QUESTION: For starters, what is the minimalist approach to transcatether aortic valve implantation (TAVI)?
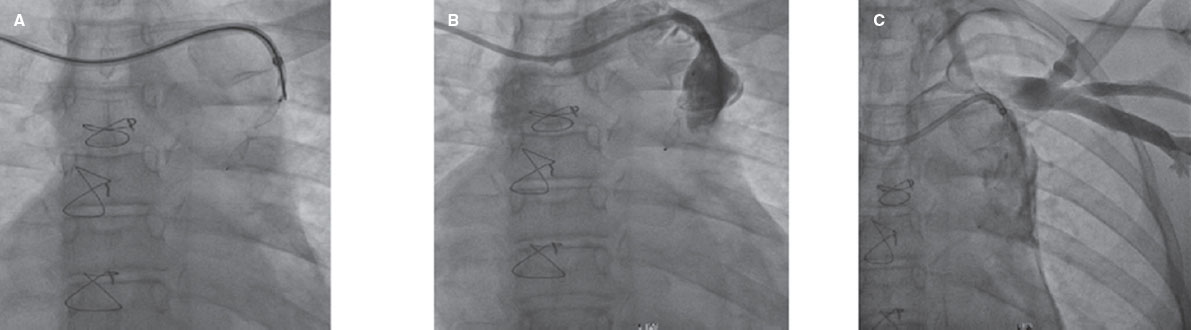
ANSWER: Minimalist TAVI is a recent strategy to simplify the procedure, reduce possible complications, and favor early hospital discharges. This general definition can be explained by 2 keys aspects: what measures should be taken? And what patients should be eligible? Replacing general anesthesia and orotracheal intubation for sedation and local anesthesia are some of these measures. Sedation with the use of a laryngeal mask airway waking up the patient once the procedure is done is an intermediate situation. The type of hospital stay following TAVI is also an important aspect to be considered and it is associated with the type of anesthesia or sedation used: intensive care unit, post-anesthesia care unit or the hospital cardiac care unit. Other minimalist approaches during the procedure would be the access site used and the percutaneous closure, to avoid bladder catheterization, use the femoral venous access, use the radial, and not the femoral, artery for monitorization purposes, and to avoid the transesophageal echocardiogram. After the implantation, promoting early walking and removing IVs as soon as possible may also help. All these measures facilitate early hospital discharges. However, the hospital stays following these minimalist measures vary in the series published. In the first series ever published,1 the average stay was 3 days including the intensive care unit stay. Recent series2 report next-day hospital discharges for patients without complications within the first 24 hours. Finally, in the pandemic era of COVID-19 even same-day hospital discharges have sometimes been proposed.3
The other key aspect we should analyze is what patients should be eligible for minimalist TAVI, something we will talk about later.
Q.: What advantages does general anesthesia have to offer and what is patient profile is the most eligible of all?
A.: The way I see it, general anesthesia is beneficial for 2 reasons mainly. The first one is that the patient will remain still for the entire procedure, which is very convenient because precision is required when moving and placing the catheters. The second one is that, in case of hemodynamic instability or serious complications, we have one healthcare professional available, the anesthesiologist, in charge of the patient’s ventilation and vital signs. This liberates the operator who can devote himself to the implantation technique alone or to solve any of the complications that may have occurred. Still, some issues still need further clarification: first, the difference between general anesthesia and sedation. In non-intubated patients, superficial general anesthesia or deep sedation can be used. These are very similar techniques with some very similar aspects that overlap. The use of the laryngeal mask airway provides versatility to adequate sedation or anesthesia for each case in particular. The anesthesiologist is free to use the technique he likes the most with one condition only, that the patient needs to «come in awake and leave the same way». Most times, laryngeal mask airways are used. They are often removed after implantation to refer the patient to the post-anesthesia care unit while awake and with spontaneous breathing. He will remain in this unit for 2 to 4 hours. Then, he will be transferred to the hospital cardiac care unit for electrocardiographic monitoring. The second aspect to be considered is the availability of the anesthesiologist. Sedation without anesthesia gives more versatility while setting everything up at the cath lab and facilitates the performance of more TAVIs regardless of the anesthesiologist’s days available. However, the drawback is that sedation is not that perfect and, in case of hemodynamic instability during the procedure, the operators will have to do 2 things: stabilize the situation, and then proceed with the implantation. Our experience is that having an anesthesiologist available is beneficial because he can provide «a la carte» sedation or anesthesia without extending the hospital stay. Also, the patient is back to the hospital cardiac care unit within a few hours.
Q.: Do you think the transesophageal echocardiography (TEE) brings added value to TAVI? In what cases would it be more indicated during the procedure?
A.: TEE was often used when this technique was born to measure the aortic annulus when the process of sizing the valve was not as standardized as it is today. The computed tomography analyzed by current software provides all kinds of measurements including diameters, perimeters, and areas allowing an accurate selection of the device and leaving the indication for TEE obsolete. Another utility of TEE during the procedure is for the early detection of complications. In patients with severe hemodynamic impairment, it facilitates the differential diagnosis of the complication immediately. Therefore, cardiac tamponade, severe ventricular dysfunction, and severe mitral or aortic regurgitation can be identified early, which in turn facilitates the rapid adoption of the necessary measures. Thrombi and aortic damage are other complications that can also be detected with this imaging modality. To this date, except for the early detection of complications, the TEE does not seem of great utility during the procedure. Since complications are rare and difficult to predict, the systematic use of TEE has been losing interest. This, added to the requirement for endotracheal intubation and longer procedural and hospital stay times4 has put its elective use to an end in most cath labs. The transthoracic echocardiography provides enough information for the decision-making process. Also, in selected cases informs of major complications like severe mitral regurgitation or aortic annulus rupture, the TEE can be used.
Q.: Vascular occlusion systems have variable, yet constant, rates of failure and complications. Do you think there are still indications for minimal access surgery? Where does your heart team stand regarding valvular accesses?
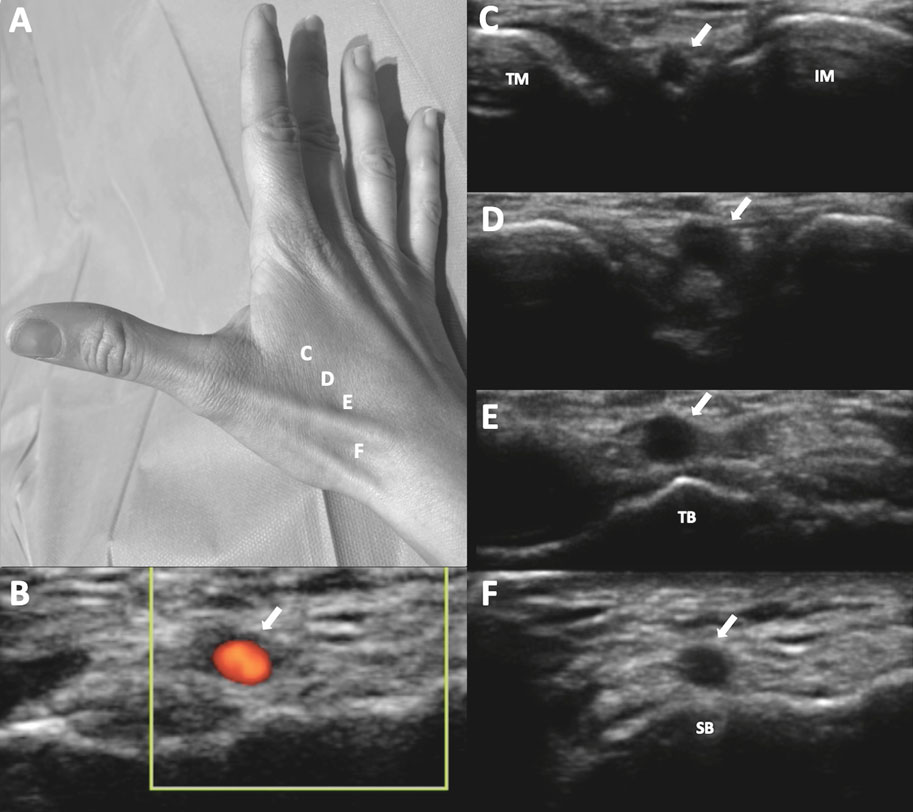
A.: I think there are no indications for minimal access surgery regarding the femoral access. Computed tomography or ultrasound-guided punctures are often used as well as percutaneous closures. Although the latter have some rate of failure, covered stent implantation from the contralateral femoral region would solve most vascular access problems. Femoral surgery is often spared for catastrophic situations only when the problem simply cannot be solved percutaneously. Therefore, from 2019 to this date, 32 failures (13%) have been reported from of a total of 239 cases regarding closures with the suture device that resolved after covered stent implantation from the contralateral femoral region. Also, only in 1 case (0.4%) emergency surgery was required. If possible, our option should always be the femoral access that, as I already said, has always been percutaneous. Elective minimal access surgery has only been used in other access routes different from the femoral one; in our own experience, it has been the subclavian access in patients with severe disease at the femoral iliac territory. Although the percutaneous approach has been described through this access route,5 we are not as experienced with it since most TAVIs can be performed percutaneously via femoral access. Other access routes that require surgery are the transcarotid and the transaortic ones, but we don’t have any experience at all here.
Q.: Regarding patients discharged after TAVI, what is the common practice at your center and what would you recommend?
A.: Ambulatory care patients without femoral complications or conduction disorders find themselves walking the next day. A transthoracic echocardiography is performed after 24-48 hours, and they are often discharged after 2 days. The causes that can delay hospital discharge are severe heart failure prior to TAVI, access site complications (whether homolateral or contralateral), the presence of fever, kidney failure, and conduction disorders. In the latter, delaying the hospital discharge is due to the decision on whether to implant a definitive pacemaker or keep the patient hospitalized while waiting for a definitive resolution of the possible intermittent disorders. A panel of experts has proposed 5 different algorithms depending on the type of conduction defect reported in baseline conditions and after the procedure.6 The goal is to standardize both the indications for definitive pacemaker implantation and the monitorization time necessary for the decision-making process. Thus, the decision to implant a definitive pacemaker cannot be made within the first 24-hours in most patients. My recommendation on hospital discharge following TAVI is to simplify procedure and convalescence as much as possible and try hospital discharge after 48 hours. When the aforementioned complications occur, the right thing to do is wait until they are solved. The algorithms mentioned6 are useful to make the decision, as soon as possible, on whether to implant a definitive pacemaker or not.
Q.: Finally, in your own opinion, what patients would be eligible for minimalist TAVI and when is it ill-advised?
A.: Although the Vancouver 3M7 criteria are wide enough to include patients in the minimalist approach to TAVI I think it should only be eligible for patients scheduled for TAVI without severe heart failure with good femoral access, no kidney failure or respiratory failure or anemia. However, it would be ill-advised in hospitalized patients with heart failure and hemodynamic instability, depressed ejection fraction or who don’t meet the aforementioned criteria. In patients with previous conduction disorders, the algorithms proposed by the panel of experts should be followed.6 As I have already said, in the presence of complications, the minimal approach to TAVI strategy should be changed and hospital discharged delayed until the complication has resolved, and the patient has fully recovered. In this context, as Albert Einstein used to say: «everything should be made as simple as possible, but no simpler».
FUNDING
None reported.
CONFLICTS OF INTEREST
None reported.
REFERENCES
1. Babaliaros V, Devireddy C, Lerakis S, et al. Comparison of transfemoral transcatheter aortic valve replacement performed in the catheterization laboratory (minimalist approach) versus hybrid operating room (standard approach):outcomes and cost analysis. JACC Cardiovasc Interv. 2014;7:898-904.
2. Kamioka N, Wells J, Keegan P, et al. Predictors and Clinical Outcomes of Next-Day Discharge After Minimalist Transfemoral Transcatheter Aortic Valve Replacement. JACC Cardiovasc Interv. 2018;11:107-115.
3. Perdoncin E, Greenbaum AB, Grubb KJ, et al. Safety of same-day discharge after uncomplicated, minimalist transcatheter aortic valve replacement in the COVID-19 era. Catheter Cardiovasc Interv. 2021;97:940-947.
4. Bhatnagar UB, Gedela M, Sethi P, et al. Outcomes and Safety of Transcatheter Aortic Valve Implantation With and Without Routine Use of Transesophageal Echocardiography. Am J Cardiol. 2018;122:1210-1214.
5. Amat-Santos IJ, Santos-Martínez S, Conradi L, et al. Transaxillary transcatheter ACURATE neo aortic valve implantation —The TRANSAX multicenter study. Catheter Cardiovasc Interv. 2020. https://doi.org/10.1002/ccd.29423.
6. Rodés-Cabau J, Ellenbogen KA, Krahn AD, et al. Management of Conduction Disturbances Associated With Transcatheter Aortic Valve Replacement:JACC Scientific Expert Panel. J Am Coll Cardiol. 2019;74:1086-1106.
7. Wood DA, Lauck SB, Cairns JA, et al. The Vancouver 3M (Multidisciplinary, Multimodality, But Minimalist) Clinical Pathway Facilitates Safe Next-Day Discharge Home at Low-, Medium-, and High-Volume Transfemoral Transcatheter Aortic Valve Replacement Centers:The 3M TAVR Study. JACC Cardiovasc Interv. 2019;12:459-469.
* Corresponding author: Servicio de Cardiología, Hospital Reina Sofía, Avda. Menéndez Pidal 1, 14004 Córdoba, Spain.
E-mail address: manuelpanalvarez@gmail.com (M. Pan).