ABSTRACT
Introduction and objectives: The final diagnosis of a myocardial infarction with non-obstructive coronary arteries (MINOCA) is often hard to achieve. Angiographic findings may be suggestive of the presence of unstable plaques although it is common to discharge patients without an etiologic diagnosis. The high spatial resolution provided by the optical coherence tomography (OCT) allows the detection of vulnerable and unstable coronary plaques that are prone to rupture, erosion, and thrombi which may lead to more targeted individual therapies. The objective of this study is to assess the utility of OCT when achieving an etiologic diagnosis in selected patients with MINOCA and high clinical suspicion of atherosclerotic etiology.
Methods: Registry of 27 patients recruited between September 2015 and January 2020 admitted to a single tertiary hospital with acute coronary syndrome and non-significant stenosis in the coronary angiography who underwent OCT. The baseline data of the study population, the angiographic and OCT findings, treatment and follow-up information were all collected.
Results: The OCT imaging showed evidence of unstable plaques (thrombus, plaque erosion or plaque rupture) in 78% of patients, which lead to an etiologic diagnosis of MINOCA. Patients were predominantly males (89%), smokers (63%), middle-aged (median 53 years old) and with a low cardiovascular risk burden. The left anterior descending coronary artery was the most frequently compromised vessel (74%) and 95% of patients ended up receiving coronary stents. The mid-term follow-up was excellent.
Conclusions: In our study, OCT imaging proved to be a valuable tool to achieve an etiologic diagnosis in a large proportion of selected patients with MINOCA which, as a result could lead to more specific and individualized treatments.
Keywords: Optical coherence tomography. Myocardial infarction with non-obstructive coronary arteries. Unstable plaque. Vulnerable plaque.
RESUMEN
Introducción y objetivos: A menudo resulta complejo diagnosticar a pacientes con infarto agudo de miocardio y estenosis coronarias no significativas en la coronariografía (MINOCA). En ocasiones, la angiografía muestra datos sugestivos de placa inestable, aunque no es infrecuente que estos pacientes acaben sin un diagnóstico etiológico. La tomografía de coherencia óptica (OCT) permite detectar placas vulnerables e inestables con rotura, erosión o trombo gracias a su elevada resolución espacial, lo que podría implicar un cambio en el manejo de estos pacientes. El objetivo de este estudio es valorar la utilidad de la OCT para alcanzar un diagnóstico final en casos seleccionados de MINOCA con alta sospecha de etiología ateroesclerótica.
Métodos: Registro de 27 pacientes desde septiembre de 2015 hasta enero de 2020 en los que se indica OCT en el contexto de síndrome coronario agudo y estenosis < 50% en la angiografía. Se describen las características de la población, los hallazgos en la angiografía y la OCT, la actitud terapéutica y la evolución.
Resultados: La OCT evidenció la presencia de placa inestable con trombo, rotura de placa o erosión de placa en el 78% de los pacientes como causa del MINOCA. Los pacientes fueron predominantemente varones (89%), fumadores (63%), de mediana edad (53 años de mediana), con poca carga de factores de riesgo y afectación principalmente de la descendente anterior (74%). El 95% de los casos en que se detectó placa inestable fueron tratados con stent. La evolución a medio plazo fue excelente.
Conclusiones: En nuestra serie de pacientes con MINOCA y alta sospecha de causa ateroesclerótica, la OCT resultó ser una técnica útil para identificar la etiología de la mayoría de ellos, lo que permitió adoptar una estrategia terapéutica más específica.
Palabras clave: Infarto de miocardio con arterias coronarias sin estenosis significativas. Placa inestable. Placa vulnerable. Tomografía de coherencia óptica.
Abbreviations:
MINOCA: myocardial infarction with non-obstructive coronary arteries. OCT: optical coherence tomography. ACS: acute coronary syndrome.
INTRODUCTION
Patients admitted with a diagnosis of acute coronary syndrome (ACS) with coronary arteries without significant angiographic obstructions (considered as angiographic stenoses < 50% of the lumen of a major epicardial vessel) should be reassessed before re-planning their diagnosis.1 In general, differential diagnosis is required with other conditions that may trigger acute myocardial damage without an acute myocardial ischemia as the underlying cause (myocarditis, stress cardiomyopathy or other cardiomyopathies, pulmonary thromboembolism, etc.). Only when these are discarded or unlikely the diagnosis of acute myocardial infarction with non-obstructive coronary arteries, also known as MINOCA, can be established.2
MINOCA amounts to between 5% and 7% of all acute myocardial infarctions, but even in some series its prevalence reaches 15% of the cases.3-5 The causes for MINOCA are varied: atherosclerotic plaque disruption (rupture or erosion), vasospasm, microvascular dysfunction, thrombus or coronary embolism, spontaneous coronary dissection or oxygen supply-demand imbalance (like in the tachyarrhythmia or anemia setting). For this reason, treatment varies significantly depending on each particular case.6 However, some studies have reported that in half of the patients no specific etiological diagnosis was established,7,8 which may lead to inappropriate treatments.
The optical coherence tomography (OCT) is an intravascular imaging modality based on the use of infrared light to acquire images with very good spatial resolution (approximately between 10 µm and 20 µm), even 10 times better resolution compared intravascular ultrasound (IVUS).9 For this reason, the OCT allows the detection of vulnerable plaques (those whose characteristics show a higher risk of destabilization) or findings suggestive that the plaque is already destabilized (table 1).10-12 Therefore, it is a useful imaging modality to establish the etiological diagnosis of MINOCA, especially when there is clinical or electrocardiographic suspicion of ACS due to atherosclerosis and also in cases of spontaneous coronary dissection.
Table 1. Pathologic findings on the optical coherence tomography
| Vulnerable plaque | Unstable plaque |
|---|---|
| Type of plaque | Thrombus |
| Macrophages | Rupture of plaque |
| Neovessels | Erosion of the plaque |
| Cholesterol microcrystals | Protruding calcium nodule with presence of thrombus or plaque disruption |
The objective of this study was to assess the utility of the OCT to establish the etiological diagnosis of patients with MINOCA and highly suspected ACS due to atherosclerosis, and describe the profile of the population studied.
METHODS
Study population
This was a prospective registry of selected cases of MINOCA in the reference center of an autonomous community between September 2015 and January 2020 with the following characteristics: a) admission with a diagnosis of ACS or recovered sudden death with suspected ACS as the underlying cause; b) angiographic coronary stenoses < 50%, and c) performance of an OCT on the possible culprit artery causing the event due to suspected angiographic imaging or ECG or segmental alterations on the echocardiogram. When in doubt on which the infarct-related culprit artery was, the vessels considered in each case were assessed using the OCT.
Procedure and analysis
The OCT was performed using the Dragonfly Optis catheter (Abbott, United States) over a pullback length of 55 mm or 75 mm in the segment of interest. The OCT study was performed in the same Ilumien Optis OCT console (Abbott). The angiographic study was performed using the Stenosis Analysis 1.6 software package (GE Healthcare, Advantage Workstation 4.5, United States). The offline analyses of the angiographic and OCT findings were performed by the same operator while the interventional procedure was being performed. This operator made the therapeutic decisions too. Afterwards, 2 expert operators performed an independent, thorough, and retrospective analysis of the angiographic and OCT images in a first reading and, simultaneously, in a second reading to achieve consensus when in the presence of suspected cases or possible discrepancies.
The following qualitative analysis were defined according to the methodology described in the OCT consensus document:12 vulnerable plaque, presence of thin-cap fibroatheroma (TCFA), macrophages, neovascularization, presence of thrombus, erosion of the plaque, ruptured plaque, and protruding calcium nodule. Unstable plaque is defined as a plaque with a thrombus, ruptured plaque, erosion of the plaque or protruding calcium nodule with thrombus or plaque disruption as seen on the OCT. Quantitative analysis was performed for every 1 mm interval while the software automatically calculated luminal dimension. The results of patients treated with a stent and those who underwent a new OCT after the implant were confirmed by verifying the adequate position, expansion, and lack of large dissections of the borders of the stent.
Statistical analysis
Quantitative variables with a normal distribution were expressed as mean and standard deviation. Those without a normal distribution were expressed as median and interquartile range [IQR]. Finally, qualitative variables were expressed using percentages as the frequency measure.
RESULTS
The registry included 27 patients. A total of 28 arteries through 38 OCT pullbacks were studied. Results are shown on table 2.
| Demographic and clinical variables of the patients (n = 27) | |
|---|---|
| Age | 53 [45-64] |
| Female sex | 3 (11) |
| Smoking | 17 (63) |
| Dyslipidemia | 12 (44) |
| Arterial hypertension | 10 (37) |
| Diabetes mellitus | 1 (4) |
| Indication for coronary angiography: | |
| NSTEACS | 17 (63) |
| STEACS | 6 (22) |
| Sudden death with suspected ACS | 4 (15) |
| Elevation of high-sensitive troponin I levels | 20 (74) |
| LVEF | 61 ± 9 |
| Findings of the coronary angiography | |
| Stenosis as seen on the visual angiographic assessment, % | 40 [30-40] |
| Stenosis as seen on the quantitative coronary angiography assessment, % | 41.2 [35.5-48.4] |
| Suspected vessels on the coronary angiography | |
| LAD | 20 (74) |
| Cx | 1 (4) |
| RCA | 7 (26) |
| Angiographic characteristics of the lesion | |
| Irregular lesion | 9 (33) |
| Image of an ulcer | 3 (11) |
| Calcified lesion | 3 (11) |
| Smooth lesion | 15 (56) |
| Angiographic thrombus | 2 (7) |
| Long lesion | 6 (22) |
| Variables of the OCT | |
| Minimum lumen area, mm2 | 3.2 [2.5-4.9] |
| Vulnerable plaque | 23 (85) |
| TCFA | 18 (67) |
| Lipid core > 90% of the vessel area | 13 (48) |
| Protruding calcium nodule | 2 (7) |
| Neovessels | 15 (56) |
| Macrophages | 16 (59) |
| Measure of the TCFA fibrous layer, µm | 63 ± 7 |
| Unstable plaque | 21 (78) |
| Thrombus | 19 (70) |
| Rupture | 8 (30) |
| Erosion | 11 (41) |
| Protruding calcium nodule with thrombus/plaque disruption | 2 (7) |
| Variables of the OCT | |
| Other causes for MINOCA found on the OCT: hematoma/spontaneous coronary dissection | 2 (7) |
| OCT post-stent implantation | 15 de 20 casos (75) |
| Underexpansion | 1 (7) |
| Malapposition | 1 (7) |
| Dissection of the borders | 1 (7) |
| Therapeutic approach | |
| Perform PCI after OCT with findings suggestive of plaque | 20 de 21 casos (95) |
| Perform PCI after OCT without findings suggestive of plaque | 0 de 6 casos (0) |
| Progression | |
| Death during admission | 0 (0) |
| Death during follow-up | 1 (4) |
| Cardiac death | 1 (4) |
| Follow-up, months | 4 [1-19] |
|
ACS, acute coronary syndrome; Cx, circumflex artery; LAD, left anterior descending coronary artery; LVEF, left ventricular ejection fraction; MINOCA, myocardial infarction with non-obstructive coronary arteries; NSTEACS, non-ST-segment elevation acute coronary syndrome; OCT, optical coherence tomography; PCI, percutaneous coronary intervention; QCA, quantitative coronary angiography; RCA, right coronary artery; STEACS, ST-segment elevation acute coronary syndrome; TCFA, thin-cap fibro-atheroma. Unless specified otherwise, data are expressed as no. (%), mean ± standard deviation or median [interquartile range]. |
|
The patients’ mean age was 53 years [45-64]. Most of them were males (89%). Smoking was the main cardiovascular risk factor (63%). The most common indication for the coronary angiography was non-ST-segment elevation ACS (63%).
The median angiographic stenosis obtained through visual analysis was 40% [30-40]. In 5 cases the stenosis assessed through visual estimation was between 50% to 60%; according to the quantitative coronary angiography the median stenosis was 41.2% [35.5-48.8]. The quantitative coronary angiography showed a 50% to 60% stenosis in 2 cases only. In all of the patients the initial TIMI flow was normal (Thrombolysis in Myocardial Infarction [TIMI] grade 3). The vessel most often damaged was the left anterior descending coronary artery (74%). In most patients the angiographic imaging did not show any signs indicative of an unstable plaque. The angiographic imaging was suggestive of a thrombus and an ulcer in 2 and 3 cases, respectively. No thromboaspiration was performed in any of the patients.
Regarding the OCT findings, the median minimum lumen area was 3.2 mm2 [2.5-4.9]. In most of the cases different types of vulnerable plaque were found in the form of a TCFA (67%), macrophages (59%), and neovessels (56%). The OCT showed signs of unstable plaque in 21 cases (78%) with thrombus in 70% of the patients. The erosion of the plaque was the main cause for plaque instability (41%) followed by the rupture of the plaque (30%). A decision was made to implant a stent in 20 of the 21 patients (95%) with data of unstable plaque as seen on the OCT. One patient with plaque erosion received medical therapy. The 6 patients without data of unstable plaque on the OCT received medical therapy too. In 75% of the cases with stenting the outcomes were assessed using the OCT; 5 out of the 20 cases were postdilated and an additional overlapping stent was implanted in 1 out of the 20 cases.
Finally, no sudden deaths were reported during the index event. At the median 4-month follow-up only 1 death due to cardiovascular causes was reported.
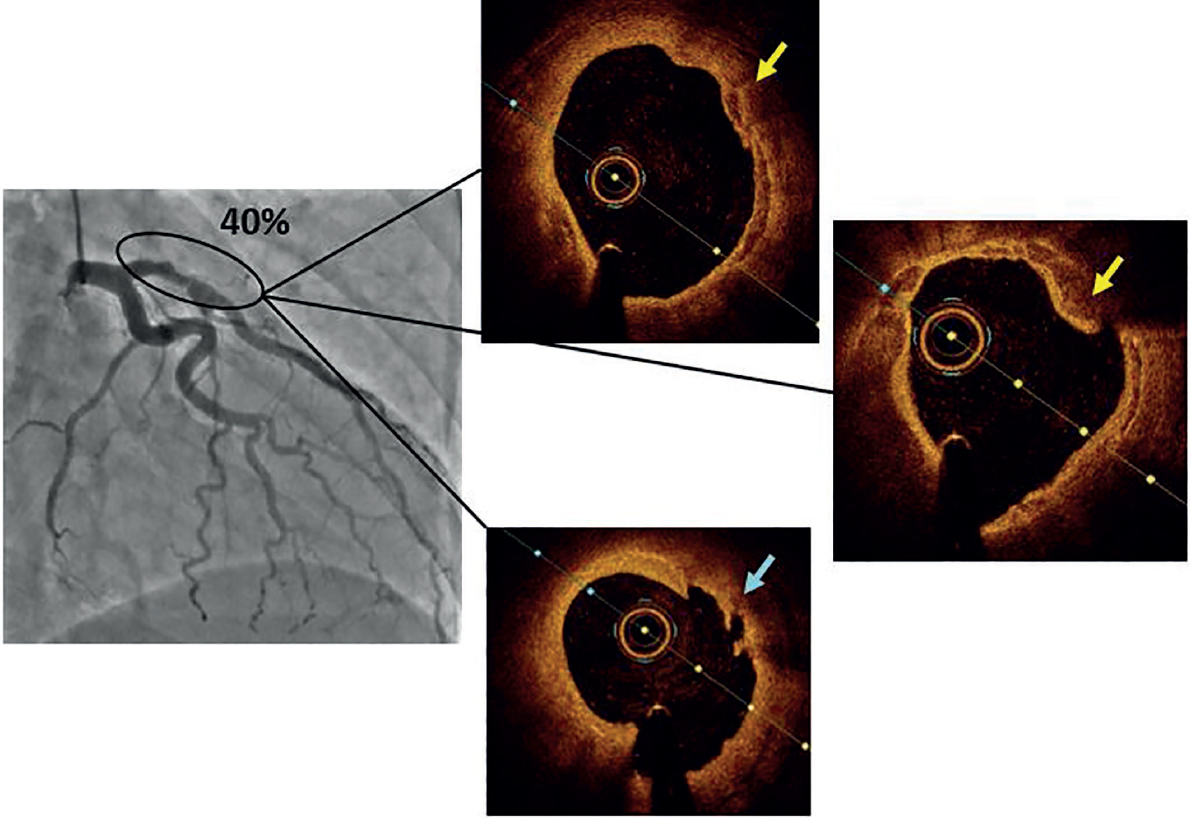
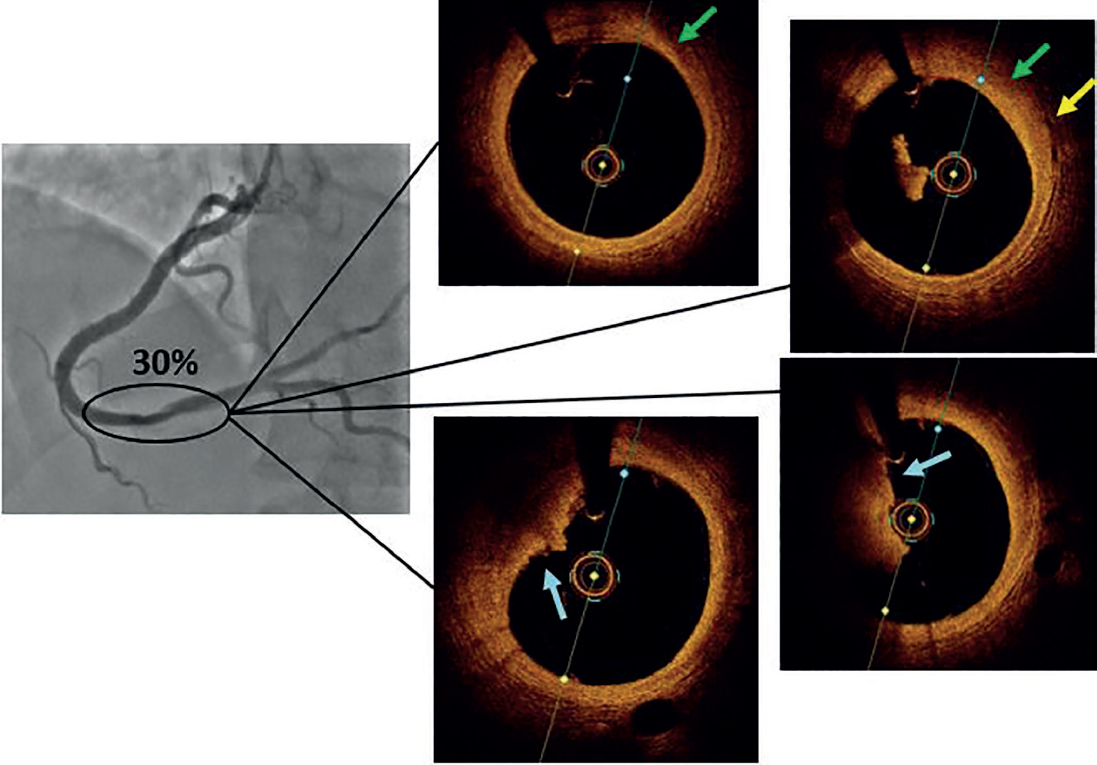
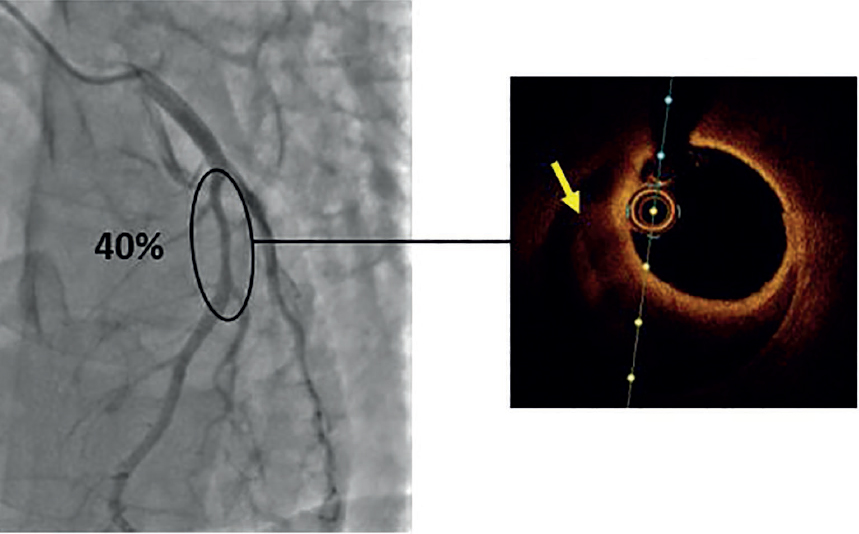
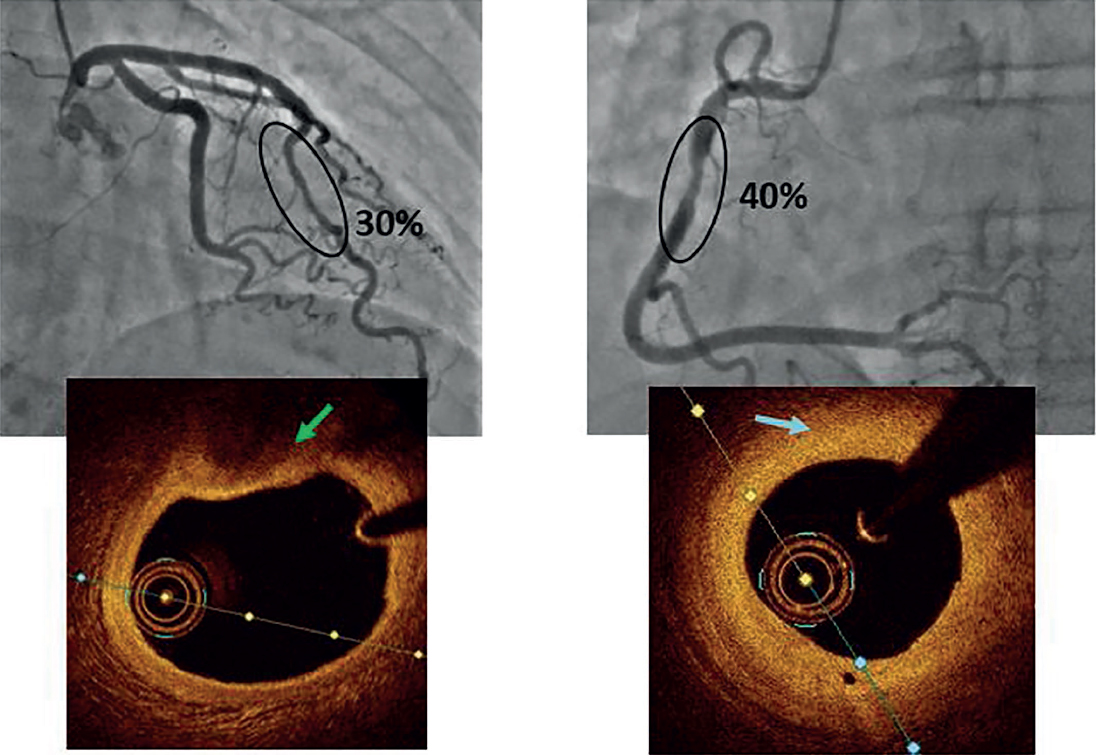
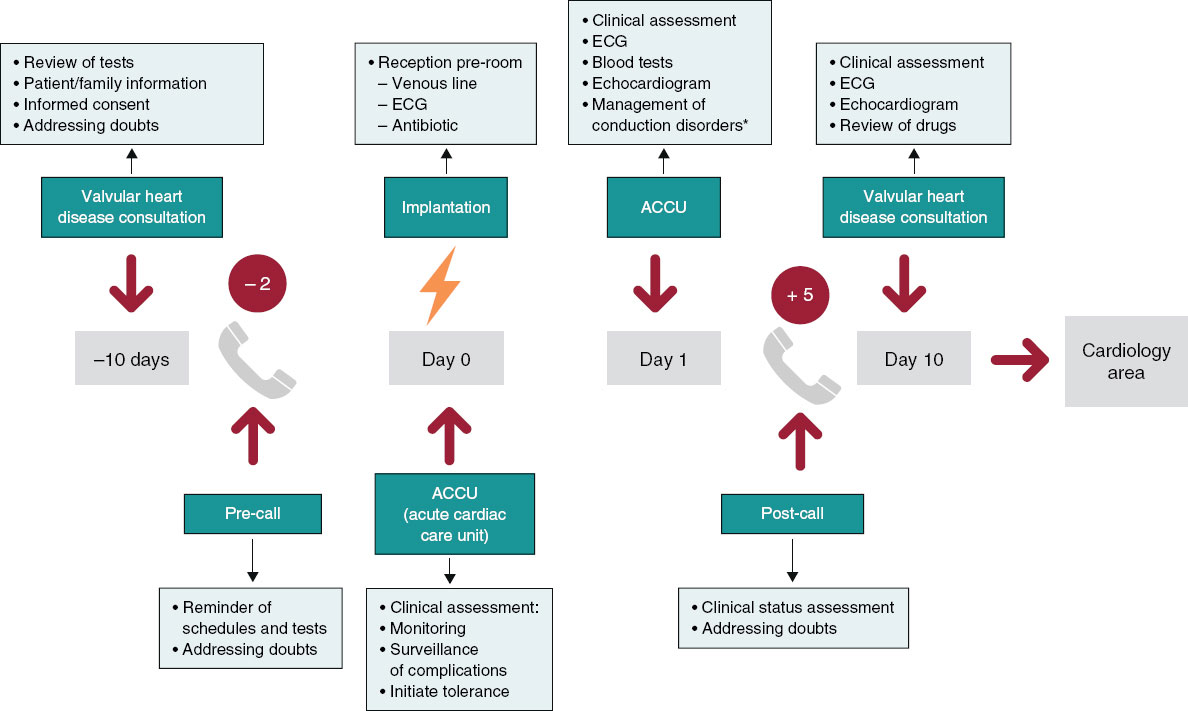
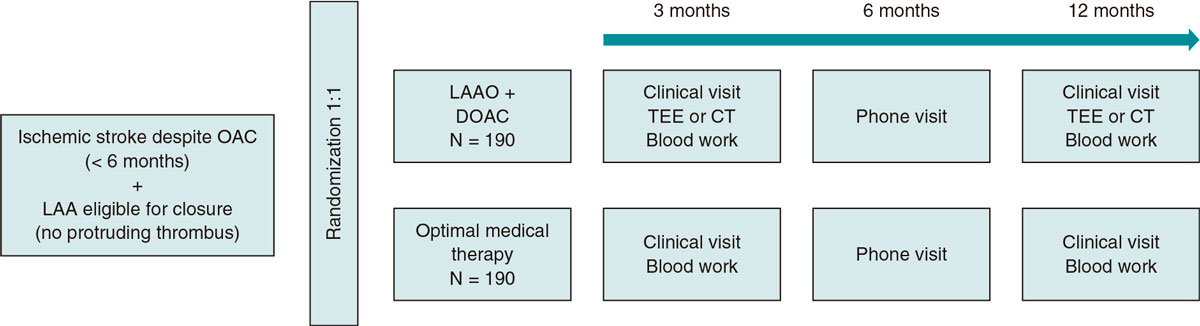
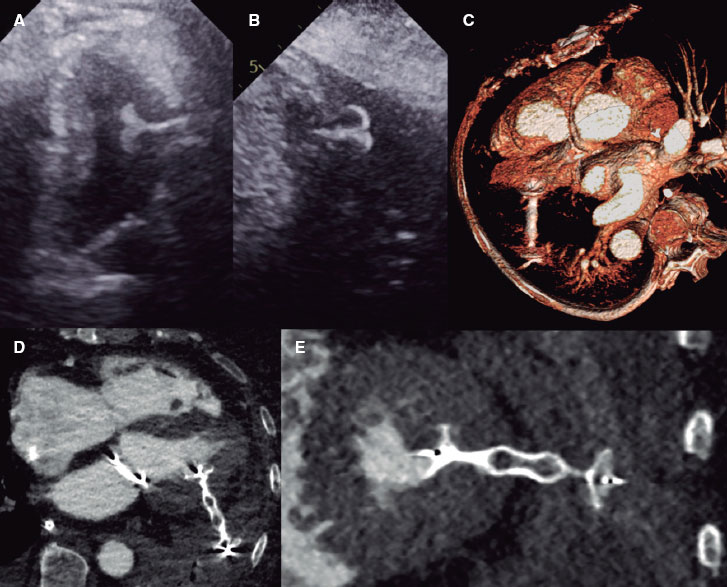
Figure 1, figure 2, figure 3, and figure 4 show the 4 cases included in the registry together with the images obtained on the coronary angiography and OCT.
Figure 1. Sixty-nine years-old male patient admitted with a non-ST-segment elevation acute coronary syndrome. Smoking is the only relevant past medical history. High-sensitivity troponin I peak levels of 293 ng/L and preserved left ventricular ejection fraction. The coronary angiography reveals the presence of a non-significant plaque (40%) by visual estimation in the left anterior descending coronary artery. The optical coherence tomography reveals the presence of fibrocalcic plaques with calcium nodules (yellow arrow) protruding into the endovascular lumen to eventually rupture the plaque (blue arrow). Findings of scarce content of white thrombus.
Figure 2. Forty-year-old male patient admitted with an ST-segment elevation acute coronary syndrome. High-sensitivity troponin I peak levels of 5000 ng/L and normal left ventricular ejection fraction. The coronary angiography reveals the presence of a non-significant plaque (30%) in the distal right coronary artery. The optical coherence tomography reveals the presence of vulnerable plaques with the shape of a fibro-lipid plaque (green arrow) and neovessels (yellow arrow). Afterwards, it confirms the presence of a massive amount of thrombus, but the discontinuity of the intima layer cannot be identified (blue arrow) suggestive that it is plaque erosion.
Figure 3. Thirty-five-year-old male patient. He is a smoker who is admitted with a non-ST-segment elevation acute coronary syndrome, high-sensitivity troponin I peak levels of 2796 ng/L, and a normal left ventricular ejection fraction. The coronary angiography reveals angiographic diffuse thinning of the left anterior descending coronary. The optical coherence tomography reveals a very well-established low-signal region surrounding the vessel lumen (yellow arrow) suggestive of hematoma.
Figure 4. Fifty-nine-year-old female patient admitted with a diagnosis of sudden death of cardiac origin after chest pain. The coronary angiography reveals the presence of non-significant plaques in the left anterior descending coronary artery (LAD) and right coronary artery (RCA). Facing the possibility that either one of them could have destabilized, an optical coherence tomography is performed in both arteries without findings of unstable plaques. A fibro-lipid plaque is seen in the LAD (green arrow) and a fibrous plaque in the RCA (blue arrow). Coronary vasospasm appears as the possible cause, but since the patient was from another country, she was transferred and the study could not be completed in our hospital.
DISCUSSION
In some series of patients with MINOCA it has been reported that in up to 50% to 70% of the cases no etiological diagnosis is established. This means that these patients may end up receiving unspecific treatment for their MINOCA.7,8 For this reason, diagnostic algorithms have been designed by expert consensus including intravascular imaging techniques as useful tools to establish the etiological diagnosis of MINOCA.2,12,13 Regarding the use of the OCT specifically for these patients, the studies have proven its capacity to detect the mechanism of the infarction in some of MINOCAs.14,15 However, although its use has been reported in some series of patients with MINOCA7,8,16 it is still scare (only 0.08% in some registries.)16 This may be due to the fact that its wide use in this type of patients has not been fully established or to the different availability and training capabilities of each center.
According to different expert consensuses2,12,13 in our center OCTs are performed on this type of patients (suspected atherosclerotic cause). This registry was started back in 2015 to later study and assess the utility of OCT in these cases since scientific evidence available on this regard is scarce in part due to its low use. Also, it would be advisable to establish a protocol to perform OCTs in most cases of MINOCA even in the absence of suspected atherosclerotic etiology; thanks to its high spatial resolution, the OCT also allows us to detect other causes for MINOCA like thromboembolisms, vasospasms or spontaneous coronary dissections.12 This was also confirmed by our study that identified 2 cases of hematoma/spontaneous coronary dissection (table 2, figure 3).12
The characteristics of this registry were those of a young population of patients (median age, 53 years), which is consistent with what has been reported by former studies. However, most of the patients included were males (89%), which varies significantly from other previous registries or reviews where over half of the patients with MINOCA were women.3,7,8,15,16 Our interpretation of these data is that our registry studied highly selected cases of MINOCA with a high clinical suspicion of atherosclerotic ACS due, which is more common in males. This would be consistent with the characteristics of the series of ACS previously reported.17 Also, when the different causes for MINOCA were analyzed, some studies have reported that when it is due to the disruption of the plaque there is a higher prevalence of male sex. However, in the occurrence of MINOCAs due to other causes, female sex is still predominant.15
According to several studies, the main clinical presentation of these patients was non-ST-elevation ACS (63%). However, there was a larger number of sudden deaths with MINOCA as the early presentation, which would be indicative of the utility of OCT for the etiological study of recovered sudden death.7,8,16
Regarding the coronary angiography findings, although the atherosclerotic cause for MINOCA was suspected, the angiography imaging were inconclusive (non-significant stenosis and scarce cases of images suggestive of plaque instability). This totally justified performing the OCT in all of the cases. The left anterior descending coronary artery was the vessel more commonly damaged, which is consistent with the results reported by other studies.15
The OCT findings show that the median minimum lumen area of the patients was 3.2 mm2. Former studies conducted with IVUS have reported on the minimum lumen area as suggestive of non-significant stenosis for which medical therapy is, therefore, preferred.18 The study conducted by Gonzalo et al.,19 that studied the value of OCT to establish the severity of intermediate angiographic stenoses (40% to 70% as seen on the quantitative coronary angiography) in patients with stable coronary artery disease revealed that the minimum lumen area as seen on the OCT to establish the concept of a functionally significant stenosis (fractional flow reserve ≤ 0.80) was 1.95 mm2. Therefore, our patients showed stenoses on the OCT without compromised coronary flows, which is consistent with the angiographic results that showed non-significant stenoses (median of 40% by visual estimation and 41.2% on the quantitative coronary angiography). However, the OCT detected the instability of the plaque in 78% of registry patients, which is why although no significant stenosis was seen (on the angiography or OCT) a decision was made to implant a stent in 95% of the cases with an unstable plaque as seen on the OCT. There is not enough evidence to support this therapeutic strategy over pharmacological treatment only.2,6,13,20-22 The EROSION trial21,22 studied conservative management (pharmacological) in cases of ACS with residual angiographic stenosis < 70% after the aspiration of a thrombus and the erosion of the plaque as the infarction mechanism. At the 1-year follow-up, 92.5% of the patients were still free from any major cardiovascular events. Therefore, conservative treatment may have been an option for a larger percentage of patients from our series. We should mention that the OCT avoided stent implantation in 6 patients in whom no unstable plaque was detected or in whom a different cause for MINOCA was found (hematoma/coronary dissection). It would be advisable to conduct randomized, prospective clinical trials to assess the possible benefit of percutaneous coronary intervention compared to pharmacological medical therapy for the management of patients with plaque disruption as the cause for MINOCA.
Mid-term patient progression was good and consistent with what has been reported by registries.7 Only 1 patient died of cardiovascular causes at the follow-up (a patient with multiple comorbidities and of an older age compared to the study median age, that is, a patient different from the population studied).
On the other hand, although this trial basically tries to identify the presence of unstable plaques on the OCT, the presence of vulnerable plaques was also studied since they are indicative of high cardiovascular risk. Thus, in most of the patients studied vulnerable plaques were found and they were often thin-cap fibroatheromas. TCFAs are considered as some of the most vulnerable plaques of all because they are made up of a lipid core (also known as lipid-rich necrotic core) covered by a very thin fibrous cap (< 65 µm) that makes them more prone to destabilization. Plaques with calcium nodules protruding towards the vessel lumen also have a higher risk of destabilization due to prospective plaque disruption, but in general they are less common. As a matter of fact, only 2 cases were found in our registry. Other findings of vulnerable plaque are the presence of macrophages (indicative of plaque inflammation), neovessels (they are immature, they can break, and cause intraplaque hemorrhage), and the size of the lipid core. all of these findings were present in over half of the study patients. Findings that are consistent with those reported by former studies.10,11,14,15
Finally, we should mention that the registry included very few patients (27) over a 4.5-year period. The largest number of patients included happened over the last 2 years. This is due to the few OCTs performed in our center to this profile of patients at the beginning of the registry with a wider use of this imaging modality after its great utility was confirmed in selected cases (figure 1 of supplementary data ). The follow-up of patient was short (median follow-up, 4 months) because over the last 6 months of the registry up to 9 patients (33%) were included and because 7 patients (26%) had a different nationality and were followed in their home countries; overall this amounts to 59% of the patients with a limited follow-up period.
CONCLUSIONS
The OCT is an intravascular imaging modality to establish etiological diagnosis in a large number of patients with MINOCA, which can lead to a better decision-making process with each particular case. Our study confirms the great accuracy of this imaging modality for the detection of unstable atherosclerotic plaques. Yet despite its proven utility and recommendation from expert consensuses, the use of this imaging modality in this type of patients is still scarce. This means that it will be necessary to establish algorithm of common actions in patients with MINOCA to avoid misdiagnosing its different etiologies.
CONFLICTS OF INTEREST
None reported.
WHAT IS KNOWN ABOUT THE TOPIC?
- MINOCAs amount to 5% to 7% of all myocardial infarctions. Different causes can trigger MINOCAs and treatment is different in each of them.
- Although there are different imaging modalities available (magnetic resonance imaging, OCT, IVUS, etc.) and their utility has been proven in the diagnosis of MINOCA, in over half of the patients the etiological diagnosis is never established.
- In part this is due to a scarce use of these imaging modalities, although expert consensuses recommend their use.
WHAT DOES THIS STUDY ADD?
- This study shows the utility of OCT to establish the etiological diagnosis of MINOCA, which reinforces the idea of a wider use of this imaging modality.
- We should mention that OCT findings can change the therapeutic approach.
- The need to conduct more specific studies to assess the best therapeutic strategy for the management of patients with MINOCA and plaque disruption.
REFERENCES
1. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction (2018). Circulation. 2018;138:618-651.
2. Tamis-Holland JE, Jneid H, Reynolds HR, et al. Contemporary Diagnosis and Management of Patients With Myocardial Infarction in the Abscence of Obstructive Coronary Artery Disease:A Scientific Statement From the American Heart Association. Circulation. 2019;139:891-908.
3. Pasupathy S, Air T, Dreyer RP, Tavella R, Bertrame JF. Systematic Review of Patients Presenting With Suspected Myocardial Infarction and Nonobstructive Coronary Arteries. Circulation. 2015;131:861-870.
4. Bainey KR, Welsh RC, Alemayehu W, et al. Population-level incidence and outcomes of myocardial infarction with non-obstructive coronary arteries (MINOCA):Insights from the Alberta contemporary acute coronary syndrome patients invasive treatment strategies (COAPT) study. Int J Cardiol. 2018;264:12-17.
5. Barr PR, Harrison W, Smyth D, Flynn C, Lee M, Kerr AJ. Myocardial Infarction Without Obstructive Coronary Artery Disease is Not a Benign Condition (ANZACS-QI 10). Heart Lung Circ. 2018;27:165-174.
6. Scalone G, Niccoli G, Crea F. Pathophysiology, diagnosis and management of MINOCA:an update. Eur Heart J Acute Cardiovasc Care. 2019;8:54-62.
7. Abdu FA, Liu L, Mohammed AQ, et al. Myocardial infarction with non-obstructive coronary arteries (MINOCA) in Chinese patients:Clinical features, treatment and 1 year follow-up. Int J Cardiol. 2019;287:27-31.
8. Reparelli V, Elharram M, Shimony A, Eisenberg MJ, Cheema AN, Pilote L. Myocardial Infarction With No Obstructive Coronary Artery Disease:Angiographic and Clinical Insights in Patients With Premature Presentation. Can J Cardiol. 2018;34:468-476.
9. Herrero-Garibi J, Cruz-González I, Parejo-Díaz P, Jang IK. Optical Coherence Tomography:Its Value in Intravascular Diagnosis Today. Rev Esp Cardiol. 2010;63:951-962.
10. Uemura S, Soeda T, Sugawara Y, Ueda T, Watanabe M, Saito Y. Assessment of Coronary Plaque Vulnerability with Optical Coherence Tomography. Acta Cardiol Sin. 2014;30:1-9.
11. Sinclair H, Bourantas C, Bagnall A, Mintz GS, Kunadian V. OCT for the identification of vulnerable plaque in acute coronary syndrome. JACC Cardiovasc Imaging. 2015;8:198-209.
12. Johnson TW, Räber L, di Mario C, et al. Clinical use of intracoronary imaging. Part 2:acute coronary syndromes, ambiguous coronary angiography findings, and guiding interventional decision-making:an expert consensus document of the European Association of Percutaneous Cardiovascular Interventions. Eur Heart J. 2019;40:2566-2584.
13. Agewal S, Beltrame JF, Reynolds HR, et al. ESC working group position paper on myocardial infarction with non-obstructive coronary arteries. Eur Heart J. 2017;38:143-153.
14. Bogale N, Lempereur M, Sheikh I, Wood D, Saw J, Fung A. Optical coherence tomography (OCT) evaluation of intermediate coronary lesions in patients with NSTEMI. Cardiovasc Revasc Med. 2016;17:113-118.
15. Opolski MP, Spiewak M, Marczak M, et al. Mechanisms of Myocardial Infarction in Patients With Nonobstructive Coronary Artery Disease:Results From the Optical Coherence Tomography Study. JACC Cardiovasc Imaging. 2019;12:2210-2221.
16. Rakowski T, De Luca G, Siudak Z, et al. Characteristics of patients presenting with myocardial infarction with non-obstructive coronary arteries (MINOCA) in Poland:data from the ORPKI national registry. J Thromb Thrombolysis. 2019;47:462-466.
17. EUGenMed Cardiovascular Clinical Study Group, Regitz-Zagrosek V, Oertelt- Prigione S, et al. Gender in cardiovascular diseases:impact on clinical manifestations, management, and outcomes. Eur Heart J. 2016;37:24-34.
18. de la Torre Hernandez JM, Hernández Hernandez F, Alfonso F, et al. Prospective application of pre-defined intravascular ultrasound criteria for assessment of intermediate left main coronary artery lesions results from the multicenter LITRO study. J Am Coll Cardiol. 2011;58:351-358.
19. Gonzalo N, Escaned J, Alfonso F, et al. Morphometric assessment of coronary stenosis relevance with optical coherence tomography:a comparison with fractional flow reserve and intravascular ultrasound. J Am Coll Cardiol. 2012;59:1080-1089.
20. Lindahl B, Baron T, Erlinge D, et al. Medical Therapy for Secondary Prevention and Long-Term Outcome in Patients With Myocardial Infarction With Nonobstructive Coronary Artery Disease. Circulation. 2107;135:1481-1489.
21. Jia H, Dai J, Hou J, et al. Effective anti-thrombotic therapy without stenting:intravascular optical coherence tomography-based management in plaque erosion (the EROSION study). Eur Heart J. 2017;38:792-800.
22. Xing L, Yamamoto E, Sugiyama T, et al. EROSION Study (effective Anti-Thrombotic Therapy Without Stenting:Intravascular Optical Coherence Tomography-Based Management in Plaque Erosion):A 1-Year Follow-Up Report. Circ Cardiovasc Interv. 2017;10:e005860.
Corresponding author: Camí de Ciutat Vell 15, 07630 Campos, Islas Baleares, Spain.
E-mail address: cmasllad@gmail.com (C. Mas Lladó).