ABSTRACT
Percutaneous coronary intervention of complex coronary artery disease remains challenging and is still associated with suboptimal cardiovascular outcomes. Over the years, different strategies and technologies have been developed to improve these results. Particularly, the development and evolution of intravascular imaging modalities to guide the procedure have improved lesion assessment and preparation, and stent optimization. However, whether these advantages are beneficial in this particular setting is still under discussion. In this article we intend to briefly summarize previous imaging-guided trials and give an outline on the ongoing large trials that are being conducted on imaging-guided interventions in complex coronary disease.
Keywords: Complex percutaneous coronary intervention. Optical coherence tomography. Intravascular ultrasound.
RESUMEN
El intervencionismo coronario complejo es aún un escenario desafiante que todavía se asocia con resultados subóptimos. A lo largo de los años han surgido diferentes estrategias y tecnologías con el objetivo de mejorar dichos resultados. En concreto, el desarrollo y la evolución de herramientas de imagen intravascular para guiar el procedimiento han permitido perfeccionar la evaluación de la lesión y su preparación, y asegurar su optimización. No obstante, los posibles beneficios de su uso en este escenario particular son aún objeto de estudio. En este artículo, el objetivo es resumir brevemente los principales estudios realizados previamente con estas técnicas, así como los ensayos que en la actualidad están en marcha en intervencionismo coronario complejo guiado por imagen.
Palabras clave: Intervencionismo coronario complejo. Tomografía de coherencia óptica. Ecografía intravascular.
Abbreviations IVUS: intravascular ultrasound. OCT: optical coherence tomography. PCI: percutaneous coronary intervention.
INTRODUCTION
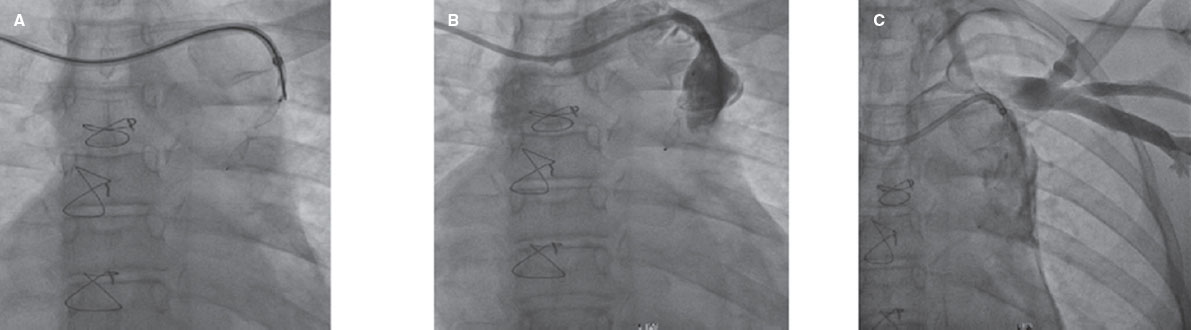
Percutaneous coronary interventions (PCI) of complex coronary artery disease namely heavily calcified coronary lesions, bifurcations (including left main coronary artery bifurcations), in-stent restenosis, chronic and acute total coronary occlusions, and long lesions is still associated with suboptimal long-term cardiovascular outcomes. Whether the advances made in stent technology and intracoronary imaging modalities can help reduce this risk is still under discussion. We provide a brief historical overview of intracoronary imaging-guided trials, and large ongoing randomize clinical trials.
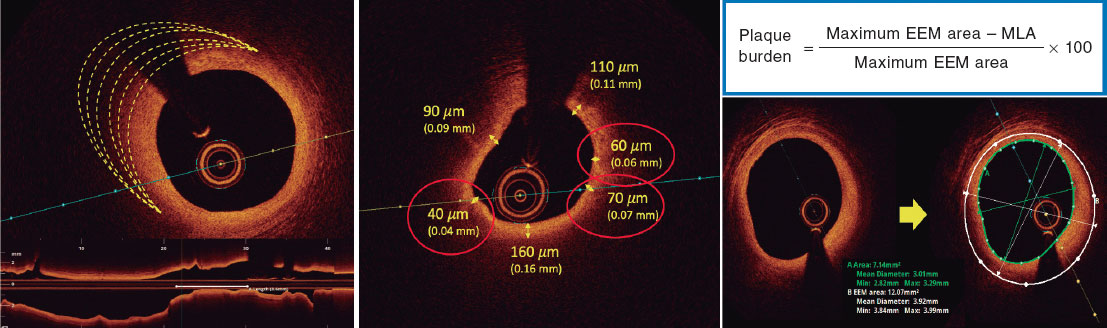
After 4 decades of angiography being the mainstay of balloon angioplasty and stent implantation procedures, the evolution of intravascular ultrasound (IVUS), and optical coherence tomography (OCT) on the wake of the availability of new-generation drug-eluting stents and bioresorbable scaffolds has prompted the gradual adoption of both intravascular imaging modalities for PCI guiding purposes. Over the years, several clinical trials and systematic reviews have compared the results and long-term outcomes of angiography vs intracoronary imaging-guided PCI with significant findings.1-12 The latest clinical practice guidelines recommend both imaging modalities to guide stent implantation in a selected subset of patients only (IVUS guidance–Class IIa, and OCT guidance–Class IIb).13,14 This opens new opportunities to set up more contemporary clinical trials in high-risk populations who may benefit the most from these interventions.
Although reports including multicenter trials and systematic reviews have shown the benefits of intravascular imaging-guided PCI compared to angiography-guided PCI, different variations have been observed in the findings reported possibly due to differences in: a) patients and lesion types included in the studies; b) the definition of a specific optimization criteria based on intravascular imaging guidance and differences in those criteria across various studies; c) the length of follow up; and d) the study endpoints. Invariably, the omission or misrepresentation of certain groups of angiographically complex lesions in former studies has triggered the need for trials to focus on this direction.2,3,7,9,15-20
Table 1 shows brief details of former imaging guidance studies and the findings reported.
Table 1. Key former studies on PCI imaging guidance
| Study (N.), NCT | Year | Guidance criteria | Modality | Endpoints | Key findings |
|---|---|---|---|---|---|
| MUSIC (N = 161) NCT N/A |
1998 | Complete stent apposition over its entire length against the vessel wall; MLA: in-stent MLA ≥ 90% of the average reference lumen area or ≥ 100% of the reference segment with the lowest lumen area; in-stent MLA of proximal stent entrance ≥ 90% of the proximal reference lumen area. If in-stent MLA is > 9.0 mm2, in-stent MLA ≥ 80% of the average reference lumen area or ≥ 90% of the reference segment with the lowest lumen area; in-stent MLA of proximal stent entrance ≥ 90% of the proximal reference lumen area; symmetric stent expansion defined by the minimum lumen diameter divided by the maximum lumen diameter ≥ 0.7 |
IVUS | Death, MI, coronary artery bypass surgery, and TLR, and clinically and/or angiographically documented (sub)acute thrombotic stent occlusion 30 days after stent implantation | 6-month angiographic outome in IVUS-guided implantation arm, a TLR of 5.7%, and a restenosis rate of 9.7% with the largest MLD 2.12 ± 0.67 |
| AVID (N = 800) NCT N/A |
2000 | MSA should be ≥ 90% of the distal reference vessel lumen cross-sectional area; stent fully apposed; dissections covered by stent | IVUS | The study primary endpoint was the rate of TLR at 12 months determined by the clinical follow-up without having to repeat the angiography | The 12-month follow-up results revealed a TLR rate of 10.1% in the angiography group vs a 4.3% rate in the IVUS group (P = .01; 95%CI, −10.6% to −1.2%) |
| SIPS (N = 269) NCT N/A |
2000 | Complete apposition against the vessel wall of the entire stent; MLA ≥ 90% of the average reference lumen area or ≥ 100% of the lumen area of the reference segment with a MLA > 9.0 mm2; MLA ≥ 80% of the average reference lumen area or ≥ 90% of the reference segment lumen area with the lowest lumen area. Symmetric stent expansion | IVUS | The study primary endpoint was the 6-month angiographic MLD. Secondary endpoints included acute MLD, acute and chronic cost, quality of life, composite clinical event rates, and clinically driven TLR | The clinical follow-up (602 days ± 307 days) showed a significant decrease in clinically driven TLR in the IVUS group compared to the standard guidance group (17% vs 29%, respectively; P = .02) |
| MAIN-COMPARE (N = 975) NCT N/A |
2009 | Specific criteria for IVUS guidance not provided | IVUS | The study primary endpoint was mortality. Secondary endpoints were MI, target vessel revascularization (TVR) or a composite of events | IVUS guidance, especially during drug-eluting stent implantation, may reduce the long-term mortality rate for unprotected left main coronary artery stenosis compared to conventional angiography guidance |
| HOME DES (N = 210) NCT N/A |
2010 | Good apposition; apposition of all stent struts to the vessel wall; Optimal stent expansion (with a MSA = 5 mm2) or a cross-sectional area > 90% of the distal reference lumen cross-sectional area for small vessels/and no edge dissection (5 mm margins proximal and distal to the stent) | IVUS | MACE (death, MI, and reintervention) | No significant differences were reported between the groups at the 18-month follow-up regarding MACE (11% vs 12%; P = NS) |
| CLI-OPCI (N = 670) NCT N/A |
2012 | Stent underexpansion was defined based on established IVUS criteria of optimal stent expansion (eg, in-stent minimal lumen area ≥ 90% of the average reference lumen area or ≥ 100% of the reference segment lumen area with the lowest lumen area) | OCT | Primary endpoint was the 1-year rate of cardiovascular death or MI | The OCT group had a significantly lower 1-year risk of cardiovascular death (1.2% vs 4.5%; P = .010), cardiac death or MI (6.6% vs13.0%; P = .006), and a composite endpoint of cardiac death, MI or new revascularization (9.6% vs 14.8%, P = .044) |
| AVIO (N = 284) NCT N/A |
2013 | Final MSA of, at least, 70% of the hypothetical cross-sectional area of the fully inflated balloon used for post-dilatation. The optimal balloon size for post-dilatation is the average of the media-to-media diameters of the distal and proximal stent segments as well as at the sites of maximum in-stent narrowing. The value is rounded to the lowest 0.00 mm or 0.50 mm. For values ≥ 3.5 mm the operator could downsize the diameter of the balloon based on his best clinical judgment |
IVUS | The primary study endpoint was the postoperative lesion minimal lumen diameter. The secondary endpoints were a composite of MACE, TLR, target vessel revascularization, MI, and stent thrombosis at 1, 6, 9, 12, and 24 months | IVUS optimized DES implantation as seen on the complex lesions in the postoperative minimal lumen diameter. No statistically significant differences were found in MACE at the 24-month follow-up. |
| RESET (N = 1574) NCT N/A |
2013 | Specific criteria for IVUS guidance not provided | IVUS | MACE, including cardiovascular death, MI or target vessel revascularization at the 1-year follow-up after DES implantation in short-length lesions | There were no statistically significant differences regarding the MACE outcome between the IVUS-guided and the angiography-guided groups |
| AIR CTO (N = 230) NCT N/A |
2015 | Good apposition, MSA > 80% of the reference vessel area, symmetry index > 70%, and no > type B dissection | IVUS | The primary endpoint was in-stent late lumen loss at the 1-year follow-up | The in-stent late lumen loss in the IVUS-guided group was significantly lower compared to the angiography-guided group at the 1-year follow-up (0.28 mm ± 0.48 mm vs 0.46 mm ± 0.68 mm; P = .025) with a significant difference of the “in-true-lumen” stent restenosis between the 2 groups (3.9% vs13.7%; P = .021) |
| CTO IVUS (N = 402) NCT01563952 |
2015 | a) MSA ≥ distal reference lumen area; b) stent area at CTO segment ≥ 5 mm2 vessel area permitting; and c) complete stent apposition | IVUS | The primary endpoint was the occurrence of cardiovascular death. The secondary endpoint was MACE defined as a composite of cardiovascular death, MI or target vessel revascularization at 12 months | The IVUS-guided CTO intervention did not reduce cardiovascular mortality significantly. The occurrence of MACE was significantly lower in the IVUS-guided group compared to the angiography-guided group (2.6% vs 7.1%) |
| IVUS-XPL (N = 1400) NCT01308281 |
2016 | MLA greater than the lumen cross-sectional area at the distal reference segments post-PCI | IVUS | The primary outcome measure was a composite of MACE, including cardiovascular death, target vessel MI or ischemia-driven TLR at the 1-year follow-up analyzed by intention-to-treat | IVUS-guided stent implantation was associated with a significant 2.9% absolute reduction, and a 48% relative reduction in the risk of MACE at the 1-year follow-up compared to angiography-guided stent implantation |
| ILUMIEN III (N = 450) NCT02471586 |
2016 | MSA: achievement of, at least, acceptable stent expansion (a minimum stent area of, at least, 90% in both the proximal and distal halves of the stent relative to the closest reference segment) Acceptable stent expansion: the MSA of the proximal segment is ≥ 90% and < 95% of the proximal reference lumen area, and the MSA of the distal segment is ≥ 90% and < 95% of the distal reference lumen area |
IVUS, OCT | The primary efficacy endpoint was the post-PCI minimum stent area as seen on the OCT at a masked independent core laboratory after completing recruitment in all randomly allocated participants with primary outcome data available. The primary safety endpoint was procedural MACE | OCT guidance was non-inferior to IVUS guidance (one-sided 97.5% lower confidence interval, −0.70 mm²; P = ·001), but not superior either to IVUS-guidance (P = .42) and angiography guidance (P = .12). There were no significant differences in the MACE outcome |
| OPINION (N = 800) NCT01873222 |
2016 | In-stent MLA ≥ 90% of the average reference lumen area; complete stent apposition over its entire length against the vessel wall; symmetric stent expansion defined by minimum lumen diameter/maximum lumen diameter ≥ 0.7; no plaque protrusion, thrombus or edge dissection with potential to provoke flow disturbances | IVUS, OCT | The primary endpoint was TVF defined as a composite of cardiovascular death, target vessel MI, and ischemia-driven target vessel revascularization 12 months after the PCI | TVF occurred in 21 (5.2%) out of the 401 patients undergoing OFDI-guided PCI, and in 19 (4.9%) out of the 390 patients undergoing IVUS-guided PCI, which proved the non-inferiority of OFDI-guided PCI with respect to the IVUS-guided PCI (hazard ratio, 1.07; upper limit of one-sided 95%CI, 1.80; P value for non-inferiority = .042) |
| ULTIMATE (N = 1448) NCT02215915 |
2021 | a) In-stent MLA > 5.0 mm or 90% of the MLA at the distal reference segments; b) plaque burden 5 mm proximal or distal to the stent edge is < 50%; and c) no edge dissection involves the media with a length > 3 mm | IVUS | The primary endpoint was the risk of TVF at the 3-year follow-up | IVUS-guided DES implantation was associated with significantly lower rates of TVF and stent thrombosis at the 3-year follow-up among all-comers |
|
95%CI, 95% confidence interval; CTO, chronic total coronary occlusion; DES, drug-eluting stent; IVUS, intravascular ultrasound; MACE, major adverse cardiovascular events; MLA, minimum lumen area; MI, myocardial infarction; MLD, minimum lumen diameter; MSA, minimum stent area; NA, not available; NS, not significant; OFDI, optical frequency domain imaging; OCT, optical coherence tomography; PCI, percutaneous coronary intervention; TLR, target lesion revascularization; TVF, target vessel failure. |
|||||
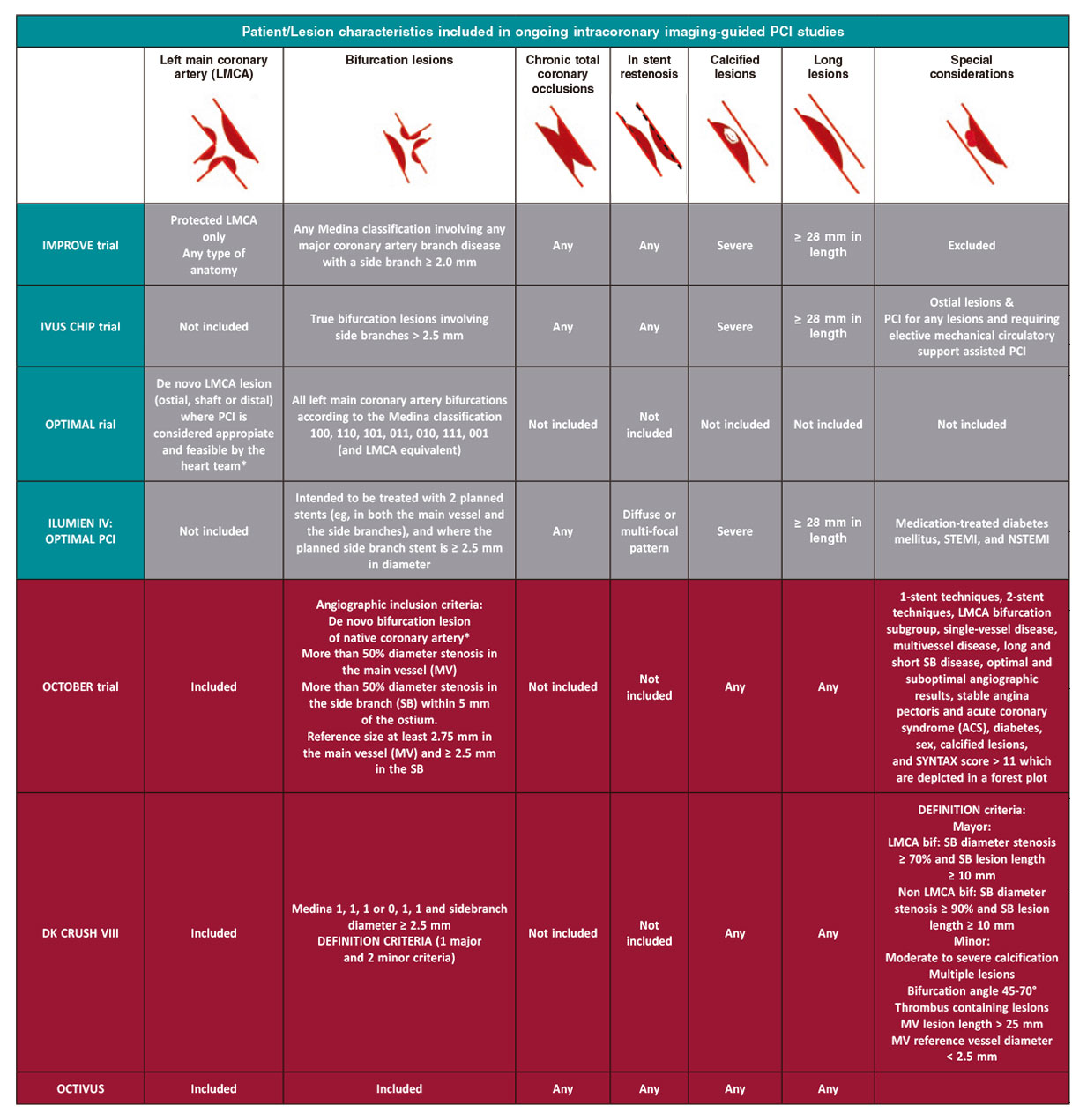
Subsequently, new ongoing studies are assessing the effect of PCI imaging guidance on the clinical outcomes over longer follow-up periods and the value of guiding interventions with imaging modalities when treating specific lesion subsets like in-stent restenosis, calcified lesions, and long lesions. Table 2 highlights the ongoing PCI guidance trials.
Table 2. Ongoing studies on PCI imaging guidance
| Study, NCT | Modality | Study design | Study objective | Imaging criteria | Clinical endpoints |
|---|---|---|---|---|---|
| IMPROVE, NCT04221815 | IVUS vs angiography | Prospective multileft, international, single-blind clinical investigation No. of subjects: approximately 2500-3100 randomized subjects Follow-up period: 2 years |
To demonstrate the superiority of an IVUS-guided stent implantation strategy compared to an angiography-guided stent implantation strategy achieving larger post-PCI lumen dimensions, and improving the clinical cardiovascular outcomes of patients with complex angiographic lesions | Optimal stent deployment is considered to have been achieved if the following 3 criteria are met on the final IVUS: MSA > 90% of the distal reference lumen area. No edge dissection involving the media with an arc ≥ 60° and length ≥ 3 mm Absence of geographic miss defined as plaque burden > 50% within 5 mm from the proximal or distal stent edge or both |
Target vessel failure outcomes at 12 months defined as a composite of cardiovascular death, target vessel MI or clinically indicated target vessel revascularization |
| IVUS-CHIP, NCT04854070 | IVUS vs angiography | Randomized, controlled, multileft, international, event-driven, post-marketing study. A total of 2020 patients will be randomized in a 1:1 fashion to the IVUS-guided PCI vs the angio-guided PCI | To demonstrate the superiority of IVUS guidance compared to angio guidance regarding target vessel failure | Final MSA > 5 mm2 or MSA < 90% of distal reference lumen Plaque burden < 50% within 5 mm from the proximal or distal stent edge No edge dissection involving the media and > 3 mm in length |
Target vessel failure defined as a composite of cardiovascular death, target vessel MI or clinically indicated target vessel revascularization |
| OPTIMAL, NCT04111770 | IVUS vs angiography | Randomized, controlled, multileft, international study | To demonstrate the superiority of IVUS- vs angiography-guided stent implantation in patients with LMCA disease, and also improving the clinical outcomes | MSA > 5 (LCX), > 6 (LAD), > 7 (bifurcation point), > 8 (LMCA) Malapposition < 0.4 mm Absence of edge dissection defined as ≥ 60° and ≥ 2 mm in length Plaque burden at the edge of the stent < 50% |
Patient-oriented composite endpoint (POCE): a composite of all-cause death, any strokes, any MIs, any clinically indicated revascularizations at the 2-year follow-up |
| ILUMIEN IV, NCT03507777 |
OCT vs angiography | Prospective, multileft, randomized, controlled clinical trial No. of subjects: between 2490 and 3656 Follow-up period: 2 years Expected study duration: approximately 2 years |
To demonstrate the superiority of OCT- vs angiography-guided stent implantation in the patients’ clinical outcomes | To achieve: Acceptable stent expansion (an MSA of, at least, 90% in both the proximal and distal segments of the stent relative to the closest reference segment). Both proximal/distal reference segments have a minimal lumen area ≥ 4.5 mm2 Absence of a major edge dissection defined as ≥ 60° of the vessel circumference at the dissection site and ≥ 3 mm in length |
Target vessel failure, a composite of cardiovascular death, target vessel MI or ischemia-driven target vessel revascularization |
| DKCRUSH VIII, NCT03770650 |
IVUS vs angiography | Randomized, controlled, multicenter trial Sample size: 556 patients Allocation 1:1 |
To assess superiority of IVUS-guided vs angiography-guided DK Crush stenting in complex bifurcations | For LMCA: MSA ≥ 10mm2 (LM), 7mm2(LAD), 6mm2 (CX) Stent expansion index ≥ 90% (of distal reference lumen area in LCX) Symmetry index > 0.8 For non-LMCA: MSA ≥ 6mm2 in the main vessel, and ≥ 5mm2 in the ostial side branch Stent expansion ≥ 90% of distal reference lumen area Symmetry index > 0.8 |
The primary outcome is the rate of 12-month target vessel failure: Cardiac death, target vessel myocardial infarction, clinically driven target vessel revascularization |
| OCTOBER, NCT03171311 |
OCT vs angiography | Randomized, investigator-initiated, multileft trial. The calculated sample size is 1200 patients in total allocated in a 1:1 fashion |
To show the superiority of OCT-guided stent implantation compared to standard angiographic-guided implantation in bifurcation lesions | Adequate vessel and stent expansion (> 90%) Full stent apposition Optimal lesion coverage |
The primary outcome measure is a 2-year composite endpoint of cardiovascular death, target lesion myocardial infarction, and ischemia-driven target lesion revascularization |
| OCTIVUS, NCT03394079 |
OCT vs IVUS guided PCI | Multicenter, randomized, controlled trial. “All-comer” population ample size:2000 patients Allocation 1:1 |
To compare the clinical efficacy and safety of OCT-guided and IVUS-guided PCI | Optimization criteria by IVUS or OCT: Stent expansion > 80% by average reference lumen area Absence of large dissections (> 60º, > 2mm length, flap extending to media or adventicia). Absence of malapposition Avoidance of a landing zone in a plaque burden < 50% or lipid-rich tissue at stent edge Distal lumen reference based (0.25mm up-round) or EEM reference based (0.25mm down-round) |
The primary outcome is target vessel failure: cardiac death, target vessel myocardial infarction or ischemia-driven target vessel revascularization at 1 year. |
|
IVUS, intravascular ultrasound; LAD, left anterior descendent coronary artery; LCX, left circumflex artery, LMCA, left main coronary artery; MI, myocardial infarction; MSA, minimum stent area; OCT, optical coherence tomography; PCI, percutaneous coronary intervention. |
|||||
ONGOING CLINICAL TRIALS ON INTRAVASCULAR ULTRASOUND GUIDANCE
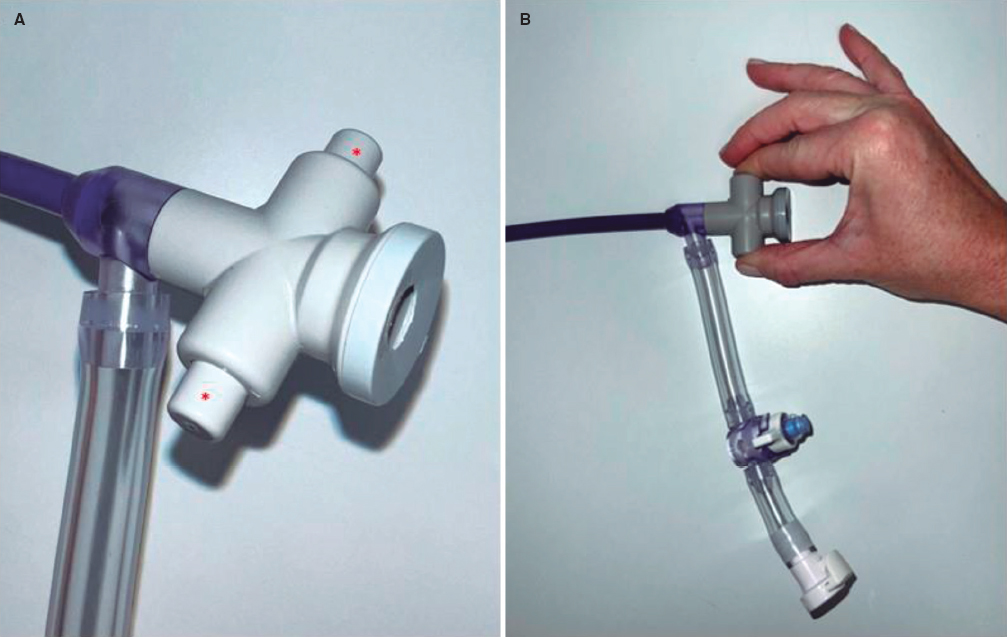
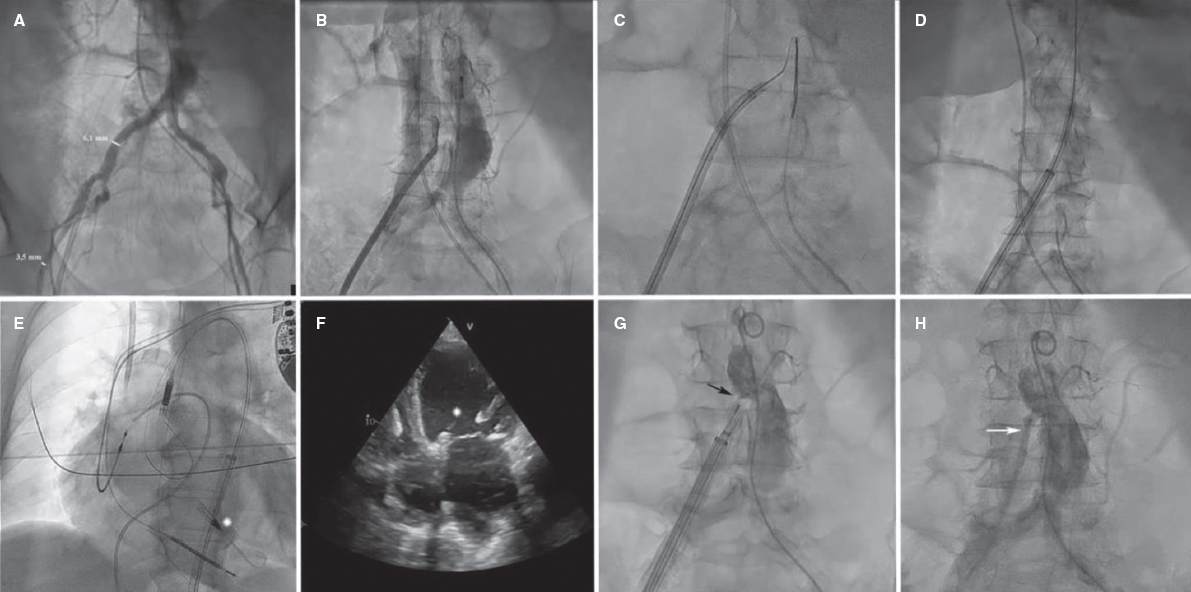
The IMPROVE (Impact on revascularization outcomes of IVUS-guided treatment of complex lesions and economic impact, NCT04221815) trial,17 a multicenter, prospective, single-blind 3100 patient study, aims to demonstrate the superiority of IVUS-guided stent implantation over the angiography-guided stent implantation strategy in complex lesions (including chronic total coronary occlusions, calcified lesions, long lesions, bifurcations, and in-stent restenosis) based on the different post-PCI minimum stent area, and target vessel failure outcomes reported at 12 months defined as a composite endpoint of cardiovascular death, target vessel myocardial infarction, and ischemia-driven target vessel revascularization (table 2 and figure 1).
Figure 1. Main patient and lesion characteristics included in these ongoing large intracoronary imaging trials. * Functional inclusion criteria: functional significance of the main vessel lesion or documented ischemia of the main vessel territory or other objective documentation of lesion significance. Objective evidence of ischemia is required for all target lesions except for those with > 80% diameter stenosis that may be considered significant. PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction; NSTEMI, non—ST-segment elevation myocardial infarction; SB, side branch.
The IVUS-CHIP trial (Intravascular ultrasound guidance for complex high-risk indicated procedures, NCT04854070) is a randomized, controlled, multicenter, international, event-driven, post-marketing study. A total of 2020 participants with complex coronary lesions (angiographic heavy calcifications, ostial lesions, true bifurcation lesions, left main coronary artery lesions, chronic total coronary occlusions, in-stent restenosis, long-lesions) or requiring elective mechanical circulatory support assisted PCI will be randomized in a 1:1 fashion to receive IVUS-guided PCI vs angio-guided PCI. The study aims to demonstrate the superiority of the IVUS guidance strategy in terms of the primary endpoint, target vessel failure, defined as a composite endpoint of cardiovascular death, target vessel myocardial infarction or clinically indicated target vessel revascularization (table 2 and figure 1).
The OPTIMAL (Optimization of left main PCI with intravascular ultrasound, NCT04111770) study is a randomized, controlled, multicenter, international study. A total of 800 patients will be randomized in a 1:1 fashion to receive IVUS-guided PCI vs qualitative angiography-guided PCI. Patients with a de novo left main coronary artery lesion (ostial, shaft or distal) eligible for a PCI according to the heart team will be included. All left main coronary artery bifurcations according to the Medina classification 100, 110, 101, 011, 010, 111, 001 (and LMCA equivalent) can be included. Patients with a previous coronary artery bypass graft and no patent bypass on the left main coronary artery can be included too. The study primary endpoint is a patient-oriented composite endpoint: a composite of all-cause mortality, any strokes, any myocardial infarctions, and any clinically indicated revascularizations at the 2-year follow-up (table 2 and figure 1).
The DK CRUSH VIII trial (NCT03770650)19 is a randomized, controlled, multicenter study that aims to assess the superiority of IVUS-guided versus angiography-guided DK crush stenting in 556 patients with complex bifurcation lesions based on DEFINITION criteria. Its primary endpoint is the rate of cardiac death, target vessel failure, target vessel myocardial infarction or target vessel revascularization at 12 months (table 2 and figure 1).
ONGOING CLINICAL TRIALS ON OPTICAL COHERENCE TOMOGRAPHY
In the past, the ILUMIEN III study (NCT02471586), that reported on the non-inferiority of OCT compared to IVUS (minimal stent area; one-sided 97.5% lower confidence interval, –0.70 mm²; P = .001) proved the superiority of the OCT-guided stent implantation strategy compared to the angiography-guided stent implantation strategy achieving larger post-PCI lumen dimensions, and improving clinical cardiovascular outcomes in patients with high-risk clinical characteristics and/or high-risk angiographic lesions. The ILUMIEN IV (NCT03507777) trial that has completed recruitment (3600 patients initially planned) intends to demonstrate the superiority of an OCT-guided stent implantation strategy over an angiography-guided stent implantation strategy achieving larger post-PCI lumen dimensions, and improving clinical cardiovascular outcomes in patients with high-risk clinical characteristics like diabetes and/or high-risk angiographic lesions. The result of both studies and their similar endpoints will be shedding light on the role played by intravascular imaging guidance especially for the management of complex coronary lesions (table 2 and figure 1).
Another OCT clinical trial is the European trial on optical coherence tomography optimized bifurcation event reduction (OCTOBER, NCT03171311), a randomized, investigator-initiated, multicenter trial aimed at showing the superiority of OCT-guided stent implantation compared to standard angiographic-guided implantation in bifurcation lesions. Stratified randomization: a) left main or non-left main coronary artery disease, and b) upfront planned 1-stent technique with kissing balloon inflation or a 2-stent technique.18
A direct comparison of OCT and IVUS is planned in the OCTIVUS trial (NCT03394079), a multicenter, controlled trial of an all comers population that will be randomized to either OCT-guided PCI or IVUS-guided PCI.20 The primary endpoint is death, target vessel myocardial infarction and ischemia-driven target vessel revascularization at one year (table 2 and figure 1).
CONCLUSIONS
Undoubtedly, intravascular imaging plays a role optimizing stent implantation, the extent of which remains to be fully grasped particularly in complex populations and lesion subsets. Based on previous reports that showed overwhelming evidence in favor of intravascular imaging-guided PCI, it is expected that these large 4 contemporary randomized clinical trials will show a reduction of major adverse cardiovascular events and, therefore, favor the use of intracoronary imaging in these populations and lesion subsets. One may also predict a significant increase in the use of IVUS/OCT based on the positive results, increased reimbursements, and hopefully a change in the societal guideline recommendations.
FUNDING
None whatsoever.
AUTHORS’ CONTRIBUTIONS
H.M. Garcia-Garcia is responsible for the study design and draft of the manuscript. E. Fernández-Peregrina, K.O. Kuku, and R. Diletti also drafted the manuscript and gave their critical review.
CONFLICTS OF INTEREST
H.M. Garcia-Garcia, and K.O. Kuku declared having received Institutional grant support from Biotronik, Boston Scientific, Medtronic, Abbott Vascular, Neovasc, Shockwave, Phillips, and Corflow. R. Diletti also declared having received institutional grant support from Biotronik, and Boston Scientific. E. Fernández-Peregrina declared having received a research grant from Sociedad Española de Cardiología.
REFERENCES
1. de Jaegere P, Mudra H, Figulla H, et al. Intravascular ultrasound-guided optimized stent deployment. Immediate and 6 months clinical and angiographic results from the Multicenter Ultrasound Stenting in Coronaries Study (MUSIC Study). Eur Heart J. 1998;19:1214-1223.
2. Chieffo A, Latib A, Caussin C, et al. A prospective, randomized trial of intravascular-ultrasound guided compared to angiography guided stent implantation in complex coronary lesions:the AVIO trial. Am Heart J. 2013;165):65-72.
3. Tian N-L, Gami S-K, Ye F, et al. Angiographic and clinical comparisons of intravascular ultrasound- versus angiography-guided drug-eluting stent implantation for patients with chronic total occlusion lesions:two-year results from a randomised AIR-CTO study. EuroIntervention. 2015;10:1409-1417.
4. Kim B-K, Shin D-H, Hong M-K, et al. Clinical Impact of Intravascular Ultrasound-Guided Chronic Total Occlusion Intervention With Zotarolimus-Eluting Versus Biolimus-Eluting Stent Implantation:Randomized Study. Circ Cardiovasc Interv. 2015;8:e002592.
5. Hong S-J, Kim B-K, Shin D-H, et al. Effect of Intravascular Ultrasound-Guided vs Angiography-Guided Everolimus-Eluting Stent Implantation:The IVUS-XPL Randomized Clinical Trial. JAMA. 2015;314:2155-2163.
6. Park S-J, Kim Y-H, Park D-W, et al. Impact of Intravascular Ultrasound Guidance on Long-Term Mortality in Stenting for Unprotected Left Main Coronary Artery Stenosis. Circ Cardiovasc Interv. 2009;2:167-177.
7. Jakabcin J, Spacek R, Bystron M, et al. Long-term health outcome and mortality evaluation after invasive coronary treatment using drug eluting stents with or without the IVUS guidance. Randomized control trial. HOME DES IVUS. Catheter Cardiovasc Interv. 2010;75:578-583.
8. Kim J-S, Kang T-S, Mintz GS, et al. Randomized comparison of clinical outcomes between intravascular ultrasound and angiography-guided drug-eluting stent implantation for long coronary artery stenoses. JACC Cardiovasc Interv. 2013;6:369-376.
9. Sheth TN, Kajander OA, Lavi S, et al. Optical Coherence Tomography-Guided Percutaneous Coronary Intervention in ST-Segment-Elevation Myocardial Infarction:A Prospective Propensity-Matched Cohort of the Thrombectomy Versus Percutaneous Coronary Intervention Alone Trial. Circ Cardiovasc Interv. 2016;9:e003414.
10. Kim I-C, Yoon H-J, Shin E-S, et al. Usefulness of Frequency Domain Optical Coherence Tomography Compared with Intravascular Ultrasound as a Guidance for Percutaneous Coronary Intervention. J Interv Cardiol. 2016;29:216-224.
11. Steinvil A, Zhang Y-J, Lee SY, et al. Intravascular ultrasound-guided drug-eluting stent implantation:An updated meta-analysis of randomized control trials and observational studies. Int J Cardiol. 2016;216:133-139.
12. Shin D-H, Hong S-J, Mintz GS, et al. Effects of Intravascular Ultrasound-Guided Versus Angiography-Guided New-Generation Drug-Eluting Stent Implantation:Meta-Analysis With Individual Patient-Level Data From 2,345 Randomized Patients. JACC Cardiovasc Interv. 2016;9:2232-2239.
13. Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58:e44-122.
14. Kolh P, Windecker S, Alfonso F, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization:the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur J Cardiothorac Surg. 2014;46:517-592.
15. Bavishi C, Sardar P, Chatterjee S, et al. Intravascular ultrasound-guided vs angiography-guided drug-eluting stent implantation in complex coronary lesions:Meta-analysis of randomized trials. Am Heart J. 2017;185:26-34.
16. Ali Z, Landmesser U, Karimi Galougahi K, et al. Optical coherence tomography-guided coronary stent implantation compared to angiography:a multicentre randomised trial in PCI - design and rationale of ILUMIEN IV:OPTIMAL PCI. EuroIntervention. 2021;16:1092-1099.
17. Shlofmitz E, Torguson R, Mintz GS, et al. The IMPact on Revascularization Outcomes of intraVascular ultrasound-guided treatment of complex lesions and Economic impact (IMPROVE) trial:Study design and rationale. Am Heart J. 2020;228:65-71.
18. Holm NR, Andreasen LN, Walsh S, et al. Rational and design of the European randomized Optical Coherence Tomography Optimized Bifurcation Event Reduction Trial (OCTOBER). Am Heart J. 2018;205:97-109.
19. Ge Z, Kan J, Gao XF et al. Comparison of intravascular ultrasound-guided with angiography-guided double kissing crush stenting for patients with complex coronary bifurcation lesions: Rationale and design of a prospective, randomized, and multicenter DK CRUSH VIII Trial. Am Heart J. 2021;234:101-110.
20. Kang DY, Ahn JM, Park H et al. Comparison of optical coherence tomography-guided percutaneous coronary intervention: Rationale and design of a randomized, controlled OCTIVUS trial. Am Heart J. 2020;228:72-80.
* Corresponding author: Division of Interventional Cardiology, MedStar Washington Hospital Center, 100 Irving St., NW Washington DC 20010, United States.
E-mail addresses: hector.m.garciagarcia@medstar.net; hect2701@gmail.com (H.M. Garcia-Garcia).