To the Editor,
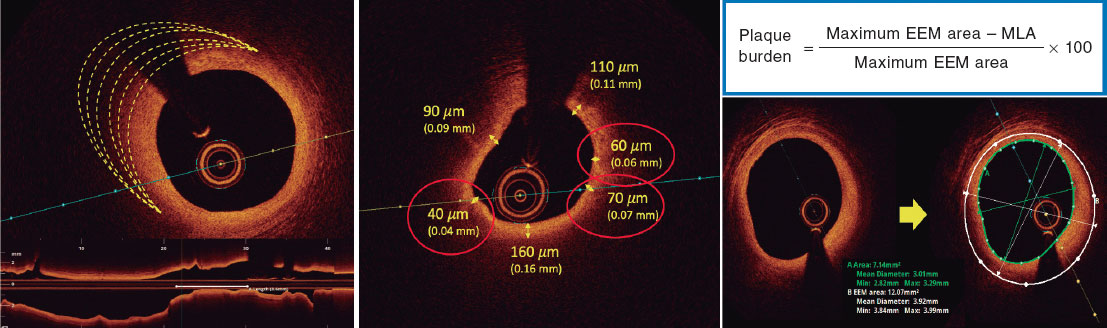
Coronary artery disease due to sustained inflammation and the effects of calcification promoters is the leading cause of morbidity and mortality in patients with chronic kidney disease.1,2 When seen on the optical coherence tomography, the atheromatous plaques of these patients show features of vulnerability.3 The prevalence or kidney disease (KD) in patients with acute coronary syndrome is up to 30% and is an independent predictor of both ischemic and hemorrhagic adverse events.1 However, the evidence available on the prognostic impact of KD in patients with ST-segment elevation acute myocardial infarction treated with a primary angioplasty is scarce.4-8
Our objective was to assess the long-term and in-hospital prognosis (5-year follow-up) of a single-center, retrospective cohort of patients who underwent a primary angioplasty between 2007 and 2014. We assessed the frequency of the composite endpoint of dead, stroke or non-fatal acute myocardial infarction and major bleeding (Bleeding Academic Research Consortium [BARC] type 3 or 5). It was based on the presence of KD defined as an estimated glomerular filtration rate ≤ 60 mL/min/1.73 m2 according to the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation and taking the serum creatinine levels obtained immediately before the current admission as reference values.
The Student t test was used for mean comparison purposes and the chi-square test was used to compare proportions. The variables predictive of the composite endpoint with P values < .05 in the univariate analysis (age, sex, arterial hypertension, smoking, and previous ischemic heart disease) were included in a multivariate logistic regression analysis with likelihood-ratio test. Patients gave their verbal consent for the use of data derived from hospitalization and follow-up for teaching and scientific purposes.
A total of 826 out of 1622 primary angioplasties were included (51% without previous creatinine levels). A total of 21.8% had KD and follow-up was completed in 567 patients (222 were lost to follow-up). The baseline characteristics are shown on table 1 (how patients with KD actually had a higher risk profile and more comorbidities). Stent thrombosis was the leading cause of acute myocardial infarction (5% vs 1.1%; P = .01).
Table 1. Baseline characteristics, prognosis, and predictors of adverse events
| Baseline characteristics | |||||
|---|---|---|---|---|---|
| Total (N = 826) | eGFR ≤ 60 mL/min (N = 180) | eGFR > 60 mL/min (N = 646) | P | ||
| Age | 71.3 ± 8.3 | 78.2 ± 9.5 | 62.0 ± 12.5 | < .01 | |
| Feminine sex | 21% | 32.2% | 17.8% | < .01 | |
| Arterial hypertension | 60% | 80% | 54.6% | < .01 | |
| Diabetes mellitus | 28.6% | 31.7% | 27.7% | .29 | |
| Dyslipidemia | 43.5% | 44.4% | 43.2% | .76 | |
| Active smoker | 39.8% | 11.7% | 47.7% | < .01 | |
| Atrial fibrillation | 9% | 18.2% | 6.8% | .002 | |
| Previous IHD | 11.6% | 17.8% | 9.9% | .004 | |
| Peripheral arteriopathy | 8.5% | 14.4% | 6.8% | .001 | |
| Previous revascularization | 13.6% | 23.8% | 10.8% | .007 | |
| Prognosis KD vs no KDa | |||||
| Total | eGFR ≤ 60 mL/min/1.73 m2 | eGFR > 60 mL/min/1.73 m2 | P | ||
| Composite endpointa | Admission | 6% | 13.9% | 3.9% | < .005 |
| 1 year | 14.5% | 23% | 11.9% | .005 | |
| 3 years | 23% | 33.3% | 20.5% | .007 | |
| 5 years | 32.1% | 47.8% | 28.9% | .001 | |
| Overall mortality rate (CV) | Admission | 4.5% (3.9%) | 10.2% (8.33%) | 3% (2.63%) | < .0001 (.05) |
| 1 year | 6% (1.4%) | 11.7% (3.5%) | 4.4% (0.8%) | .007 (.05) | |
| 3 years | 9% (2.1%) | 17.4% (6.6%) | 7.3% (1.2%) | .004 (.004) | |
| 5 years | 23% (5%) | 41.8% (15.8%) | 19.1% (2.6%) | .001 (.01) | |
| BARC type 3 or 5 bleeding | Admission | 3.8% | 8.9% | 2.5% | < .001 |
| Multivariate analysisb | |||||
| Variable | Admission | 1 year | 3 years | 5 years | |
| Arterial hypertension | 1.9 (1.1-3.5; P= .02) | 1.7 (0.9-3.1; P= .06) | 1.8 (1.1-3; P= .02) | 1.9 (1.2-3; P= .09) | |
| Previous IHD | 3.9 (2.02-7.5; P< .001) | 3.5 (1.7-7.1; P< .001) | 2.7 (1.4-5.4; P= .03) | 1.7 (0.7-3.7; P= .18) | |
| KD | 5.9 (2.7-12.6; P< .001) | 1.95 (1.1-3.6; P= .03) | 2.04 (1.2-3.5; P= .01) | 2.2 (1.3-3.7; P= .03) | |
|
BARC, Bleeding Academic Research Consortium; CV, cardiovascular; eGFR, estimated glomerular filtration rate; IHD, ischemic heart disease; KD, kidney disease. a Death, stroke or non-fatal acute myocardial infarction. b Multivariate analysis (odds ratio with 95% confidence interval and Cox model P values. |
|||||
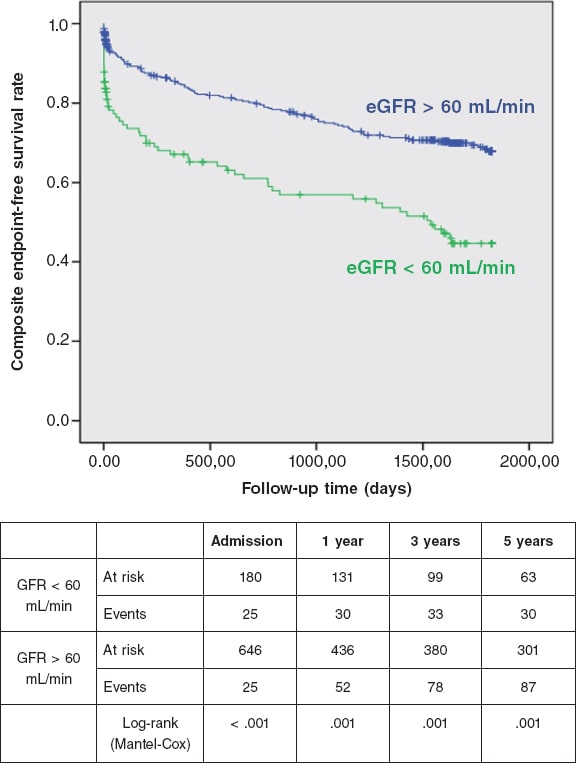
During the admission and the long-term follow-up, patients with KD more often showed the composite endpoint and a higher mortality rate, mainly cardiovascular. Also, KD was associated with the occurrence of major bleeding. Similarly, in the multivariate analysis, KD was a strong independent predictor of events in all the periods studied, especially in-hospital. Previous arterial hypertension and ischemic heart disease were also independent predictors of the composite endpoint (table 1 and figure 1).
Figure 1. Survival curves after 5 years based on the presence or absence of kidney disease. eGFR, estimated glomerular filtration rate.
In their last iteration, the European clinical practice guidelines on the management of coronary heart disease, both chronic and acute, have compared patients with KD to diabetic patients regarding their high cardiovascular risk. However, there are no solid recommendations on this regard since these patients have traditionally been excluded from most clinical trials in this field. In the primary angioplasty setting, KD affects 1 out of 5 patients,4-8 with an up to 9 times higher in-hospital mortality rate and a 5 times higher 3-year mortality rate.4 Different causes for this have been postulated: higher comorbidity, metabolic alterations, chronic inflammation, oxidative stress, and endothelial dysfunction as contributors to a greater spread, progression, and complexity of coronary artery disease. Also, the underuse of drugs that have proven capable of increasing survival after an acute myocardial infarction.1,2 On the other hand, chronic kidney disease is one of the most powerful predictors of bleeding and a known risk factor of stent thrombosis (findings we also saw). This adds more complexity to the antithrombotic management of patients with KD though further research is still needed on this issue.2
In a practical way, our observations show that the identification of patients with estimated glomerular filtration rates < 60 mL/min based on the last known serum creatinine levels is an easy and effective approach to their risk of poor progression during admission, which extends up to 5 years. This strategy would allow us to take strict precautions like nephroprotection, intensive control of other cardiovascular risk factors, close follow-up, and individual treatments.
As one of the limitations we should mention that 51% of the patients were excluded because their previous creatinine levels were not available, which may have been a selection bias.
We hope future studies will shed light on the optimal treatment for a subgroup of patients on which there are still too many shadows of evidence.
FUNDING
No funding was received for this work.
AUTHORS' CONTRIBUTIONS
The text has been prepared and revised with the participation of all signatory authors.
CONFLICTS OF INTEREST
None.
REFERENCES
1. Cai Q, Mukku V, Ahmad M. Coronary Artery Disease in Patients with Chronic Kidney Disease:A Clinical Update. Curr Cardiol Rev. 2013;9:331-339.
2. Sarnak MJ, Amann K, Bangalore S, et al. Chronic kidney disease and coronary artery disease. J Am Coll Cardiol. 2019;74:1823-1838.
3. Kato K, Yonetsu T, Jia H, et al. Nonculprit coronary plaque characteristics of chronic kidney disease. Circ Cardiovasc Imaging. 2013;6:448-456.
4. Sadeghi HM, Stone GW, Grines CL, et al. Impact of Renal Insufficiency in Patients Undergoing Primary Angioplasty for Acute Myocardial Infarction. Circulation. 2003;108:2769-2775.
5. Gibson CM, Pinto DS, Murphy SA, et al. Association of Creatinine and Creatinine Clearance on Presentation in Acute Myocardial Infarction With Subsequent Mortality. J Am Coll Cardiol. 2003;42:1535-1543.
6. Anavekar NS, McMurray JJV, Velazquez EJ, et al. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med. 2004;351:1285-1295.
7. Saltzman AJ, Stone GW, Claessen BE, et al. Long-term impact of chronic kidney disease in patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention:the HORIZONS-AMI (Harmonizing Outcomes With Revascularization and Stents in Acute Myocardial Infarction) trial. JACC Cardiovasc Interv. 2011;4:1011-1019.
8. Vavalle JP, van Diepen S, Clare RM, et al. Renal failure in patients with ST-segment elevation acute myocardial infarction treated with primary percutaneous coronary intervention:Predictors, clinical and angiographic features, and outcomes. Am Heart J. 2016;173:57-66.
Corresponding author: Servicio de Cardiología, Hospital Universitari de Bellvitge, Feixa Llarga s/n, 08907 L’Hospitalet de Llobregat, Barcelona, Spain
E-mail addresses: bsanchezmarisa@gmail.com; mbarrionuevo@bellvitgehospital.cat (M.I. Barrionuevo Sánchez).