with SAPT compared to DAPT.
-
2) The risk of all-cause mortality, myocardial infarction, and stroke did not differ between the 2 treatment strategies.
Currently, the clinical practice guidelines recommend DAPT for 1 to 6 months after TAVI in patients with no indication for long-term oral anticoagulation.7-9 However, this regimen is not supported by actual evidence available. This practice is derived from the percutaneous coronary intervention field where the addition of a P2Y12 inhibitor to aspirin compared to aspirin monotherapy proved to reduce the risk of ischemic complications especially stent thrombosis.17 The addition of clopidogrel to aspirin after TAVI has the theorical rationale of reducing the rate of ischemic cerebrovascular events, myocardial infarction, and valve thrombosis.
Ischemic stroke is one of the worst complications after TAVI. Its highest incidence rate occurs within the first 24 hours after the procedure. It seems to be mainly associated with embolized tissue waste during TAVI due to dilation of the calcified valve or navigation through the aortic arch.18-20 Instead, subacute stroke (between 1 to 30 days after the procedure)—representative of a quarter of the total number events at 2 years—4,21 are often associated with new-onset atrial fibrillation,22-24 against which DAPT is known to perform poorly.
Another motivation to prescribe DAPT after TAVI is to limit the rate of myocardial infarction. Nevertheless, the reported rate of myocardial infarction after TAVI is relatively low,4,21 and concomitant coronary artery disease is often treated percutaneously before TAVI. Therefore, the addition of a P2Y12 inhibitor to aspirin after TAVI does not seem to offer any additional advantages compared to aspirin monotherapy regarding the reduction of the risk of myocardial infarction as our results showed.
Finally, while symptomatic valve thrombosis is a rare condition (< 1%), subclinical thrombosis has a higher incidence rate (from 10% to 40% according to different series).25-27 The clinical impact of this phenomenon is still unknown: it could not only impact valve durability due to pannus formation, but it also has been associated with a higher rate of transient ischemic attack.25,26 In this setting, the pathophysiology of thrombus formation after TAVI is also still under discussion as the relative weight of primary and secondary hemostasis is still to be established. On the one hand, the endothelial injury and high shear stress environment present all around the valve stent frame before re-endothelialization may favour platelet aggregation, thus leading to the formation of a platelet-rich thrombus. This is somehow similar to what happens during coronary stent thrombosis against which the most effective treatment has proven to be DAPT.17 On the other hand, the bioprosthetic sinus of the valve leaflets could favour a condition of low shear stress and flow turbulence, thus predisposing to the development of a thrombin-rich thrombus. DAPT seems to offer no benefit over SAPT in terms of reducing bioprosthetic valve thrombosis while oral anticoagulants have proven to both prevent and resolve this complication.25-27 However, so far the only trial to assess the role of anticoagulant therapy following TAVI in patients with no indication for long-term oral anticoagulation is the Global study comparing a rivaroxaban-based antithrombotic strategy to an antiplatelet-based strategy after transcatheter aortic valve replacement to optimize clinical outcomes (GALILEO). It was stopped following relevant safety issues seen on the interim analyses revealing higher rates of complications with low doses of rivaroxaban/aspirin compared to DAPT including hard endpoints like mortality (6.8% vs 3.3%).28
Overall, ischemic events post-TAVI seem to elude the antiplatelet action provided by thienopyridines added to aspirin. A current meta-analysis confirms that the addition of a P2Y12 inhibitor does not reduce the risk of ischemic events (ie, myocardial infarction, and stroke), but most importantly predisposes patients to a higher risk of life-threatening or major bleeding. The bleeding risk reduction seen with SAPT compared to DAPT shown by this meta-analysis is of great clinical relevance, with a NNT of only 11 patients to prevent any bleeding and a NNT of 17 patients to prevent 1 life-threatening or major bleeding. Moreover, since most of the bleeding events occur within 30 days after the procedure, likely due to periprocedural antithrombotic therapy and access site bleeding complications,1-4,29 even a short-term DAPT course raises safety issues in term of bleeding events.
Based on the evidence published so far and the results of this research, in patients with no indication for long-term anticoagulation undergoing TAVI, aspirin monotherapy should be preferred over DAPT. However, larger trials are still needed to determine whether antiplatelet strategies should be tailored and based on the valve implanted (balloon-expandable vs self-expandable) or on the particular valve-in-valve implantation setting; also, to elucidate the role of alternative antiplatelet regimens (ie, P2Y12i monotherapy), and oral anticoagulants.
Limitations
The results of our study should be interpreted considering some limitations. First, this was a study-level meta-analysis that provided average treatment effects. Also, the lack of patient-level data from the studies included data prevents us from assessing the impact baseline clinical and procedural characteristics had on treatment effects. Secondly, minor differences in the definition used were present in the ischemic endpoints, thus limiting the reliability of the effect estimates. However, in terms of the bleeding endpoints, the VARC definition was used in all the studies included, which adds to the robustness of our findings. Finally, the limited number of studies and patients as well as the small event rate for certain endpoints such as myocardial infarction may have reduced the statistical power to detect any significant inter-group differences.
Additional evidence will be provided by ongoing randomized trials: the Antithrombotic strategy after trans-aortic valve implantation for aortic stenosis (ATLANTIS, NCT02664649) trial will evaluate the benefit of apixaban therapy (standard dose) vs standard of care; the Anticoagulant versus dual antiplatelet therapy for preventing leaflet thrombosis and cerebral embolization after transcatheter aortic valve replacement (ADAPT-TAVR, NCT03284827) trial will compare edoxaban (standard dose) vs DAPT. Finally, the Dual antiplatelet therapy versus oral anticoagulation for a short time to prevent cerebral embolism after TAVI (AUREA, NCT01642134) trial will study a strategy of vitamin K antagonist vs a 3-month course of DAPT.
CONCLUSIONS
In patients without an indication for long-term anticoagulation undergoing TAVI, monotherapy with aspirin compared to DAPT is associated with a lower risk of life-threatening or major bleeding, and a comparable risk of all-cause mortality, myocardial infarction, and stroke.
FUNDING
None.
AUTHORS’ CONTRIBUTIONS
J. Sanz-Sánchez, C. A. Pivato, P. P. Leone, and M. Chiarito con- tributed to the design, analysis, and writing of this manuscript. D. Regazzoli, and G. Petriello contributed to the design, and writing of this manuscript too. B. Reimers, G. Condorelli, and G. G. Stefanini contributed to the study design, writing, and supervision.
CONFLICTS OF INTEREST
G. G. Stefanini reported a research grant from Boston Scientific, and speaker/consulting fees from B. Braun, Biosensors, and Boston Scientific. D. Regazzoli reported speaker fees from Amgen, and Boehringer. The remaining authors declared no conflicts of interest whatsoever.
What is known about the topic?
- Ischemic and bleeding complications are not rare after TAVI and can be life-threatening. To reduce the rate of stroke, myocardial infarction, and valve thrombosis, the clinical practice guidelines recommend a 1 to 6 month DAPT course after TAVI in patients with no indication for long-term oral anticoagulation. However, this regimen is not supported by the current evidence and overall, ischemic events post-TAVI seem to elude the antiplatelet action provided by thienopyridines added to aspirin. Indeed, reports on therapy duration over the last decade have suggested a neutral or beneficial effect of aspirin monotherapy compared to early DAPT followed by aspirin regarding vascular complications, and major or life-threatening bleedings.
What does this study add?
- The present study confirms that the addition of thienopyridines added to aspirin does not reduce the risk of ischemic events (namely myocardial infarction, and stroke). Instead it predisposes patients to an increased risk of life-threatening or major bleeding. The bleeding risk reduction with aspirin compared to DAPT is of great clinical relevance, with a NNT of only 11 patients to prevent any bleeding and a NNT of 17 patients to prevent 1 life-threatening or major bleeding. Based on the evidence published so far and the results of this study, in patients without an indication for long-term anticoagulation undergoing TAVI, aspirin monotherapy should be preferred over DAPT.
REFERENCES
1. Leon MB, Smith CR, Mack M, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010;363:1597-1607.
2. Smith CR, Leon MB, Mack MJ, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011;364:2187-2198.
3. Adams DH, Popma JJ, Reardon MJ, et al. Transcatheter aortic-valve replacement with a self-expanding prosthesis. N Engl J Med. 2014;370:1790-1798.
4. Leon MB, Smith CR, Mack MJ, et al. Transcatheter or Surgical Aortic-Valve Replacement in Intermediate-Risk Patients. N Engl J Med. 2016;374:1609-1620.
5. Popma JJ, Deeb GM, Yakubov SJ, et al. Transcatheter Aortic-Valve Replacement with a Self-Expanding Valve in Low-Risk Patients. N Engl J Med. 2019:NEJMoa1816885.
6. Mack MJ, Leon MB, Thourani VH, et al. Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med. 2019;380:1695-705.
7. Baumgartner H, Falk V, Bax JJ, et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2017;38:2739-2791.
8. Webb J, Rodés-Cabau J, Fremes S, et al. Transcatheter Aortic Valve Implantation:A Canadian Cardiovascular Society Position Statement. Can J Cardiol. 2012;28:520-528.
9. Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients with Valvular Heart Disease:A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135:e1159-1195.
10. Mangieri A, Jabbour RJ, Montalto C, et al. Single-Antiplatelet Therapy in Patients with Contraindication to Dual-Antiplatelet Therapy After Transcatheter Aortic Valve Implantation. Am J Cardiol. 2017;119:1088-1093.
11. Rodés-Cabau J, Masson JB, Welsh RC, et al. Aspirin Versus Aspirin Plus Clopidogrel as Antithrombotic Treatment Following Transcatheter Aortic Valve Replacement With a Balloon-Expandable Valve:The ARTE (Aspirin Versus Aspirin +Clopidogrel Following Transcatheter Aortic Valve Implantation) Randomized Clinical Trial. JACC Cardiovasc Interv. 2017;10:1357-1365.
12. Stabile E, Pucciarelli A, Cota L, et al. SAT-TAVI (single antiplatelet therapy for TAVI) study:A pilot randomized study comparing double to single antiplatelet therapy for transcatheter aortic valve implantation. Int J Cardiol. 2014;174:624-627.
13. Ussia GP, Scarabelli M, Mul M, et al. Dual antiplatelet therapy versus aspirin alone in patients undergoing transcatheter aortic valve implantation. Am J Cardiol. 2011;108:1772-1776.
14. Brouwer J, Nijenhuis VJ, Delewi R, et al. Aspirin with or without Clopidogrel after Transcatheter Aortic-Valve Implantation. N Engl J Med. 2020:NEJMoa2017815–NEJMoa2017815.
15. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions:explanation and elaboration. BMJ. 2009;339:b2700.
16. Risk of bias tools - Current version of RoB 2 n.d. https://www.riskofbias.info/welcome/rob-2-0-tool/current-version-of-rob-2. Accessed 23 June 2019.
17. Stefanini GG, Holmes DR. Drug-Eluting Coronary-Artery Stents. N Engl J Med. 2013;368:254-265.
18. Van Mieghem NM, El Faquir N, Rahhab Z, et al. Incidence and predictors of debris embolizing to the brain during transcatheter aortic valve implantation. JACC Cardiovasc Interv. 2015;8:718-724.
19. Schmidt T, Leon MB, Mehran R, et al. Debris Heterogeneity Across Different Valve Types Captured by a Cerebral Protection System During Transcatheter Aortic Valve Replacement. JACC Cardiovasc Interv. 2018;11:1262-1273.
20. Kahlert P, Al-Rashid F, Döttger P, et al. Cerebral embolization during transcatheter aortic valve implantation:A transcranial doppler study. Circulation. 2012;126:1245-1255.
21. Reardon MJ, Van Mieghem NM, Popma JJ, et al. Surgical or transcatheter aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2017;376:1321-1331.
22. Nombela-Franco L, Webb JG, De Jaegere PP, et al. Timing, predictive factors, and prognostic value of cerebrovascular events in a large cohort of patients undergoing transcatheter aortic valve implantation. Circulation. 2012;126:3041-3053.
23. Siontis GCM, Praz F, Lanz J, et al. New-onset arrhythmias following transcatheter aortic valve implantation:A systematic review and meta-analysis. Heart. 2018;104:1208-1215.
24. Vora AN, Dai D, Matsuoka R, et al. Incidence, Management, and Associated Clinical Outcomes of New-Onset Atrial Fibrillation Following Transcatheter Aortic Valve Replacement:An Analysis From the STS/ACC TVT Registry. JACC Cardiovasc Interv. 2018;11:1746-1756.
25. Makkar RR, Fontana G, Jilaihawi H, et al. Possible subclinical leaflet thrombosis in bioprosthetic aortic valves. N Engl J Med. 2015;373:2015-2024.
26. Chakravarty T, Søndergaard L, Friedman J, et al. Subclinical leaflet thrombosis in surgical and transcatheter bioprosthetic aortic valves:an observational study. Lancet. 2017;389:2383-2392.
27. Pache G, Schoechlin S, Blanke P, et al. Early hypo-attenuated leaflet thickening in balloon-expandable transcatheter aortic heart valves. Eur Heart J. 2016;37:2263-2271.
28. Dangas GD, Tijssen JGP, Wöhrle J, et al. A controlled trial of rivaroxaban after transcatheter aortic-valve replacement. N Engl J Med. 2020;382:120-129.
29. Piccolo R, Pilgrim T, Franzone A, et al. Frequency, Timing, and Impact of Access-Site and Non–Access-Site Bleeding on Mortality Among Patients Undergoing Transcatheter Aortic Valve Replacement. JACC Cardiovasc Interv. 2017;10:1436-1446.
* Corresponding author: Department of Biomedical Sciences, Humanitas University, Via Rita Levi Montalcini 4, Pieve Emanuele - Milan, Italy.
E-mail address: giulio.stefanini@gmail.com (G. G. Stefanini).