To the Editor,
Over the last few years the number of procedures that have been broadcast live—often at medical meetings—has been growing exponentially. Still, this is a controversial issue.1,2 In cardiology, the very first case of a coronary angioplasty broadcast live took place in Zurich back in 1980.1,2
Some say that there is a potential risk for patients, and they share different arguments claiming that live broadcasts may bring no educational benefits at all compared to cases already filmed or recorded. Added to the technical complexity involved, there would be more pressure to the operators themselves. However, others are true defenders of these broadcasts mentioning their educational value when performed correctly with selected cases claiming that this should not be detrimental at all to results or safety.3,4 Thus, the VERITAS study compared 60 transcatheter aortic valve implantation (TAVI) broadcasts to 42 similar control procedures and concluded that, if performed by experienced operators, broadcasting TAVI procedures live is safe and results are similar to the usual ones.4
Also, consensus documents have been published with recommendations, and several meetings have been held and hosted by the European Society of Cardiology (VITAL-Live2) to define how courses with live cases should work.3
The primary endpoint of this study was to know the expert opinion on the procedures that are broadcast live in medical meetings and those that are performed for the general public. The study secondary endpoint was to conduct a stratified analysis based on the professional profile (sex, years of experience, field of expertise, etc.) A brief survey in English and Google-forms format was e-mailed to 360 health professionals (from the specialties of cardiology, hemodynamics, electrophysiology, cardiac surgery, and anesthesia) of different countries. The scores given were ranked from 1 to 5 being 1 the worst score of all and 5 the best score of all (more safety and more educational value). Respondents sent back the survey in September 16, 2019 and no further reminders were sent.
Ninety-nine valid responses were received within a month: 65% on the same day the survey was sent. Eighty-two-point-eight per cent were males, mostly specialists with extensive training (83.8%), and the remaining ones were fellows (16.2%). The age profile was the following one: 26.3% of the participants were between 25 and 35 years old, 46.5% were between 36 and 45 years old, and 27.3% > 45 years old. The most predominant group were interventional cardiologists (60.6%), electrophysiologists (5.1%), and cardiac surgeons (2%); 30.3% of the participants were from other medical specialties (clinicians, experts in cardiovascular imaging, etc.) (table 1).
Table 1. Scores given based on the professional profile
| Professional profile | Educational value | Patient safety | Live cases for the general public | |||
|---|---|---|---|---|---|---|
| Interventionists* (N = 67) Non-interventionists (N = 32) | 4.12 ± 0.78 3.81 ± 1.09 | P = .11 | 3.63 ± 0.99 3.38 ± 1.10 | P = .25 | 2.76 ± 1.25 2.65 ± 1.17 | P = .66 |
| Males (N = 82) Women (N = 17) | 3.96 ± 0.92 4.29 ± 0.77 | P = .17 | 3.51 ± 1.03 3.71 ± 1.04 | P = .48 | 2.54 ± 1.22 3.12 ± 1.16 | P = .14 |
| ≤ 45 years old (N = 72) > 45 years old (N = 27) | 4.15 ± 0.81 3.67 ± 1.03 | P = .01 | 3.68 ± 0.97 3.19 ± 1.11 | P = .03 | 2.75 ± 1.19 2.65 ± 1.32 | P = .73 |
| Residents or fellows (N = 16) Attending physicians (N = 83) | 4.19 ± 0.65 3.99 ± 0.94 | P = .42 | 3.75 ± 1.00 3.51 ± 1.04 | P = .39 | 2.81 ± 1.27 2.71 ± 1.22 | P = .75 |
| Participated as an operator (N = 45) Was never an operator (N = 54) | 4.02 ± 0.96 4.02 ± 0.85 | P = .98 | 3.51 ± 0.99 3.57 ± 1.07 | P = .76 | 2.69 ± 1.20 2.75 ± 1.25 | P = .79 |
|
* Including interventional cardiologists, electrophysiologists, and surgeons. |
||||||
Respondents from different countries participated: Canada, 1; Cuba, 1; Check Republic, 1; Ecuador, 1; Germany, 1; Italy, 14; Korea, 1; Mexico, 1; The Netherlands, 2; Spain, 69, Uruguay, 1; United States, 2; and not specified, 4.
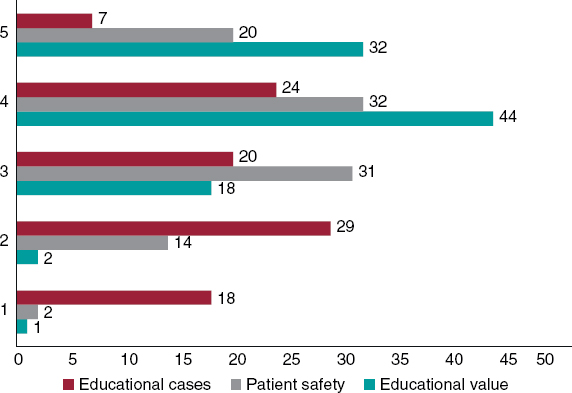
Most respondents (90.9%) said they had attended, at least, 1 course with live cases; 45.5% did so as operators too. Thirty-nine-point-four per cent had attended between 2 and 3 of these courses within the last year, and 22.2% had attended more than 3. The average score on the educational value of the live cases seen in medical courses was 4.02 ± 0.90. The average safety score was 3.55 ± 1. The average score of live educational cases was 2.72 ± 1.22 (figure 1). Among the factors considered most relevant by the respondents to give this or that score were potential distractions (54.2%), different management than usual (46.9%), overall educational value (38.5%), and impact on funding (24%).
Figure 1. Scores given by the respondents of the survey to the educational value of live cases broadcast in medical meetings (green), their safety (gray), and level of acceptance of those with educational purposes for the general public (red), between 1 and 5, from lowest to highest level of agreement.
Regarding the specific guidelines or recommendations to organize or host courses with live cases, only 19.2% had read documents on this regard.
The suggestions to improve safety were to minimize distractions by training operators and moderators and include highly experienced health professionals to avoid questions and discussions with the operators during the case that would only be allowed before or after performing the procedure.
Also, it is important to adapt oneself to the clinical practice guidelines without changing the approach by just being in a live case, avoid very complex cases, and use checklists. As a matter of fact, this may be a very appropriate scenario for the current simulation techniques that have already become very popular technological advances like computers, phantom models, etc.
Health professionals are much more critical on the procedures that are broadcast live with general educational purposes; some even do not recommend them openly and question their educational value compared to pre-filmed or pre-recorded cases. However, we should mention here that nobody identified any possible medical-legal risks for the health professionals. The potential detriment to the patient’s confidentiality or intimacy was not mentioned either.
The low response rate (27.5%) and heterogeneous sample used were some of the study limitations. Also, no parameters were built to report on how representative the results were, which may have induced a certain selection bias since only highly interested health professionals were surveyed. However, this was just an exploratory study for the sake of scientific reflection.
In conclusion, the participants of the LIVE study agreed on the benefits of this type of courses with live cases for medical training purposes for their educational value while keeping the patient safe. However, the broadcast of these courses to the general population did not achieve the same level of acceptance, which is why other curricular approaches were suggested.
FUNDING
No funding was received for this work.
CONFLICTS OF INTEREST
None.
REFERENCES
1. Millat B, Fingerhut A, Cuschieri A. Live surgery and video presentations:seeing is believing but no more:a plea for structured rigor and ethical considerations. Surg Endosc. 2006;20:845-847.
2. Fajadet J, Shelley W, Wijns W. Live-case demonstrations:putting patients aside. Eur Heart J. 2017;38:3173-3176.
3. Eliyahu S, Roguin A, Kerner A, et al. Patient safety and outcomes from live case demonstrations of interventional cardiology procedures. JACC Cardiovasc Interv. 2012;5:215-224.
4. Waksman R, Thomas M, Gloekler S, et al. The impact of live case transmission on patient outcomes during transcatheter aortic valve replacement:results from the VERITAS study. Cardiovasc Revasc Med. 2014;15:63-68.