QUESTION: Do you think there is enough evidence to indicate the use of intravascular imaging during percutaneous coronary interventions?
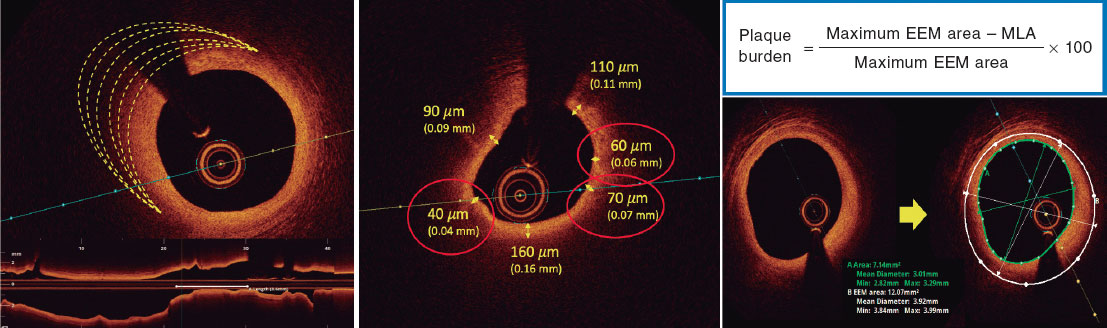
ANSWER: The appearance of intracoronary angiography was a major breakthrough for the management of ischemic heart disease. However, the limitations of this imaging modality became evident right from the start. The arrival of intravascular ultrasound (IVUS) 30 years ago now and then the optical coherence tomography (OCT) brought significant advances regarding diagnosis and percutaneous coronary intervention. Although the independent studied that compared IVUS and angiography showed variable results, several meta-analyses1 reinforce the use of the former. On the other hand, although the OCT is much newer compared to the IVUS and there is less scientific evidence supporting it, the excellent quality of its images has turned it into the imaging modality of choice for the management of complex plaques, the detection of complications during the procedure, and the assessment of stent implantation both in the clinical practice and clinical studies.
Q.: Which are the anatomical or clinical contexts with more evidence available?
A.: Both imaging modalities have proven their best cost-effectiveness ratio for the management of complex lesions. In this context, both provide very valuable information in calcified lesions. However, each of them has a specific profile with important differences between the 2.
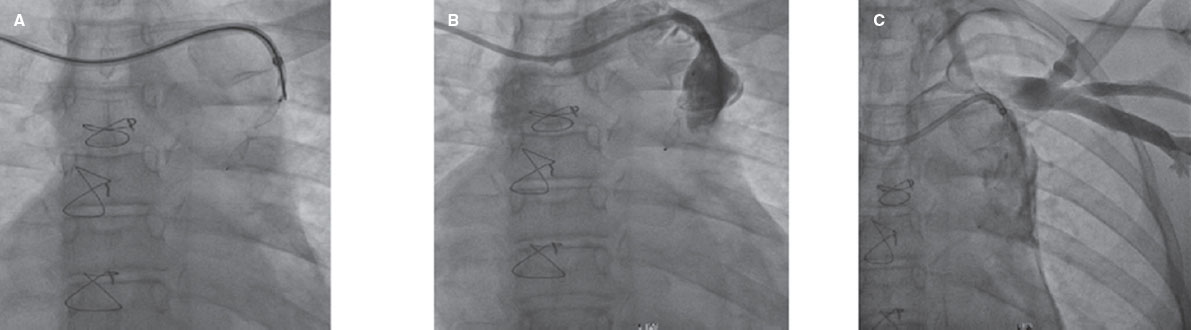
The left main coronary artery disease is the location where the IVUS has proven most beneficial because it can guide the procedure, but also in long lesions and chronic total occlusions. On the other hand, the effectiveness of IVUS in patients with conditions like diabetes or acute coronary syndrome has been confirmed in former studies.
The excellent quality of the images provided by the OCT makes it very attractive especially in 3 scenarios. In the first place, in cases of acute coronary syndrome where the angiography can show non clearly culprit stenoses, the OCT can detect the presence of dissections, eroded or ruptured plaques, small thrombi or vessel wall hematomas. The second scenario is in-stent restenosis, where it can identify underlying mechanisms like underexpansion, hyperplasia and neoatherosclerosis. Finally, it is the imaging modality of choice to study stent endothelization, a very important aspect if it can be relevant enough as to decide on the continuity or not of antiplatelet therapy and, above all, in the context of clinical studies
Q.: Is the IVUS and OCT level of evidence the same?
A.: To this day, and partly due to the fact that IVUS has been with us much longer, its scientific evidence is more solid since the OCT has less often been compared to the angiography and only to IVUS in a clinical trial.2 As a consequence, the clinical practice guidelines3 show the current scientific evidence available in the following recommendations and levels of evidence:
-
– IVUS in selected cases to optimize stent implantation: IIa B.
-
– IVUS to determine severity and optimize stent implantation in unprotected left main coronary artery disease: IIa B.
-
– IVUS or OCT to study the underlying mechanism of stent failure: IIa C.
-
– OCT in selected cases to optimize stent implantation: IIb C.
Q.: What are the advantages of OCT with respect to IVUS during percutaneous coronary interventions?
A.: Although the IVUS has 10 times less resolution than the OCT and, therefore, worse image quality, it is superior to the OCT in some aspects. The IVUS has a greater capacity to penetrate soft tissues (5-6 mm vs 1-2 mm of the OCT) and detects the total thickness of the vessel, which is an advantage when having to decide on the diameter of the stent in relation to the size of the vessel. Its second greatest advantage is that it does not require washing the artery to eliminate the red blood cells that complicate the performance of an OCT so much. Finally, in certain patients, especially those with left main coronary artery disease, and since no artery washing is required, both scientific evidence and image quality make IVUS the imaging modality of choice.
Q.: Which cases would be eligible for using IVUS and which for using OCT?
A.: The characteristics of the patient and the lesion condition the use of 1 imaging modality over the other. For example, IVUS is more adequate in cases of:
-
– Left main coronary artery disease, especially proximal: IVUS is supported by more scientific evidence as shown by the guidelines. On the other hand, in many cases, the arterial washout with contrast cannot be performed properly, which leads to suboptimal image quality with the OCT.
-
– Aorto-ostial junction, both in the left and right coronary arteries since, as we already mentioned, the OCT does not provide a proper image quality.
-
– Kidney disease or patients in whom the amount of contrast should to be limited: although a few alternatives to this have been described like the use of dextran to induce less kidney damage, in general, all these agents cause volume overload which is ill-advised in complex procedures. It is estimated that the use of OCT involves some extra 17 mL and 70 mL of contrast per case.
In the remaining scenarios, the superior image quality provided by the OCT is a very significant advantage, which means that it is the imaging modality of choice when the aforementioned situations don’t take place.
There is a subgroup of lesions where the OCT has become very popular. I am talking about bifurcations that amount to 15% of all the percutaneous coronary interventions performed these days. The use of intravascular imaging is highly recommended here since they are lesions with an associated higher rate of thrombosis and restenosis. Besides, the latter is difficult to treat, and a top level of excellence is advised in the results obtained that can be optimized with the use of imaging modalities, especially OCT. Having said this, we should always remember the limitation imposed by the use of additional contrast at the end of a complex case. Therfore, despite the fact that the image quality of IVUS is worse compared to OCT, at times it can replace it. The recent advances made in the design of new higher-resolution IVUS catheters can be an alternative to bear in mind when the use of OCT is somehow problematic.
Q.: What studies are necessary to establish the role of these imaging modalities during percutaneous coronary interventions?
A.: Since the left main coronary artery is the location where IVUS performs better and taking into consideration the current class IIa recommendation with grade B level of evidence, it would be very interesting to have studies available that would enable an upgrade to a class I recommendation. Regarding the left main coronary artery disease, these studies can also be very interesting for another reason. For example, the EXCEL and NOBLE clinical trials are no longer producing more evidence on the percutaneous revascularization of these patients. This means that «something new» should come up if we want to show additional benefits to be able to upgrade the levels of recommendations and evidence. Examples of these trials in the pipeline are (ClinicalTrials.gov):
-
– The OPTIMAL NCT04111770 clinical trial: an international, randomized, controlled, multicenter clinical trial where 800 patients will be randomized in a 1:1 ratio to undergo IVUS or angiography-guided percutaneous revascularization. Patients will be followed for 2 years after the index procedure.
-
– The INFINITE NCT04072003: a study with a similar design to the previous one with 616 patients with left main coronary artery disease with bifurcation types 1.1.1 or 0.1.1 according to the Medina classification. In the angiography group, patients will be treated with 2 stents and the implantation technique will be left to the operator’s criterion. However, in the IVUS group the lateral branch will be treated based on the lumen area as seen on the IVUS (in cases with lumen areas > 4 mm2 no stent will be implanted).
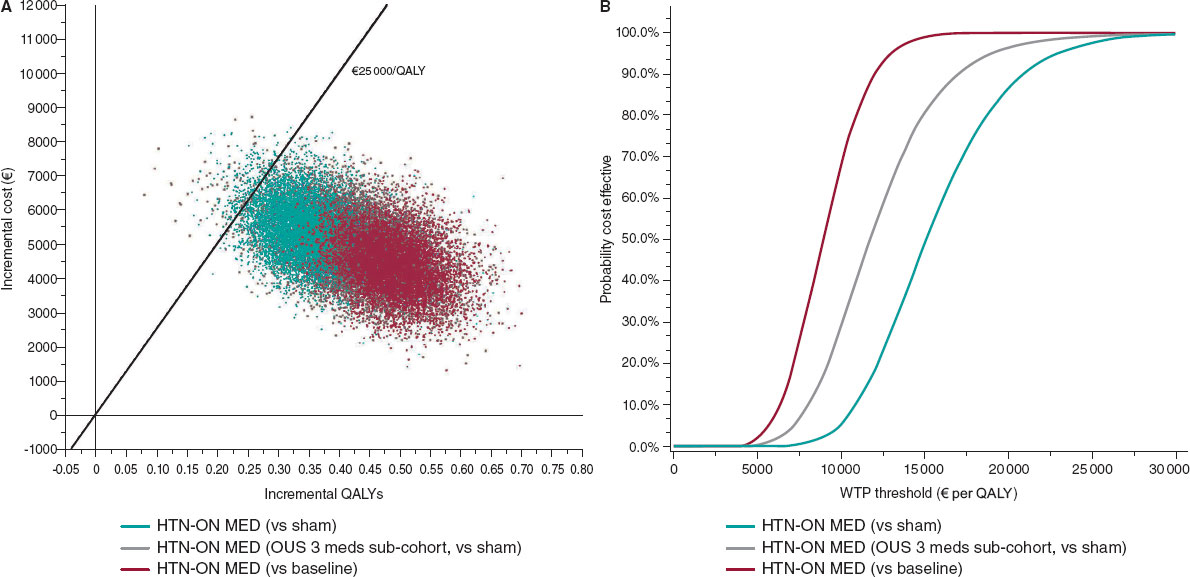
On the other hand, the situation with the OCT is different. This imaging modality has grown rapidly thanks to its excellent image quality. However, scientific support is not as strong. Added to the studies where this imaging modality is not the study primary endpoint but the tool to show the primary endpoint in subgroups of patients (acute coronary syndrome with or without ST-segment elevation and studies focused on the results of certain stents), it would be interesting to conduct clinical trials on the OCT. These studies primary endpoint would be to improve clinical results to increase the level of recommendation published by the guidelines. An example of this type of studies is the ILUMIEN IV: OPTIMAL PCI NCT03507777 where 3656 patients will be randomized in a 1:1 ratio to compare the result of angiography vs OCT-guided stenting at a 2-year follow-up.
Q.: What technical advances are available today or could be available in the near future regarding the OCT?
A.: Over the last few years, the following advances have been made regarding IVUS, some of them are still in the pipeline.
-
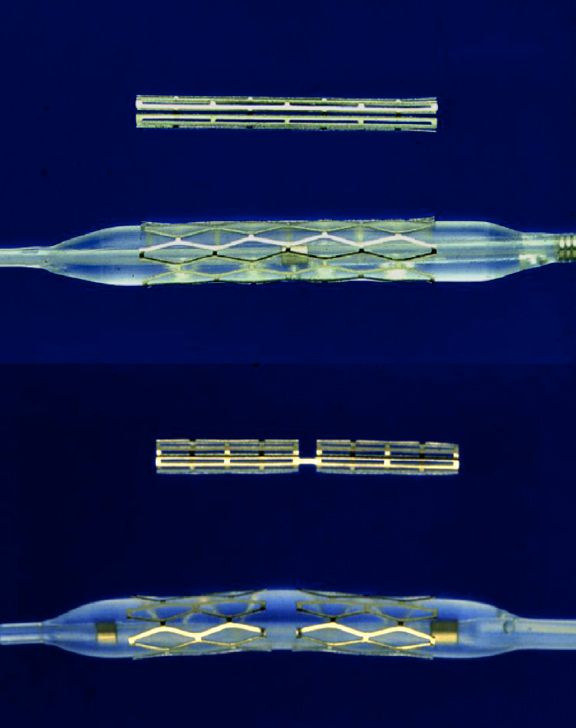
– High-definition IVUS: of up to 60 MHz and a superior image quality compared to the 20 MHz or 40 MHz IVUS. It is already available for clinical use.
-
– IVUS-angiography co-registration: this system integrates the information provided by the IVUS and the angiography in such a way that it can locate the artery of each spot analyzed by the IVUS. It is also available for clinical use.
-
– Dual-element IVUS transducer: one 35 MHz transducer to generate standard IVUS images plus another 70 MHz transducer to receive the second harmonic signals induced by the 35 MHz ultrasound. This dual transducer performs simultaneous analyses of the general anatomy through 35 MHz images and the media and adventitia layers through harmonic signals. It is still in the preclinical phase.
-
– Hybrid IVUS and OCT single transducer: undoubtedly this is the most advanced project of all by far, and it can acquire IVUS, OCT or OCT-IVUS images of the same spot with high sensitivity (up to 50 MHz for the IVUS). It is also in the preclinical phase.
REFERENCES
1. Buccheri S, Franchina G, Romano S, et al. Clinical Outcomes Following Intravascular Imaging-Guided Versus Coronary Angiography-Guided Percutaneous Coronary Intervention With Stent Implantation:A Systematic Review and Bayesian Network Meta-Analysis of 31 Studies and 17,882 Patients. JACC Cardiovasc Interv. 2017;10:2488-2498.
2. Ali ZA, Maehara A, Genereux P, et al. Optical coherence tomography compared with intravascular ultrasound and with angiography to guide coronary stent implantation (ILUMIEN III:OPTIMIZE PCI):a randomised controlled trial. Lancet. 2016;388:2618-2628.
3. Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40:87-165.
Corresponding author: Servicio de Cardiología, Hospital de Cabueñes, Avda. Los Prados 395, 33203 Gijón, Asturias, Spain.
E-mail address: inigo.lozano@gmail.com (I. Lozano).