QUESTION: What relevant evidence could support aortic valve replacement today in cases of true severe asymptomatic aortic stenosis? Are there any studies on both techniques, surgery and transcatheter implantation?
ANSWER: Ross and Braunwald’s1 description of the outcomes of patients with severe symptomatic aortic stenosis (AS) almost 60 years ago laid the foundations for the indication for surgery—the first-line therapy to date—to treat this disease, although transcatheter aortic valve implantation (TAVI) is also indicated. At a time when surgery was the only therapeutic option available, with mortality rates close to 3% to 4%, nobody thought of treating asymptomatic patients, who had a risk of sudden death of nearly 1%. These findings were confirmed by later studies, and the treatment of asymptomatic AS continued to lack evidence until the first decade of the 21st century when observational studies with small series of patients with severe asymptomatic AS (Vmax ≥ 4 m/s and mean gradient ≥ 40 mmHg) began to be published. In all of them, the results favored early surgical treatment. In the study of 197 patients by Kang et al.,2 the primary endpoint was a composite of operative and follow-up mortality. The 6-year cardiac and all-cause mortality rates were 0% and 2 ± 1% in the surgical group compared with 24 ± 15% to 32 ± 6% in the conservative treatment group. The CURRENT AS3 registry of Taniguchi et al, with 1808 patients (291 in the surgical group and 1517 in the conservative treatment group) favored the surgical group in terms of overall mortality (15.4% vs 26.4%; P < .009) and heart failure-related admissions (3.8% vs 19.9%; P < .0001). The only randomized clinical trials published to date comparing conservative vs surgical treatment are the RECOVERY4 and the AVATAR5 trials, both with a small number of patients (145 and 157, respectively), and both with results favorable to surgery. In the RECOVERY trial, the primary endpoint was a composite of procedural and cardiovascular mortality during follow-up, with rates of 1% in the surgical group and 15% in the conservative treatment group (hazard ratio [HR], 0.09; 95%CI, 0.01-0.67). The 4- and 8-year cumulative incidence rates of the primary endpoint remained at 1% in the surgical group vs 6% and 26% (P = .003) in the conservative treatment group. In the AVATAR trial, the primary endpoint was a composite of all-cause mortality, myocardial infarction, stroke, or unplanned heart failure-related admission, with rates of 15.22% and 34.7% at the 3-year follow-up (HR, 0.46; 95%CI, 0.23-0.9).
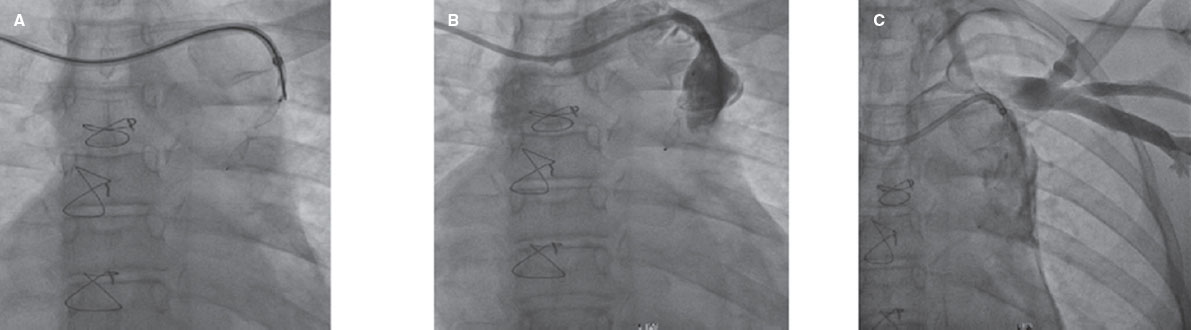
The first TAVI was performed back in 2002. Since then, we have come a long way regarding indications—although it’s only a short time—because in 20 years, TAVI has been recognized as the treatment of choice for inoperable and high surgical risk patients, with similar results compared to those of surgery in moderate and low surgical risk patients. These trials have focused on symptomatic patients. Several trials are under way in asymptomatic patients, EARLY TAVR (NCT03042104) and EVOLVED (NCT03094143), and their results will be published soon, but until then, the only evidence to date supporting treatment in asymptomatic patients is surgical.
Q.: When the decision is made to intervene in cases of severe asymptomatic aortic stenosis, on what grounds should the choice be made between surgery and TAVI? Would it be any different from the choice in a symptomatic case?
A.: The current clinical guidelines on the management valvular heart disease of the European Society of Cardiology6 still focus on the indication for treating AS based on symptoms; asymptomatic AS is not included in this indication, unless there are laboratory or echocardiographic predictors of rapid symptom progression. As explained earlier, there is currently more evidence on surgery in asymptomatic patients. However, a more in-depth analysis of the studies reveals 2 important facts. One is that the mean age was generally low: 65 years in the RECOVERY trial and 68 years in the AVATAR trial, and was very similar in registries. The other is that the causes of AS are highly variable: in the RECOVERY trial, 61% of the patients had bicuspid valves, 33% degenerative valves, and 6% rheumatic valves. In the AVATAR trial, 84.7% had degenerative valves, 14% bicuspid valves, and 1% rheumatic valves.
In Spain, where life expectancy is one of the longest worldwide—82 years in men and 87 years in women in 2023—most patients treated with TAVI have degenerative AS, and the incidence of bicuspid valves is lower than that reported by studies, which means that using the same criteria is challenging. However, it seems clear that severe or very severe AS, as included in the studies, shows better mid- and long-term survival rates when treated early, while asymptomatic. The severity criteria included in the studies (Vmax ≥ 4.5 m/s, mean gradient ≥ 50 mmHg) help us select those patients who benefit the most from early treatment. On the issue on what treatment we should use (surgery or TAVI), the decision is more complicated due to the lack of evidence on TAVI. As mentioned earlier, the average patients we treat are octogenarians. In some cases, AS is found during a routine examination, and if they are truly asymptomatic (because octogenarians often cut down on activity and have difficulty recognizing their own physical limitations) and meet severity criteria, an early intervention will result in better quality of life and fewer procedural complications. In my opinion, applying the same criteria used with symptomatic patients is beneficial for patients, meaning that, in patients with low-to moderate surgical risk, if we accept the results of TAVI trials,6-8 the transcatheter option is entirely acceptable. A different type of patient are those under follow-up because they have bicuspid valves or rheumatic disease. These patients are often younger and the indication for surgical valve replacement is clearer because TAVI still has limitations that need to be resolved in terms of durability, the need for new procedures if there is prosthetic valve degeneration, access to coronary arteries, and the treatment of bicuspid valves, which also remains poorly established. Additionally, TAVI is associated with a higher rate of pacemaker implantation, which, in young patients, is related to new comorbidities and various effects on ventricular function.
Therefore, the choice would be TAVI for octogenarians and surgery for younger patients. I would set patients from 75 to 80 years apart who could potentially receive transcatheter treatment based on their own preferences.
On the issue of whether treatment would differ in asymptomatic compared with symptomatic patients, in my opinion, this would not be the case. AS is a continuum in which symptoms appear sooner or later. Although it seems that we can base our decisions on evidence when treating symptomatic AS, we have to think that the benefit to the patient is greater as physical and pathophysiological conditions will always be better before symptom onset. In fact, sometimes the changes triggered by symptomatic AS can be irreversible. Treating asymptomatic patients requires both us and surgeons, who have already reduced mortality down to 1% in these patients, more meticulous approaches regarding valve selection and implantation, correctly selecting the valve while minimizing risks and complications, since patients should benefit in the short- and long-term.
Q.: Any considerations on the TAVI technique that should be used in these cases?
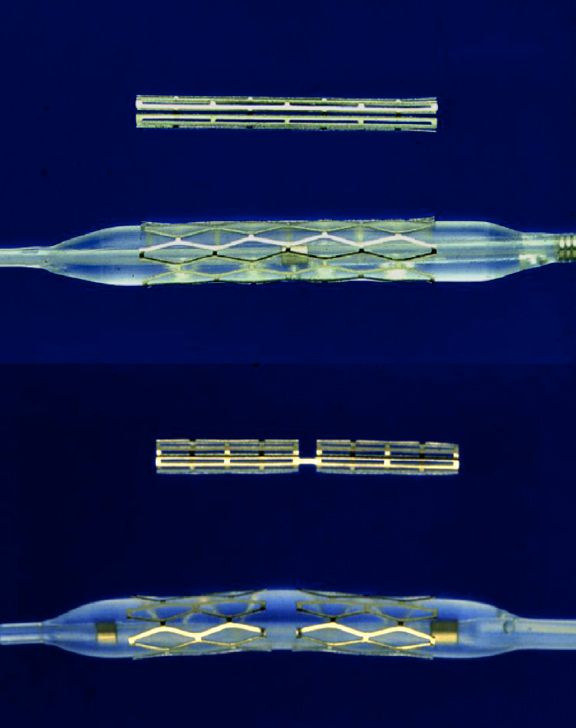
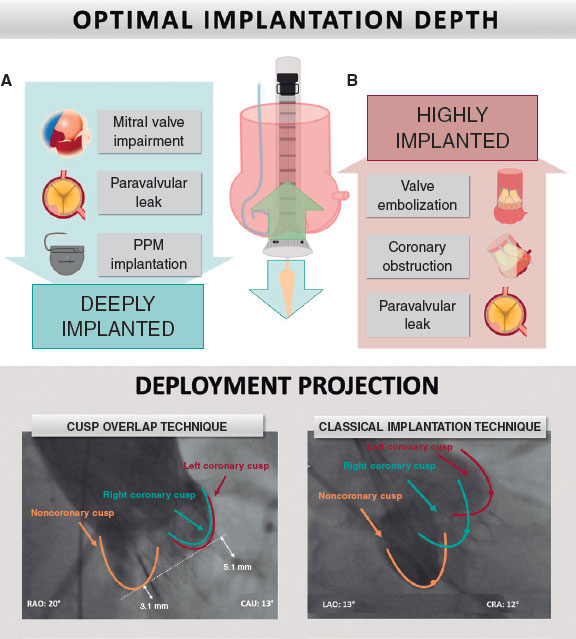
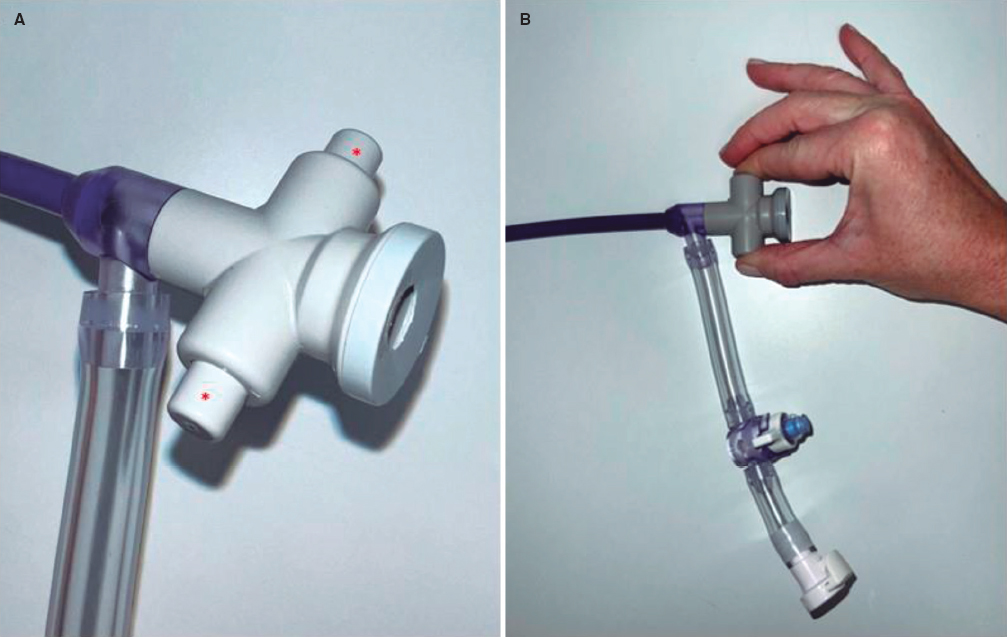
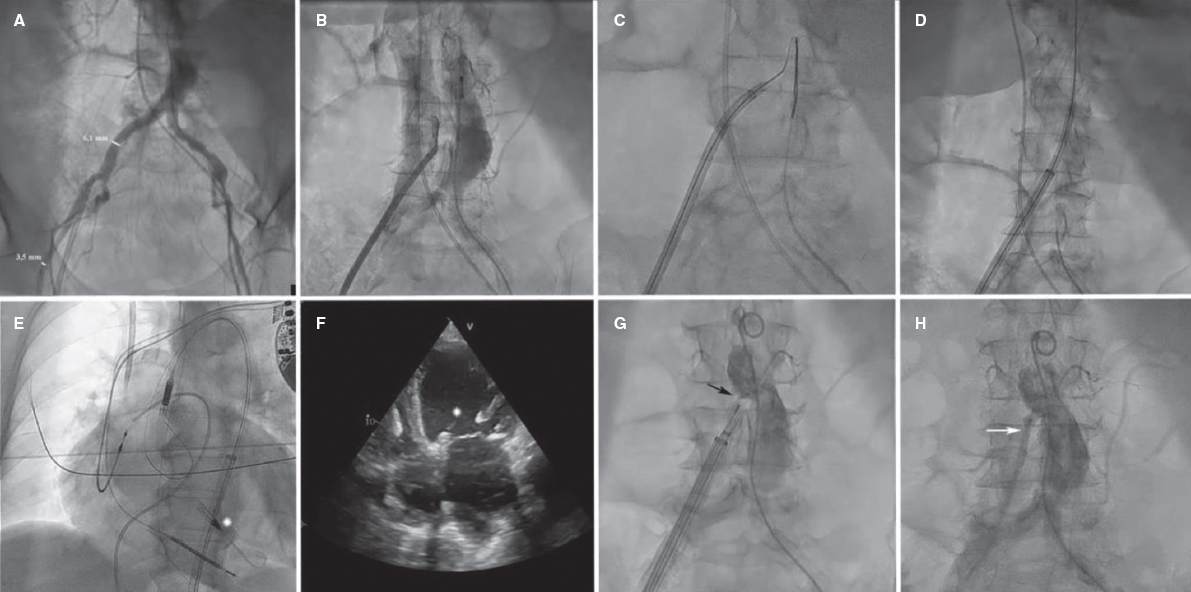
A.: When we decide to perform TAVI in a symptomatic patient, we assess the anatomical and clinical factors involved. The same applies to asymptomatic patients: on the one hand, if the patient is young and has a bicuspid valve, the valve selected should have enough radial strength, a low pacemaker implantation rate, and give us room to plan a second TAVI in the future while securing access to the coronary arteries. If a self-expanding supra-annular valve is selected, the current tendency is to place the prosthetic valve as high as possible with respect to the annulus to minimize the risk of pacemaker implantation. This may compromise access to the coronary arteries, which is why, commissural alignment should be attempted, as far as possible. To avoid complications such as stroke, which can be devastating in young patients, the use of embolic protection devices is justified, although the only randomized clinical trial published to date has not shown any benefits in specific subgroups for stroke in general (primary endpoint) as opposed to disabling stroke (not the primary endpoint). In older asymptomatic patients with degenerative AS, the implantation technique follows the same pattern used with symptomatic patients.
Q.: What is the current management of these patients in your center?
A.: At the Álvaro Cunqueiro Hospital, all patients are discussed in a heart team session, where the treatment criteria are more or less clear. Asymptomatic patients come through various routes: one is patients with valvular heart disease under clinical surveillance who develop severity criteria during follow-up. If the patient is older than 80 years, the decision is often to use the transcatheter approach, from 75 to 79 years, either of the 2 treatments would be fine, and the patient’s preference is a consideration, and if the patient is younger than 75 years, the decision is often to perform surgical valve replacement. Patients with bicuspid valves are often young and initially referred for surgical treatment.
In other patients, AS is found during routine examination due to another disease. Here, there’s a subgroup that requires quick decision-making: patients with neoplasms or interventions that cannot be delayed for too long. In these cases, transcatheter treatment is the chosen one because implantation is possible once the results from the computed tomography become available. The intervention is performed within the next few days, with rapid recovery, before the next intervention. If the patient is young and has a bicuspid valve, a balloon-expandable valve is often used. If the patient is older and doesn’t have coronary artery disease, a self-expanding valve is used. If the patient has coronary artery disease to be treated after the intervention, if necessary, a self-expanding valve with easy access to the coronary arteries is often implanted. If vascular access is suboptimal, a self-expanding valve is also the preferred choice due to its better profile.
If asymptomatic patients don’t have any other conditions requiring immediate treatment, they are treated as if they were symptomatic patients, except for patients with criteria of very severe AS (Vmax ≥ 5 m/s, mean gradient ≥ 60 mm Hg, and progression of Vmax ≥ 0.3 m/s/year), who are treated preferentially.
FUNDING
None declared.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCE
No artificial intelligence has been used in the preparation of this work.
CONFLICTS OF INTEREST
J. A. Baz Alonso is a proctor for Biosensors for the Allegra valve implantation, and advisor to Medtronic Iberia on structural heart diseases.
REFERENCES
1. Ross J, Braunwald E. Aortic stenosis. Circulation. 1968;38 suppl V:61-67.
2. Kang DH, Park SCJ, Rim JH, et al. Early surgery versus conventional treatment in asymptomatic very severe aortic stenosis. Circulation. 2010;121:1502-1509.
3. Taniguchi T, Morimoto T, Shiomi H, et al. Initial surgical versus conservative strategies in patients with asymptomatic severe aortic stenosis. J Am Coll Cardiol. 2015;66:2827-2838.
4. Kang D-H, Park S-J, Lee S-A, et al. Early surgery or conservative care for asymptomatic aortic stenosis. N Engl J Med. 2020;382:111-119.
5. Banovic M, Putnik S, Penicka M, et al. Aortic valve replacement versus conservative treatment in asymptomatic severe aortic stenosis:the AVATAR trial. Circulation. 2022;145:648-658.
6. Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2022;43:561-632.
7. Popma JJ, Deeb GM, Yakubov SJ, et al. Evolut Low Risk Trial Investigators. Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N Engl J Med. 2019;380:1706-1715.
8. Mack MJ, Leon MB, Thourani VH, et al. Transcatheter aortic-valve replacement with a balloon-expandable valve in low risk patients. N Engl J Med. 2019;380:1695-1705.
* Corresponding author.
E-mail address: joseantoniobaz@gmail.com (J.A. Baz Alonso).