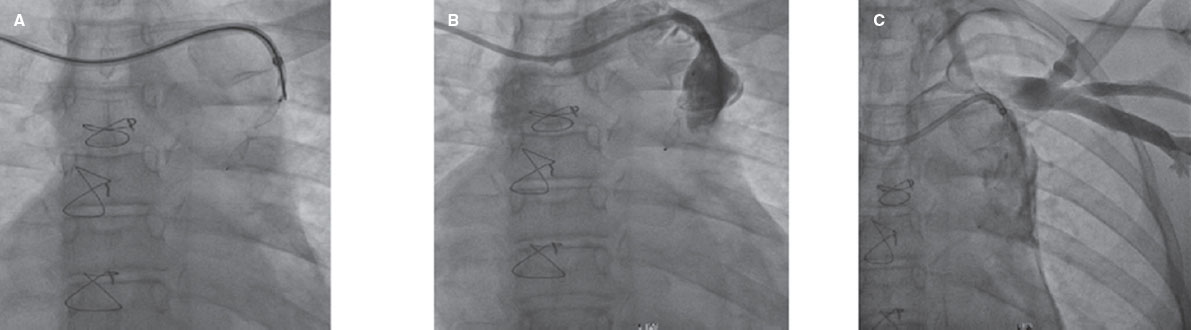
QUESTION: For starters, what is the minimalist approach to transcatether aortic valve implantation (TAVI)?
ANSWER: After the first case described by Cribier et al.1 back in 2002, the management of aortic stenosis through TAVI has consolidated and become a safe and effective therapy that is based on a well-established and standardized procedure. Although it is a complex procedure due to the characteristics of patients and devices and the fact that experienced operators are needed, the growing number of cases reported, and the technological advances made with the devices have improved processes and reduced complications significantly. This has prompted that, over the last few years, certain experienced groups2 have modified certain steps of the procedure and introduced strategies before and after the intervention to simplify and make TAVI more efficient. Also, to promote faster recoveries in the patients. This set of modifications is described as minimalist approach to TAVI. Two of the most significant aspects here are suppressing balloon dilatation and reducing hospital stays. However, there are simplifying strategies that can be divided into 3 parts: previous assessment and case analysis, valve implantation, and postoperative care. During the previous assessment part, the objective is to speed up the study circuits of the patients and reduce the waiting lists. Also, the decision between surgery or TAVI should not be made on the surgical risk but on the risk-benefit ratio based on the patient’s age, comorbidities, functional status, frailty, anatomical characteristics, family support, and on the experience and results of the treating center. Regarding valve implantation, the simplifying strategies are applied in different settings:
-
– Healthcare professionals and setting. Procedures can be performed in a cath lab by experienced interventional cardiologists. In cases of transfemoral access, the heart team often includes 2 interventional cardiologists, 2 nurses, and 1 patient care technician. The nurse or the technician is in charge of preparing the device. The presence of 1 anesthesiologist and 1 expert cardiologist in imaging modalities or 1 echocardiographist is advised. With highly selected patients—complex access sites or different from the femoral access, etc.—or if certain complications occur the collaboration of a cardiovascular surgeon may be required.
-
– Anesthesia. It is one of the main changes of this minimalist approach. Although the presence of an anesthesiologist during the procedure is advised, general anesthesia is often substituted for local anesthesia and sedation. This avoids intubation and ventilation, minimizes risks, and reduces the hospital stay. General anesthesia would be spared for patients of a higher risk of complications who cannot tolerate the procedure or with high chances of conversion to surgery.
-
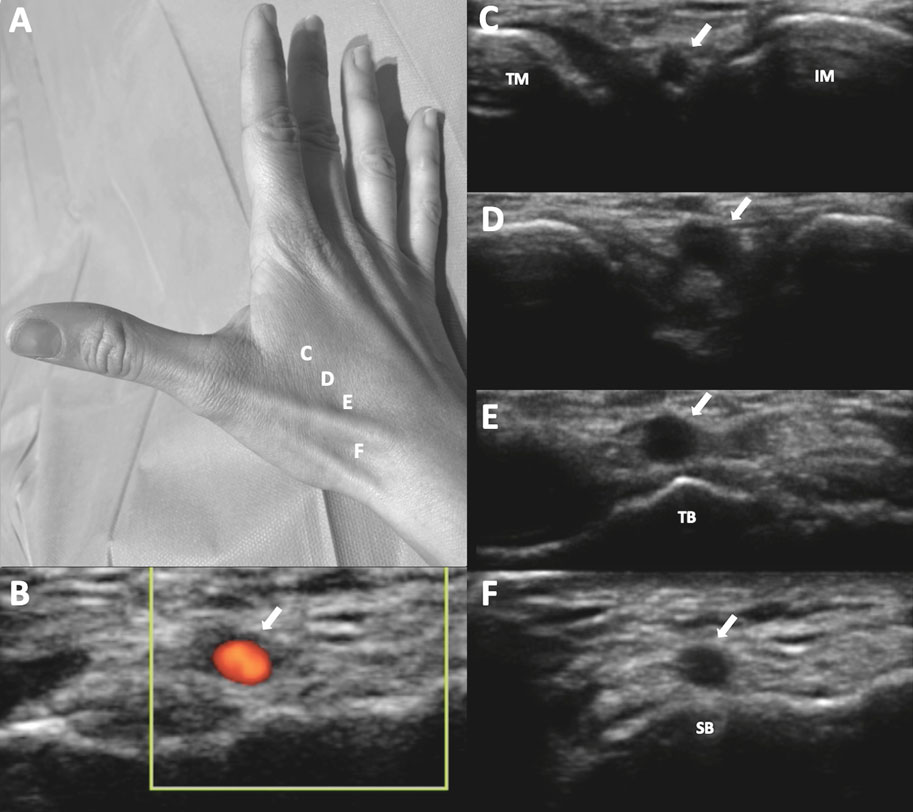
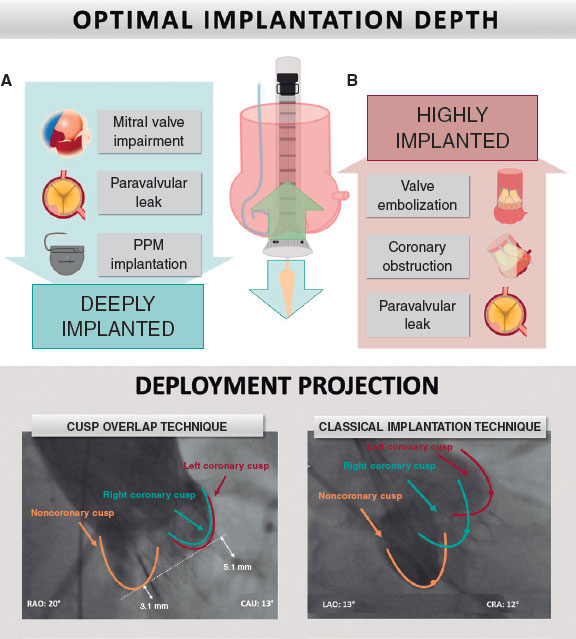
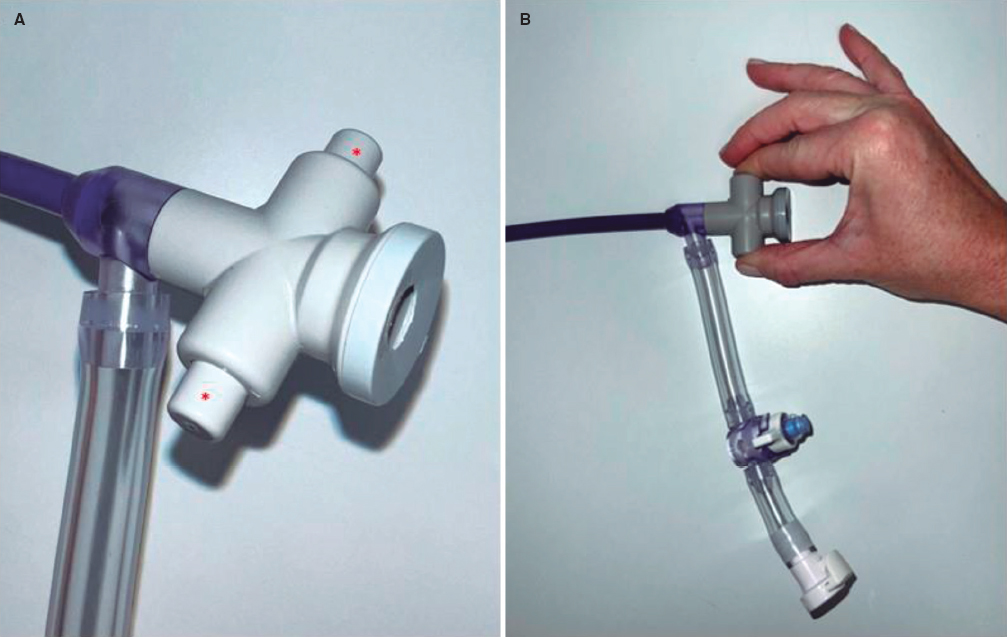
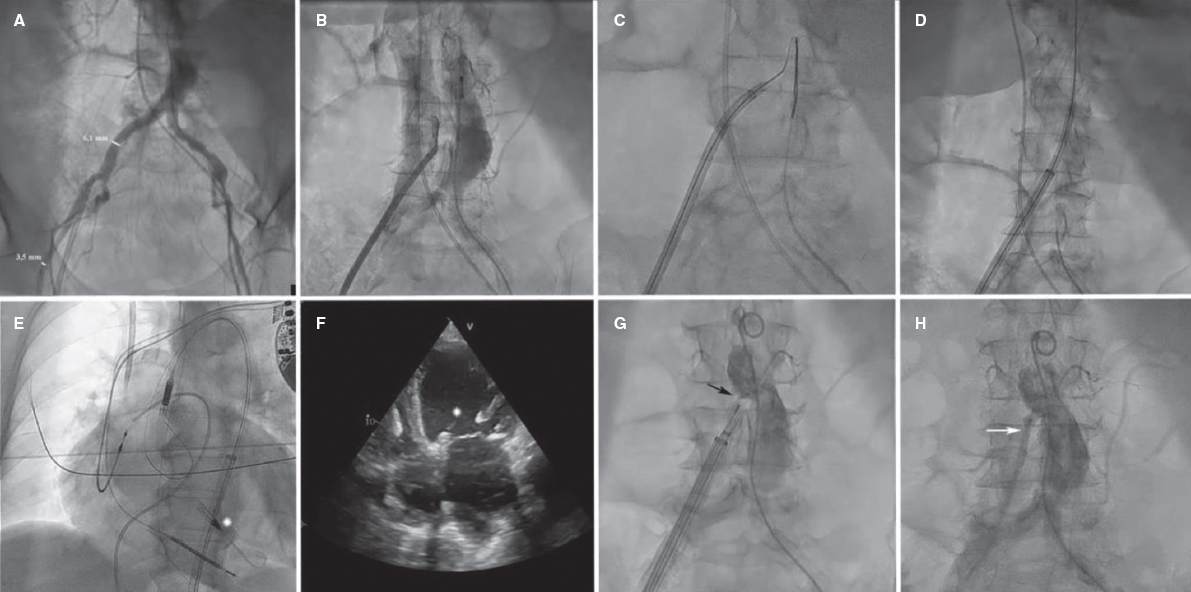
– Arterial access. In the primary access, the femoral access is often the one used for valve implantation and has given the best results of all. However, there are other alternatives available when it is not feasible. Puncture should be angiography- or ultrasound-guided and percutaneous closure is often performed with devices like Prostar (Abbott Vascular, United States), Perclose Proglide (Abbott Vascular, United States) or Manta (Teleflex, United States). Although the femoral access site is the preferred one in some cases for a direct control of hemostasis, with these devices, percutaneous puncture is a less invasive option that has good results. Regarding secondary arterial access, another arterial access site is often required, usually the contralateral femoral artery, for pigtail catheter insertion to perform the aortography. When inserted into the non-coronary sinus it serves as the reference for implantation. This access site also allows us to advance the protection guidewire inside the artery through which the access occurs in such a way that, if vascular closure is incomplete or fails, on top of providing compression, a balloon can be advanced to occlude the flow and a covered stent can be implanted. To this point, everal minimalist approaches have been suggested: a) use the radial access as the secondary access; b) simplify it by performing a more distal puncture preferably in the common femoral artery 2 cm further down or in the superficial femoral artery. Through 4-Fr or 5-Fr introducer sheath a protection guidewire would be advanced to perform selective injections, and c) with the smaller size of today’s sheath some even suggest inserting a protection guidewire.
-
– Echocardiogram. Using transthoracic echocardiography during implantation is considered enough because it avoids the problems associated with the transesophageal echocardiogram and allows us to assess fundamental aspects such as LV contractility, the position of the guidewire, and the outcome of valve implantation. Also, complications like cardiac tamponade, aortic regurgitation, etc can be discarded.
-
– Transient pacemaker. Rapid ventricular pacing is required for balloon-expandable valve and certain self-expandable valve implantation. Balloon-tipped electrode catheters should be used to reduce the risk of perforation. To avoid the problems associated with catheterizing that venous route, a metal guidewire placed in the left ventricle can be used for pacing purposes. After placing a subcutaneous 22G needle close to the sheath, the clips are connected to the needle (positive) and the ventricle metal guidewire (negative) isolated with a catheter or a valve placed close to the annulus. If there is no AV block (transient or permanent) or QRS widening > 160 m the pacemaker is removed in the cath lab after analyzing the electrocardiogram. If a definitive pacemaker is required, it should be implanted within the next 72 hours to avoid unnecessary longer the hospital stays.
-
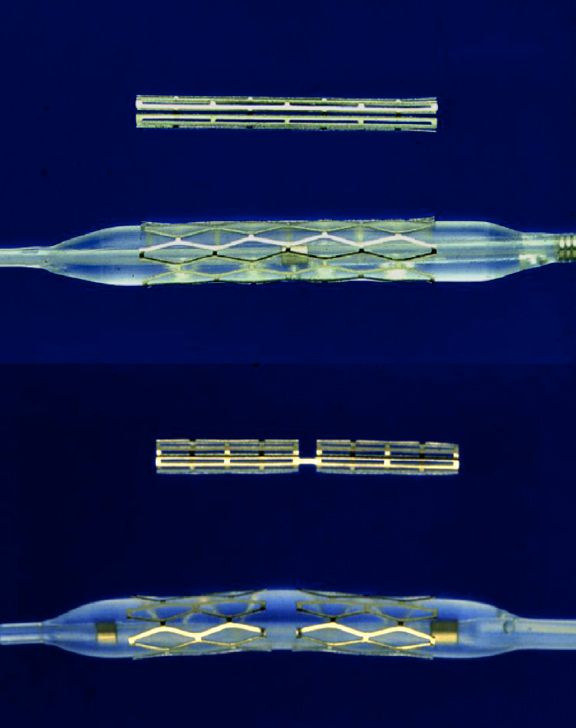
– Avoid balloon predilatation. With some of the new valves available it is possible to perform direct valve implantation, thus reducing the risks derived from aortic valvuloplasty.
-
– Avoid urinary catheterization. It reduces hospital complications—infections, hematuria—and the hospital stay.
Regarding the third part, postoperative care, it is necessary to monitor the patient closely within the first few hours by closely assessing his hemodynamic status and the vascular access routes. Follow-up blood tests should be performed to detect blood losses. Also, the heart rhythm should be monitored to rule out the presence of cardiac conduction disorders or new-onset arrhythmias. A control echocardiogram is required the next day and, in the absence of complications, the patient should regain mobilization soon.
Q.: What advantages does deep sedation have over general anesthesia and how do you think it should be performed?
A.: The presence of an anesthesiologist in the cath lab guarantees closer monitoring and brings comfort to the patient. It also speeds up the procedure in case of complications. This does not necessarily imply using general anesthesia in every case: the use of conscious sedation and local anesthesia allows us to avoid orotracheal intubation, brings greater hemodynamic stability, and shorter procedural and recovery times. Several studies have proven the safety profile of this type of sedation with similar rates of mortality and complications;3,4 its use has become very popular over the last few years. For example, in France,5 it was used in 30% of the cases in 2010 up to 70% in 2017. Therefore, general anesthesia would be spared for patients with hemodynamic instability and higher risk of complications who don’t tolerate the procedure or have high chances of conversion to surgery.
Q.: How is echocardiographic imaging implemented during TAVI? Always or occasionally? Transthoracic or transesophageal?
A.: Having a cardiologist expert in cardiac imaging modalities performing monitorization tasks through transthoracic echocardiogram brings extra safety, and avoids the problems associated with the transesophageal echocardiogram. This expert can control the position of the guidewire inside the ventricle, confirm the results of implantation by assessing gradients, identify some degrees of aortic regurgitation, and detect rapidly possible complications that may occur like abnormalities in cardiac contractility or the appearance of pericardial effusion. Transesophageal echocardiogram would be spared for cases of poor acoustic window or specific needs.
Q.: There are very different vascular occlusion systems available. Are there significant differences to pick one over the other based on certain characteristics of the patient? Which are the preferences of your heart team?
A.: Different suture-mediated closure devices (Proglide, Prostar) or collagen-based devices (Manta)6,7 can be used with good results. Some may be used based on the preferences or experience of the heart team since the comparative studies conducted so far do not make any clear differences on this regard. Suture-mediated closure devices may have more problems in femoral arteries with calcium deposits while the Manta collagen-based devices can present complications in small-caliber femoral arteries (< 6 mm) or in very obese patients. Also, we should take into consideration the cost of each one of these devices, and the necessary learning curves. The single or double Proglide device is the most widely used. As a matter of fact, the latter is the common strategy in our center. None of them is infallible and in the presence of bleeding a balloon is required for occlusion purposes and even covered stent graft implantation to contain the bleeding.
Q.: Which is the average hospital stay after TAVI at your center? What do you think of 24 to 48-hour early hospital discharges?
A.: In our center, the average hospital stay is between 3 and 4 days because, although we try to discharge the patients 48 hours after the procedure, their risk profile often requires longer hospital stays. The patient should regain mobility within a few hours if the transient pacemaker has been removed and there are no vascular access complications. Therefore, uncomplicated patients can be discharged in < 72 hours. This early hospital discharge has proven feasible and safe in different studies and even in 1 meta-analysis that confirmed the good results of discharging patients within 3 days.8 Next-day faster hospital discharges are also possible in highly selected patients without procedural complications.9 However, a reason for concern in these patients is the possibility of developing AV block, and the need for pacemaker implantation. Although 50% of cardiac conduction disorders occur during implantation, 44% of them occur within the next 3 days.10 If the 24-hour discharge is decided, it should be performed with a protocol of electrocardiographic monitoring and early detection of patients requiring pacemaker.11
Q.: Finally, in your own opinion, what patients would be eligible for minimalist TAVI and when is it ill-advised?
A.: It is going to depend on how experienced the heart team is, on the characteristics of the hospital, and on the situation of the patient always taking into consideration that the primary endpoint here is the safety and effectiveness of the procedure. The minimalist approach is a reasonable option in hemodynamically stable patients with adequate femoral accesses, collaborators, and without additional problems involving a high risk of complications like coronary occlusion. It will be gradually implemented, yet the effectiveness and quality of healthcare should not be compromised. Instead, the procedures should be performed faster, better, and adapted to the needs of the patients to avoid unnecessary tests, maneuvers, and stays.
FUNDING
None reported.
CONFLICTS OF INTEREST
None reported
REFERENCES
1. Cribier A, Eltchaninoff H, Bash A, et al. Percutaneous Transcatheter Implantation of an Aortic Valve Prosthesis for Calcific Aortic Stenosis First Human Case Description. Circulation 2002;106:3006-3008.
2. Lauck SB, Wood DA, Baumbusch J, et al. Vancouver Transcatheter Aortic Valve Replacement Clinical Pathway:Minimalist Approach, Standardized Care, and Discharge Criteria to Reduce Length of Stay. Circ Cardiovasc Qual Outcomes. 2016;9:312-321.
3. Ehret C, Rossaint R, Foldenauer AC, et al. Is local anaesthesia a favourable approach for transcatheter aortic valve implantation?A systematic review and meta-analysis comparing local and general anaesthesia. BMJ Open. 2017;7:e016321.
4. Harjai KJ, Bules T, Berger A, et al. Efficiency, Safety, and Quality of Life After Transcatheter Aortic Valve Implantation Performed With Moderate Sedation Versus General Anesthesia. Am J Cardiol. 2020;125:1088-1095.
5. Oguri A, Yamamoto M, Mouillet G, et al. FRANCE 2 Registry Investigators. Clinical outcomes and safety of transfemoral aortic valve implantation under general versus local anesthesia:subanalysis of the French Aortic National CoreValve and Edwards 2 registry. Circ Cardiovasc Interv. 2014;7:602-610.
6. Mehilli J, Jochheim D, Abdel-Wahab M, et al. One-year outcomes with two suture-mediated closure devices to achieve access-site haemostasis following transfemoral transcatheter aortic valve implantation. EuroIntervention. 2016;12:1298-1304.
7. De Palma R, Settergren M, Rück A, et al. Impact of percutaneous femoral arteriotomy closure using the MANTATM device on vascular and bleeding complications after transcatheter aortic valve replacement. Catheter Cardiovasc Interv. 2018;92:954-961.
8. Kotronias RA, Teitelbaum M, Webb JG, et al. Early Versus Standard Discharge After Transcatheter Aortic Valve Replacement. A Systematic Review and Meta-Analysis. JACC Cardiovasc Interv. 2018;11:1759-1771.
9. Kamioka N, Wells J, Keegan P, et al. Predictors and clinical outcomes of next-day discharge after minimalist transfemoral transcatheter aortic valve replacement. JACC Cardiovasc Interv. 2018;11:107-115.
10. Bagur R, Rodés-Cabau J, Gurvitch R, et al. Need for permanent pacemaker as a complication of transcatheter aortic valve implantation and surgical aortic valve replacement in elderly patients with severe aortic stenosis and similar baseline electrocardiographic findings. JACC Cardiovasc Interv. 2012;5:540-551.
11. Naveh S, Perlman GY, Elitsur Y, et al. Electrocardiographic predictors of long-term cardiac pacing dependency following transcatheter aortic valve implantation. J Cardiovasc Electrophysiol. 2017;28:216-223.
* Corresponding author: Sección de Hemodinámica - Cardiología Intervencionista, Servicio de Cardiología. Hospital Clínico Universitario Virgen de la Arrixaca, Ctra. Madrid-Cartagena, s/n, 30120 El Palmar, Murcia, Spain.
E-mail address: epbhva@yahoo.es (E. Pinar Bermúdez)