ABSTRACT
Coronary vasoreactivity testing is a key diagnostic procedure in patients with suspected coronary spasm and research procedures intended to assess the coronary endothelial function. We should mention that coronary spasm has been observed in > 40% of the patients with angina and non-obstructive coronary stenosis. Also, that its dedicated treatment has proven to reduce ischemic symptoms and improve these patients’ quality of life. This technical report elaborated by the Working Group on Intracoronary Diagnostic Techniques of the Interventional Cardiology Association of the Spanish Society of Cardiology (ACI-SEC) summarizes the indications, preparation, performance, and interpretation of the vasoreactivity testing performed by intracoronary infusion of acetylcholine.
Keywords: Spasm provocation test. Coronary endothelial function.
RESUMEN
Las pruebas de vasorreactividad coronaria con infusión de acetilcolina son una prueba diagnóstica fundamental para pacientes con sospecha de enfermedad cardiaca secundaria a vasoespasmo y en procedimientos de investigación en los que se valora la función endotelial coronaria. Se calcula que más del 40% de los pacientes con angina y ausencia de lesiones coronarias presentan vasoespasmo como causa fundamental de los síntomas, y su tratamiento específico ha demostrado mejorar la calidad de vida en estos pacientes. El Grupo de Trabajo de Técnicas de Diagnóstico Intracoronario de la Asociación de Cardiología Intervencionista de la Sociedad Española de Cardiología (ACI-SEC) ha elaborado el presente documento técnico que expone de manera práctica las indicaciones, la preparación, la realización y la interpretación de dichas pruebas.
Palabras clave: Prueba de provocación de vasoespasmo. Función endotelial coronaria.
Abbreviations: DS: diameter stenosis. INOCA: ischemia with no obstructive coronary arteries. MINOCA: myocardial infarction with non-obstructive coronary arteries.
INTRODUCTION
Coronary vasoreactivity testing performed by intracoronary infusion of acetylcholine is basically used with 2 goals in mind: for endothelial function assessment and as a vasospasm provocation test in clinically suspicious cases. Although these tests have been known and used for decades, its use is not yet fully consolidated in our setting. This is mainly due to a scarce suspicion of myocardial ischemia due to micro or vasomotor disorders that has eventually lowered the demand for these tests. In addition, the lack of test standardization and training, the off-label use of acetylcholine, and the doubts surrounding these tests safety profile have not encouraged their widespread use in the routine clinical practice.
Over the last few years, this scenario has changed dramatically thanks to the growing evidence on the importance of diagnosing the causes of myocardial ischemia not directly related to fixed stenoses. Currently, invasive coronary spasm provocation tests are formally recommended by the European Society of Cardiology in its clinical practice guidelines on the management of chronic coronary syndromes, non-ST-segment elevation acute coronary syndromes, and ST-segment elevation acute coronary syndromes.1-3 The most common indications are to treat patients with angina or ischemia but without non-obstructive coronary lesions (ANOCA, INOCA—in this document, both coined under the term INOCA—), myocardial infarction with non-obstructive coronary arteries (MINOCA), persistent angina after coronary revascularization, obstructive coronary artery disease with clinical suspicion of associated angina of microvascular origin, and finally, patients with recovered sudden death of undetermined causes.1-3 Table 1 summarizes all clinical indications and level of recommendation to perform vasospasm provocation testing. Although this paper focuses on coronary vasoreactivity testing, we should remember that its use is often recommended simultaneously with other coronary functional testing performed using pressure guidewires like coronary flow reserve and microcirculation resistance measurements.1-5 The specific diagnosis of functional damage to coronary arteries and its targeted therapies have both improved the quality of life of patients with INOCA.6 The treatment recommended for coronary vasospasm is calcium channel blockers, nitrates, and nicorandil.6,7
Table 1. Clinical indications for the coronary vasospasm provocation test performed by intracoronary infusion of acetylcholine
| Class | Indication | Clinical specifications |
|---|---|---|
| Class I (highly recommended) | Clinical suspicion of vasospastic angina without objective documentation of ischemia or obstructive coronary artery disease in patient with chronic symptoms | – Vasospastic angina can occur predominantly at rest (35%), during exertion (30%), as a mixed pattern (30%) or dyspnea (5%)4 – The epicardial and microvascular function assessment in maximum hyperemia with a pressure guidewire is advised |
| Acute coronary syndrome without presence of culprit lesions on the coronary angiography | – Carefully review the angiography to discard embolisms and radiolucent images consistent with thrombus or coronary dissections – The use of intravascular imaging (intracoronary ultrasound or optical coherence tomography) for this type of lesions is advised – Exclude other causes for high troponin levels (like myocarditis) through segmental assessments (ventriculography or echocardiography) and magnetic resonance imaging | |
| Recovered inexplicable sudden death | – After excluding structural and/or arrhythmic heart disease | |
| Study of syncope preceded by thoracic pain | – After excluding structural and/or arrhythmic heart disease | |
| Recurrent angina despite revascularization | – First assess the pressure guidewire to exclude epicardial functional disease and microcirculation disorders in maximum hyperemia | |
| Class IIa (recommended) | Clinically documented vasospastic angina in a spontaneous event or on the non-invasive provocation test that is unresponsive to medical therapy | – Patients unresponsive to therapy with calcium channel blockers and nitrates or nicorandil – Epicardial and microvascular function assessment in maximum hyperemia with a pressure guidewire is advised |
| Class IIb (debatable) | Clinically documented vasospastic angina or on the non-invasive provocation test that responds to medical therapy to know the type and degree of vasospasm | – The specification of the macro/microvascular spasm and whether it causes the occlusion of the artery can be relevant for the patient’s prognosis – Epicardial and microvascular function assessment in maximum hyperemia with a pressure guidewire is advised |
| Class III (ill-advised) | Asymptomatic patients | Asymptomatic patients |
| Patients with ejection fractions < 35% | Patients with ejection fractions < 35% | |
| Significant epicardial coronary artery disease (left main coronary artery and/or 3 vessels) | Significant epicardial coronary artery disease (left main coronary artery and/or 3 vessels) | |
Adapted with permission from the consensus document elaborated by the COVADIS Working Group (Coronary Vasomotion Disorders International Study).5 | ||
Based on the current clinical practice guidelines, the objective of the Working Group on Intracoronary Diagnostic Techniques of the Interventional Cardiology Association of the Spanish Society of Cardiology (ACI-SEC) is to facilitate and standardize the use of coronary vasoreactivity testing. Thus, this paper has been drafted to expose all technical steps in a practical way to encourage the performance and interpretation of these tests in our setting.
NORMAL ENDOTHELIAL FUNCTION OF CORONARY ARTERIES
The modulatory function of vascular endothelium in the blood flow towards the myocardium is intrinsically associated with its metabolic characteristics. Compared to the skeletal muscle, the heart has pretty high oxygen needs (some 20 times higher). The way this oxygen supply is achieved is through very high tissue extraction at baseline: at rest the myocardium extracts approximately 70% to 80% of the oxygen transported by hemoglobin compared to 30% of the skeletal muscle. This explains why, unlike other organs, the mechanism through which the heart regulates oxygen supply to the myocardium changing metabolic needs is fast regulation and constant blood flow into the coronary system.8
Microcirculation (arteries and arterioles < 400 µm) is basically responsible for regulating coronary blood flow. Although regulation is complex and includes metabolites, hormones, neurotransmitters, and other factors, the main protagonist is the vascular endothelium that produces nitric oxide—a powerful vasodilator—in response to different stimuli. Also, other vasodilator factors—like the hyperpolarizing endothelial factor—and vasoconstrictor factors like endothelin. Endothelium-dependent vasodilation can be stimulated through different ways, but the most commonly used one is the infusion of acetylcholine.
In normal conditions, an artery with a healthy endothelium responds to acetylcholine by releasing nitric oxide that translates into vasodilation. In the presence of artery denudation from the endothelium or if the action of the nitric-oxide synthase enzyme is blocked, the artery responds to acetylcholine with vasoconstriction due to the stimulation of smooth muscle muscarinic receptors not counteracted by the nitric oxide of endothelial origin. Therefore, the infusion of acetylcholine can be used to assess endothelial function: if normal, vasodilation becomes evident. If not, vasoconstriction kicks in. The macrovascular compartment endothelial function (epicardial) can be assessed on an angiography. However, to assess the endothelium-dependent response in microcirculation, blood flow should be measured using a Doppler guidewire or thermodilution. From the macrovascular point of view, visually evident epicardial vessel vasoconstriction in response to acetylcholine is considered endothelial dysfunction. Figure 1 shows examples of vasodilation (physiological) and vasoconstriction responses (suggestive of endothelial dysfunction) to the administration of acetylcholine. From the microvascular point of view, flow reductions or increases < 50% in response to the administration of acetylcholine are considered anomalous.9 Figure 2 shows examples of microvascular function assessment using the Doppler technique or intracoronary thermodilution.
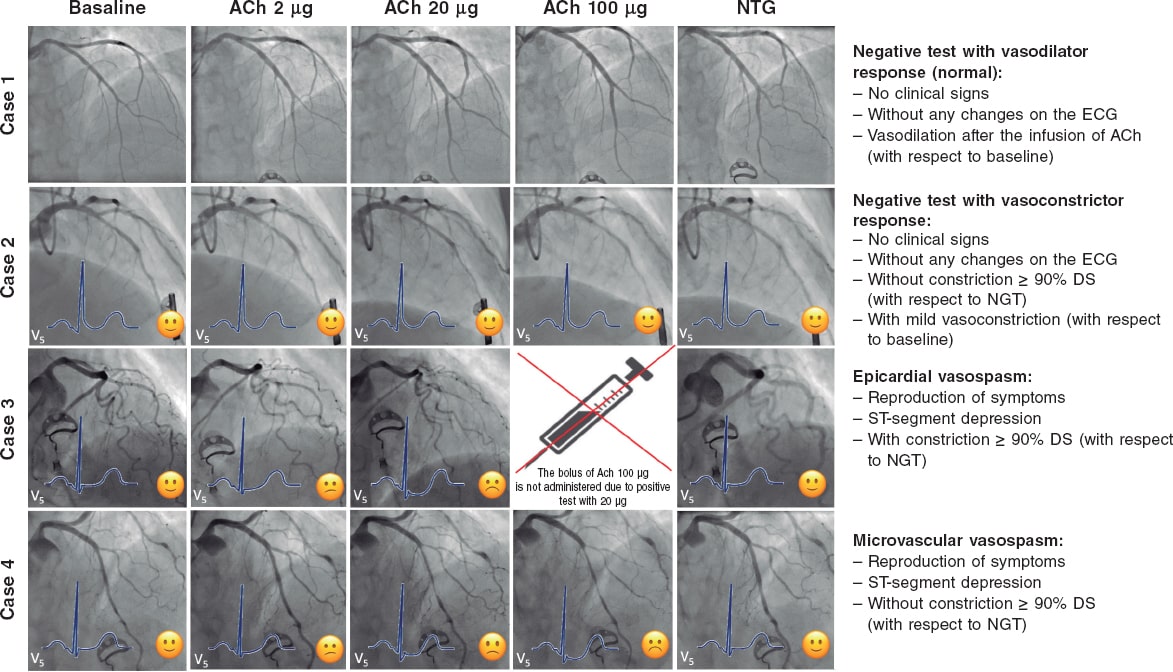
Figure 1. Possible results of the vasospasm provocation test with acetylcholine. Case 1: physiological response (vasodilator response to acetylcholine). Case 2: endothelial dysfunction with vasoconstriction with respect to baseline that does not meet the criteria for micro or macrovascular spasm. Case 3: macrovascular spasm with significant vasoconstriction of the left coronary tree. Case 4: microvascular spasm due to moderate vasoconstriction of the left tree meeting the clinical and ECG criteria for ischemia. ACh, acetylcholine; DS, diameter stenosis; NTG, nitroglycerin.
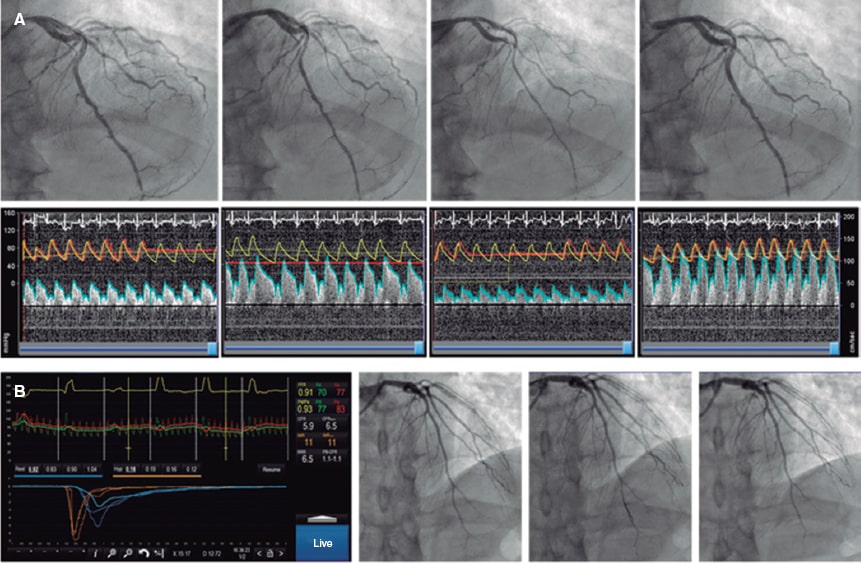
Figure 2. Combined assessment of macro and microvascular function. A: pressure-Doppler guidewire study (Combowire, Philips, The Netherlands). After the angiography and measurement of baseline flow velocity, growing doses of acetylcholine are injected. After the second dose, moderate vasoconstriction of the left anterior descending coronary artery occurs followed by an occlusive spasm at circumflex artery level plus a slower flow velocity in the left anterior descending coronary artery indicative of microvascular vasoconstriction. The spasm is solved with intracoronary nitroglycerin followed by the adenosine non-endothelium-dependent assessment of microvascular function. The patient shows macro and microvascular endothelial dysfunction and a normal non-endothelium-dependent microvascular function. B: macrovascular endothelial function assessment appears normal; adenosine non-endothelium-dependent assessment with thermodilution guidewire (Pressurewire X, Abbott, United States). Coronary flow reserve is 5.9, and the index of microcirculatory resistance is 11, which is suggestive of a normal microvascular function. In conclusion, physiological examination without any relevant findings.
CORONARY VASOSPASM PROVOCATION TESTING
Different stimuli can be used to provoque epicardial or microvascular coronary spasm. Non-pharmacological stimuli like hyperventilation or coming into contact with cold are associated with an excessive number of false negatives for clinical use. Non-invasive coronary vasospasm assessment (based on changes on the ECG or the echocardiography through the IV administration of ergonovine) is associated with a risk of causing nitrate-resistant flow-limiting coronary spasm.4 For this reason, to this date, invasive studies based on the intracoronary administration of drugs are considered the single most sensitive and safe method. Actually, to this date, it is the method recommended by European guidelines and consensus docments.2,7 The direct administration of drugs allows us to use lower doses and establish a time correlation between the development of coronary spasm followed by symptom onset and changes on the ECG. Also, it facilitates immediate treatment through the direct administration of nitrates.4,10 The use of acetylcholine vs ergonovine is advised too since the former acts on a specific pathway (by stimulating cholinergic receptors only), and its safety profile is good because its half-life is shorter. Also, because it responds faster to nitrates in case of vasoconstriction.11 Also, acetylcholine allows us to assess the vascular endothelial response specifically, which is an additional advantage. The studies that compared the results of vasospasm provocation testing with acetylcholine vs ergonovine found similar sensitivity and high matching (94%) between the two. Therefore, in the presence of a negative acetylcholine test no additional studies with different drugs are advised.12
ACETYLCHOLINE
Acetylcholine is a neurotransmitter largely found in the nervous system (central, autonomous, and peripheral). It is used in the neuromuscular junction, in all synapses of the parasympathetic autonomous system, and in the first synapsis of the sympathetic nervous system. The muscarinic receptor of acetylcholine has 5 different subtypes; among them, subtype M2 is largely found in the myocardium where it reduces the heart rate and the cardiac conduction system; subtype M3 is found in the coronary arteries both in the endothelium and the smooth muscle. In the coronary arteries, the M3 receptor stimulates the contraction of the vascular smooth muscle (vasoconstriction). Also, it stimulates the endothelial production of nitric oxide that spreads into the smooth muscle reducing the concentration of calcium, and causing relaxation (vasodilation).13,14 Acetylcholine is rapidly hydrolyzed in both the neuromuscular junction and blood by the action of cholinesterases. When infused intracoronary in the doses described here, no systemic effects occur, and its cardiac effects only last a few minutes.
ACETYLCHOLINE-INDUCED ENDOTHELIAL DYSFUNCTION AND CORONARY VASOSPASM
Endothelial dysfunction is associated with the number of cardiovascular risk factors and is a well-known precursor of atherosclerosis.15 Also, the presence of endothelial dysfunction has been associated with the appearance of ischemia in the ischemia exercise test, heavier calcification and presence of necrotic and lipidic content in the vascular wall, and more cardiovascular adverse events in the long run.16-18 The prevalence of a vasoconstrictor response to the intracoronary infusion of acetylcholine, therefore, similar to an epicardial endothelial dysfunction, is variable depending on the characteristics of the patients being more common among males.19 In the studies conducted in patients with INOCA, the prevalence of endothelial dysfunction is somewhere between 45% and 75%.19,20
Although, to this point, no cut-off value has been universally accepted, it has been confirmed that moderate degrees of vasoconstriction (20% to 50%) with respect to the artery baseline diameter after the intracoronary infusion of acetylcholine have an important prognostic impact.18,21,22 Quantitative coronary angiography studies consider the variability of the technique when measuring changes in the mean luminal diameter of a segment with respect to the different doses of acetylcholine (usually the dose with the highest vasoconstriction with respect to the baseline one). Small imaging variations due to respiratory movements in every cine coronary arteriography, different limits of the study segment in the different measures taken, the analysis of diameters at different times of the cardiac cycle between the baseline image and maximum vasoconstriction, and the operator’s variability are the reasons why vasoconstriction can only be confirmed after variability is excluded from this measuring process. Several studies have established this variability (2 times the standard deviation of the percent difference) somewhere between 3% and 6%. Therfore, endothelial dysfunction is defined as a vasoconstrictor response that is greater than this variability.23,24
The pathophysiological factors of vasospastic angina, both in their macro and microvascular manifestations are less known and, also, probably multifactorial. Vasospastic angina has been associated with the presence of coronary plaques, vascular smooth muscle cell hyperreactivity, a high baseline vagal tone, hyperreactivity to sympathetic stimulation, and finally, to a significant degree of endothelial dysfunction.10 Vasospastic angina, both macro and microvascular, is more common among women.4 The traditional criteria to define vasospastic angina of macrovascular origin have been described by the Coronary Vasomotion Disorders International Study Group (COVADIS).5 In their document they describe the diagnostic criteria of this disease that go beyond the traditional definition of variant angina described by Prinzmetal et al.25. We should mention that, unlike the definition of endothelial function where baseline angiography is used as the reference, to define macrovascular spasm the COVADIS group recommends assessing the coronary spasp in the segment with the greatest constriction of all after the administration of acetylcholine and then compare it with the diameter of the same segment after the infusion of nitroglycerin.4 Also, this group recommends the use of drug provocation testing performed by intracoronary infusion of acetylcholine given its high sensitivity and specificity values (90% and 99%, respectively).26 Based on former studies and the traditional definition, the prevalence of epicardial coronary artery vasospasm, whether associated with microvascular spasm or not, occurs in 30% to 40% of the patients with INOCA.6,27
Fewer consensus documents have been published on the definition and diagnosis of microvascular spasm.28,29 Over the last few years, the appearance of thoracic pain and changes on the ECG suggestive of ischemia in response to acetylcholine and in the absence of macrovascular spasm have been accepted for the diagnosis of microvascular spasm (located in the arterioles). By this definition, 25% of the patients with INOCA meet the microvascular spasm criteria.27
TEST PERFORMED BY INTRACORONARY INFUSION OF ACETYLCHOLINE
Preparing the patient
The best way to prepare patients eligible for the coronary vasoreactivity test with acetylcholine is still under discussion. Historically, these procedures used to be performed in a dedicated procedure while avoiding and withdrawing all kinds of vasodilator drugs (like calcium channel blockers and nitrates) for, at least, 18 hours before the infusion of acetylcholine.27,30,31 However, after the publication of the randomized clinical trial CorMicA and the consensus document of the European Association of Percutaneous Coronary Interventions (EAPCI) on the study of patients with INOCA, conventional wisdom has changed.6,7 Currently, the use of intracoronary functional testing is recommended including the vasoreactivity test to acetylcholine within the same diagnostic procedure where the coronary angiography is performed.
This brings greater comfort to the patient, uses cath lab resources more efficiently, and alleviates the pressure of the hospital agenda. In any case, this procedure should be fully adapted to the needs and possibilities of every cath lab; in polymedicated patients with vasodilators or in inexperienced centers using this test the scheduled procedure should be used.
If radial access is used in patients eligible for a coronary vasoreactivity test the administration of calcium channel blockers to prevent radial spasm is ill-advised. In these cases, the administration of low doses of nitroglycerin through the introducer sheath (100 µg to 200 µg) can be considered. However, its effect will probably mostly be gone by the time acetylcholine is infused. Also, the coronary vasoreactivity test can be performed after studying microvascular function with a pressure guidewire (with the corresponding administration of intracoronary nitroglycerin before advancing the guidewire).6,7 In this case, a 2- to 3-min washout period should be observed before the infusion of acetylcholine.6,7
Finally, a specific informed consent should be obtained before running any vasoreactivity tests. Also, 12-lead ECG monitoring is required to assess the results. The use of radiotransparent wiring and electrodes is advised here to avoid interfering with the cine-fluoroscopy images obtained for each of the doses infused during coronary angiography. Figure 3 shows a schematic sample of how to prepare a patient before running a coronary vasoreactivity test with intracoronary acetylcholine.
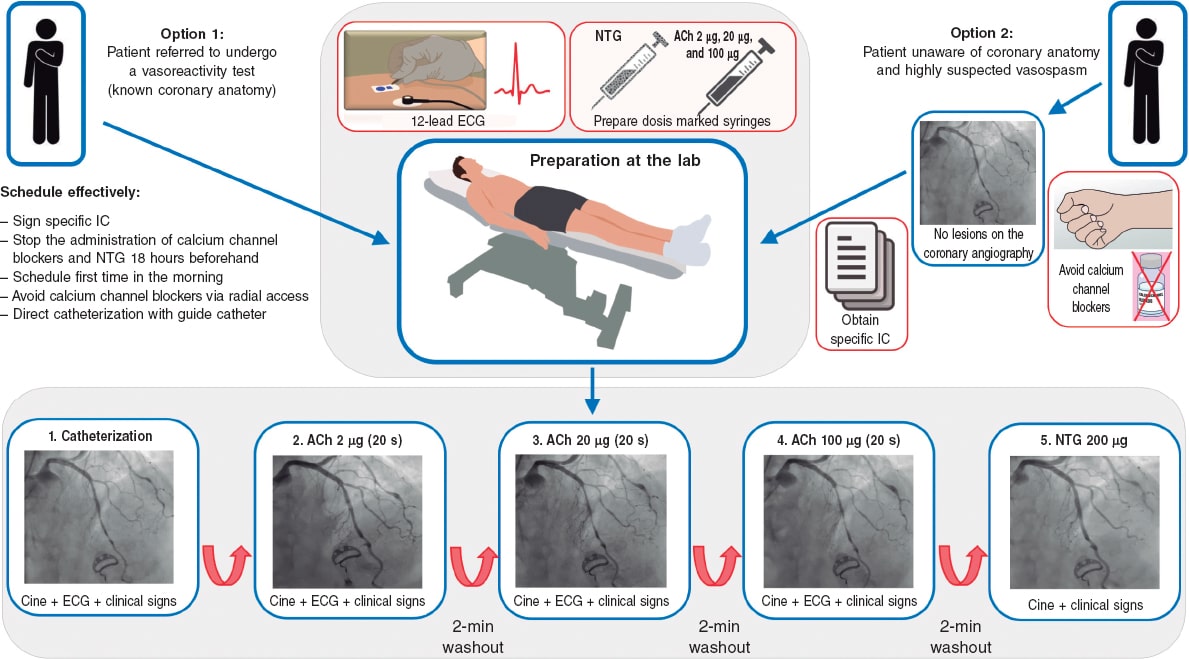
Figure 3. Preparation of the patient before running any vasoreactivity tests. ACh, acetylcholine; Ca, calcium; Cine, cine coronary arteriography; IC, informed consent; NTG, nitroglycerin.
Regarding the use of beta-blockers, certain groups also recommend their cessation before running the test to avoid any possible vasoconstrictor effects. Until more scientific data become available, the opinion of this group is that beta-blockers do not affect the results of the test significantly and in no way give false negative results.
Preparing the acetylcholine
The acetylcholine available in Spain is a preparation for the intraocular injection of 20 mg of acetylcholine chloride (powder) for its dilution in a 2 mL vial of physiological saline solution. After the solution has been prepared, the drug is still unstable, which is why the best thing to do is to prepare it right before the test; if several consecutive tests are going to be performed, the same preparation can be used. Figure 4 summarizes the way to prepare the acetylcholine solutions suggested for the test. An important safety tip is to identify correctly every solution of acetylcholine we will be using; saline solution systems and color syringes for every dose can be useful.
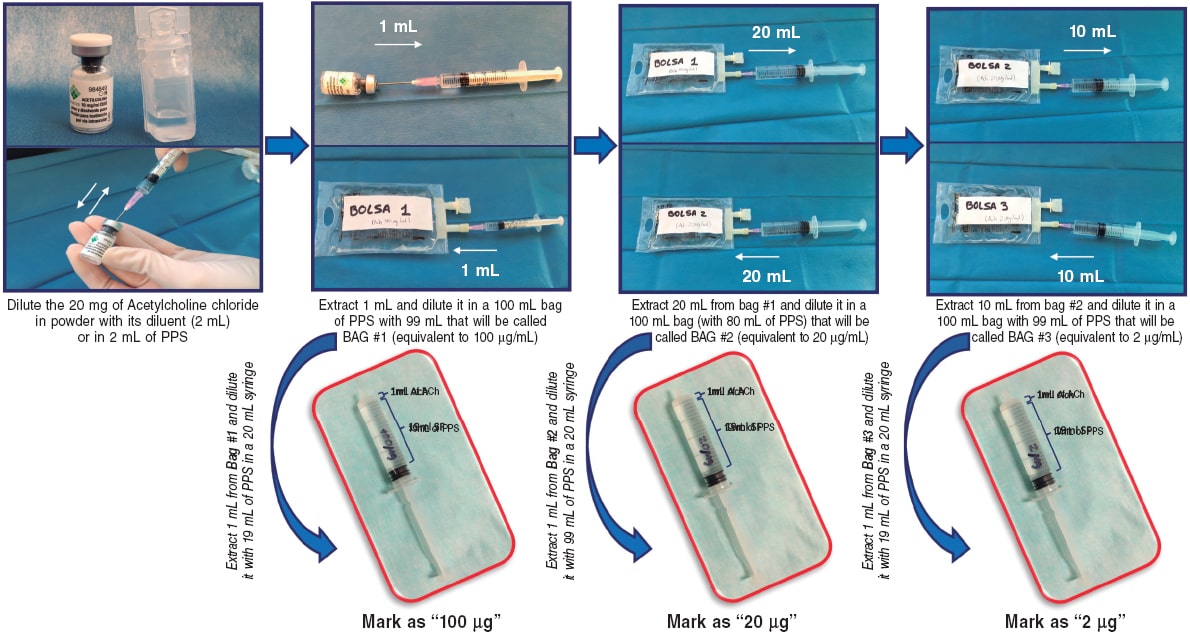
Figure 4. Preparation of growing doses of acetylcholine. ACh, acetylcholine; DS, diameter stenosis; PSS, physiological saline solution.
Intracoronary infusion protocol
Over the last 30 years, different protocols on the administration and doses of intracoronary acetylcholine have been used. Table 2 shows the different protocols used in landmark studies.6,10,19,29,30,32-34 There are differences regarding the routes of administration (manual infusion through guide catheter or controlled selective infusion into an artery through an infusion pump and microcatheter), the number of doses infused (from 2 to 4), the amount of acetylcholine used (from 0.3 µg to 200 µg), and the infusion time (from 20 seconds to 3 minutes). Below we will be seeing the most widely accepted protocols based on the objective pursued (endothelial function assessment or vasospasm provocation) followed by a proposal according to the last consensus documents published to this date.
Table 2. Comparison of the different protocols of coronary vasoreactivity to acetylcholine
| Group | Infusion method | Doses used | Infusion time per dose | Comments |
|---|---|---|---|---|
| Harvard Working Group30 | Infusion through microcatheter and infusion pump | 4 dilutions of 10–7, 10–6, 10–5, and 10–4 per liter (infusion at a rate of 0.8 mL/min) into the LCA | 2 minutes | – Designed for endothelial function assessment – A final concentration of 10–9, 10–8, 10–7, and 10–6 is estimated (equivalent to a selective total dose per artery of 0.03 µg, 0.3 µg, 3 µg, and 30 µg) – It is performed on the LCA |
| Mayo Clinic32 | Infusion through microcatheter and infusion pump | 3 dilutions of 10–6, 10–5, and 10–4 per liter (infusion at a rate of 1 mL/min) followed by a bolus of 100 µg (through the same catheter) | 3 minutes (final bolus for 20 to 30 seconds) | – Mixed protocol for endothelial function assessment (equivalent to a selective total dose per artery of 0.5 µg, 5 µg, and 50 µg) and vasospasm assessment with a bolus of 100 µg – It includes the functional assessment of microcirculation with Doppler guidewire during the infusion of acetylcholine – It is performed on the LCA |
| Korea Working Group33 | Manual infusion through guide catheter | 3 doses of 20 µg, 50 µg, and 100 µg into the LCA | 1 minute | – It is performed on the LCA |
| Japanese Circulation Society10 | Manual infusion through guide catheter | 3 doses of 20 µg, 50 µg, and 100 µg into the LCA In the absence of vasospasm 2 doses of 20 µg and 50 µg into the RCA are advised | 20 seconds | – Vasospasm provocation test on the LCA and RCA – The implantation of an electrode catheter to perform it is advised |
| Standford Working Group19 | Manual infusion through guide catheter | 4 doses of 20 µg, 50 µg, 100 µg, and 200 µg into the LCA | 1 minute | – It is performed on the LCA |
| Stuttgard Working Group34 | Manual infusion through guide catheter | 4 doses of 2 µg, 20 µg, 100 µg, and 200 µg into the LCA In the absence of vasospasm into the LCA an 80 µg dose into the RCA is advised | 20 seconds | – It studies both the LCA and the RCA |
| The CorMicA trial and the COVADIS Working Group6,29 | Mixed pump and manual infusion | 3 growing doses of 0.18 µg/mL, 1.82 µg/mL, and 18.2 µg/mL administered using an infusion pump through the guide catheter The procedure is completed with a manual bolus of 100 µg (50 µg into the RCA) | 2 minutes for every growing dose, and 20 seconds for the final bolus | – It is performed on the LCA after microcirculation assessment with adenosine through a pressure guidewire – It assesses the endothelial function and the vasospasm provocation test in the same procedure |
| Protocol of the ACI-SEC (present document) | Manual infusion through guide catheter | 3 doses of 2 µg, 20 µg, and 100 µg into the LCA In case of suspected vasospasm into the RCA the test should be started in this artery with doses of 2 µg, 20 µg, and 50 µg | 20 seconds | – For endothelial function assessment purposes, the doses should be infused more slowly for 2 to 3 minutes – It is performed on the LCA |
ACI-SEC, Interventional Cardiology Association of the Spanish Society of Cardiology; RCA, right coronary artery; LCA, left coronary artery. | ||||
Endothelial function assessment
Growing doses of acetylcholine are used for endothelial function assessment. If this procedure is performed by selective drug infusion into 1 of the main coronary vessels with a microcatheter (usually the left anterior descending coronary artery), the concentrations used are 10 moL/L to 6 moL/L, 10 moL/L to 5 moL/L, and 10 moL/L to 4 moL/L. Considering the left anterior descending coronary artery flow (some 80 mL/min), it is estimated that the drug reaches concentrations that are 100 lower in coronary microcirculation. Using the microcatheter these dilutions are injected the into the proximal left anterior descending coronary artery or into the artery to be interrogated at a rate of 1 mL/min for 3 minutes or 2 mL/min for 2 minutes through an infusion pump.24,35 Infusion starts with the least concentrated dilution and, if no complications or overt vasospasm are reported the next infusion should start 2 to 3 minutes later. In practice, this method injects 0.5 µg, 5 µg, and 50 µg of acetylcholine in each of the doses. As already mentioned, in the presence of a non-dysfunctional vascular endothelium, the physiological response is the vasodilation of major epicardial vessels.
The procedure described, although widely used in clinical trials, is somehow complicated and expensive, which is why easier and more practical alternatives have been developed for macrovascular endothelial function assessment. The most important one that has already become the standard may be the one used in the ENCORE trials (Evaluation of nifedipine and cerivastatin on recovery of coronary endothelial function)36,37 consisting of the infusion of growing doses of 2 µg, 20 µg, and 100 µg directly into the left main coronary artery for 3 minutes each followed by the performance of an angiography after every dose. Also, it consists of the assessment of the arterial diameter compared to the one measured on the baseline angiography. If macrovascular endothelial function needs to be assessed, the recommendation is to follow this infusion pattern. As we will be seeing, this protocol has already been widely adopted in recent publications and, with minor changes, has become the go-to protocol for the diagnosis of coronary vasospasm although with a faster infusion of the doses.
Microvascular endothelial function can also be assessed using dedicated guidewires for the simultaneous measurement of coronary flow. In general, this procedure is performed using a Doppler guidewire (Combowire, Philips, The Netherlands),9 although the assessment can also be performed through thermodilution with thermistor-based temperature measuring guidewires (Pressurewire, Abbott, United States).38,39 Figure 2 shows 2 examples of this procedure.
Coronary spasm provocation testing
Although there are different protocols on doses and infusion times, the protocol recommended here for vasospasm provocation has been widely accepted by the most experienced groups. In addition, there are data available on its safety profile in many patients and is the protocol backed by the EAPCI in its recent consensus document.7
Three doses of 2 µg, 20 µg, and 100 µg are used in the left coronary artery, and 3 doses of 2 µg, 20 µg, and 50 µg in the right coronary artery. If the test is negative or inconclusive and the previous doses are well-tolerated, a 200 µg or a 80 µg dose can be used in the left or right coronary artery, respectively, if suspicion runs high.
Regarding the infusion time, a slow 20 second-bolus can be administered, although this is based on clinical tolerability. The highest doses, especially in the right coronary artery, often require infusions at a slower rate to avoid sinus arrest-induced bradycardia or atrioventricular block. It is important to carefully and slowly wash the guide catheter with a saline solution to avoid the sudden injection of the remaining drug into the catheter by the time the cine-fluoroscopy imaging is acquired. After every dose both the symptoms and the repolarization and angiographic changes should be assessed while paying special attention to the appearance of epicardial spasms or significant reductions of coronary flow velocity. At the end of the test, intracoronary nitroglycerin is infused (200 µg to 300 µg) and spasm is solved within a few seconds.
Safety and complications
Before indicating the test, the presence of factors that may be correlated with a risk of complications associated with the intracoronary infusion of acetylcholine should be discarded. The test should be carefully performed in patients with a past medical history of asthma or bronchospasm and serious disorders of automaticity and cardiac conduction.
Although safe in experienced hands, coronary vasoreactivity tests to acetylcholine are not stranger to potentially serious complications. These tests should always be performed paying extra care by trained personnel and ready to face the possible complications that may arise. In a metanalysis of different studies with over 6000 procedures, the rates of major (eg, ventricular arrhythmias, need for cardiopulmonary resuscitation or infarction), and minor complications (symptomatic bradycardia, transient atrioventricular block, appearance of ventricular arrhythmias or air embolism) were 1% and 6%, respectively.40 We should mention that no death was reported in this metanalysis.40 Table 3 shows the most common complications and their corresponding treatments.
Table 3. Complications associated with the intracoronary infusion of acetylcholine
| Complication | Percentage | Comment | Treatment |
|---|---|---|---|
| Bradycardia and/or transient atrioventricular block | 3.23% | More common in high doses and when infused fast, especially into the RCA | Stop the infusion for a few seconds until going back to rhythm. Study the possibility of going on with the test at a slower infusion rate |
| Appearance of atrial fibrillation | 2.38%* | It is often self-limiting, but also fast, and its clinical tolerance is poor. It is a reason to stop the test whose outcome will be undetermined | If hemodynamic tolerance is good, use antiarrhythmic drugs; if poor, study the possibility of electrical cardioversion |
| Ventricular fibrillation, ventricular tachycardia or need for resuscitation | 1.00% | Due to acute ischemia following flow-limiting vasospasm | Nitroglycerin and defibrillation |
| Shock and/or myocardial infarction | 0.07% | Due to flow-limiting spasm at multivessel or left main coronary artery level | Nitroglycerin plus inotropic support +/– ventricular support |
| Transient hypotension | 0.05% | It is often unsignificant | Stop the infusion for a few seconds until going back to rhythm. Study the possibility of going on with the test at a slower infusion rate |
| Coronary artery dissection | 0.02% | Catheter-induced coronary artery dissection | Stenting |
| Air embolism | 0.02% | Operator-dependent complication; it is more common when infusion is performed through a microcatheter. It can be serious if not treated fast | Administer oxygen at 100% and wash the artery with saline serum multiple times (after making sure there is no more air). Inotropic and/or ventricular support (or both) may be needed |
| Catheter-induced spasm | 0.02% | More common in the RCA | Try to avoid nitroglycerin in the absence of flow lost. It is often a transient phenomenon |
The percentages disclosed were estimated based on 6183 procedures reported in 9 different studies. * According to the CorMicA trial, the rate of atrial fibrillation with the fastest doses infused was 6%.6 RCA, right coronary artery. Adapted with permission from Ciliberti et al.40 | |||
During the infusion of acetylcholine, sinus bradycardia, sinus arrests or episodes of atrioventricular block are common. This is often associated with too fast infusions, especially in the right coronary artery. If these complications occur, infusion should stop for a few seconds and restarted at a slower velocity. Atrial fibrillation can sometimes occur, but it often solves spontaneously; the most persistent cases often solve after the administration of amiodarone or other antiarrhythmic drugs. If bradyarrhythmias make a comeback, the test should stop immediately or be performed with a transient pacemaker in very selected cases where the test is considered indispensable.
An unwanted effect of the test is flow-limiting vasospasm that is not well-tolerated. In general, the consequences depend on the time elapsed between the occurrence of the vasospasm and the infusion of intracoronary nitrates to reverse it. The ischemia originated can cause hypotension and ventricular fibrillation that should be treated with nitroglycerin and immediate defibrillation. To stop this from going unnoticed, the patient’s blood pressure should be checked halfway into the infusion of acetylcholine, especially after the highest doses have been infused and when injected into a dominant left coronary branch. Under no circumstance a growing dose of acetylcholine should be infused if a significant or flow-limiting spasm or any other important complication have been spotted after the infusion of lower doses. Also, we should remember that, at the end of the infusion, the guide catheter still contains 2 mL of acetylcholine dilution that should be slowly pushed with a saline solution to stop it from entering the bolus with the injection of contrast. Same as it happens with any other invasive coronary procedures, and especially in this test, preloaded nitroglycerin should be available and ready to be infused. In most of the cases its infusion causes vasodilation, and fast flow recovery without needing further doses. On the other hand, atropine is a cholinergic receptor antagonist that can be used as an antidote when necessary.
Some operators perform the vasoreactivity test using the pressure guidewire inside the coronary artery as a safety measure. This brings more stability to the catheter, provides better selective infusion of dilutions, and allows us to monitor distal pressure (that can decrease in the case of flow-limiting spasm). Also, it controls the velocity of manual infusion in case of a long infusion without a pump (temperature or velocity changes are indicative that infusion is happening too fast). However, we should remember that the passage of the guidewire itself can cause vasospasm. Actually, it can simulate pseudo-spasms in tortuous arteries due to curve rectification.
INTERPRETING THE CORONARY VASOSPASM PROVOCATION TESTING
General concepts
Interpreting this test rests on 3 basic pillars:
The reproduction of the patient’s common symptoms that motivated the test. With the last dose of acetylcholine patients often experience changes of rhythm (eg, P-wave block or bradycardia) that can cause symptoms. These disorders should be distinguished from the patient’s usual angina symptoms.
The presence of changes on the ECG suggestive of ischemia, especially if accompanied by the angina symptoms that motivate the study. This assessment is often performed a few seconds after the infusion of each dose of acetylcholine. We should remember that in the presence of epicardial spasm with decreased blood flow in some of the epicardial arteries, the ST-segment does not need to be elevated or more changes on the ECG need to be present. That is so because patient’s safety is a priority at all time. Also, we should remember that, sometimes, the same injection of contrast or saline solution causes changes on the ECG. That is why serial ECGs (or collections of registries) should be performed a few seconds after the infusion of acetylcholine and before the cine coronary arteriography required (with the corresponding infusion of contrast).
The presence of angiographic coronary spasm (macrovascular) as seen on the serial registries (with cine-fluoroscopy) after every dose of acetylcholine. Spasm is defined as an obstruction with "65; 90% stenosis with respect to the diameter of the artery in this segment after the infusion of nitroglycerin. Diameter stenosis (DS) can be determined visually or using a quantitative coronary angiography. The DS is measured by obtaining the minimal luminal diameter after the dose of acetylcholine with greater vasoconstriction (MLD_ACh) with respect to the reference vessel diameter calculated after the infusion of nitroglycerin (RVD_NTG) with the following formula:
DS = 100 – [(MLD_Ach / RVD_NTG) × 100]
In practice, it is better to use the quantitative coronary angiography on the proximal segments of major arteries than in more distal segments where the reference diameter is often small and, according to the formula described above, could underestimate the DS.
Possible test results
Figure 1 shows the 4 results that can be obtained from a vasospasm provocation test performed by the infusion of intracoronary acetylcholine:
Negative test with vasodilator response (with respect to baseline). The presence of vasodilator response without symptom onset or changes on the ECG is suggestive of a normal endothelial function at epicardial level.
Negative test with vasoconstrictor response (with respect to baseline). The presence of epicardial vasoconstriction after acetylcholine without criteria of epicardial or microvascular vasospasm (defined by the lack of symptoms, changes on the ECG or significant vasoconstriction) is indicative of endothelial dysfunction, especially if vasoconstriction is confirmed after the infusion of the first few doses. Since the vasospasm provocation test has not been designed to assess the endothelial function (that requires a slower infusion rate) a certain degree of vasoconstriction is often seen with the highest dose due to the acetylcholine-induced direct stimulation of the vascular smooth muscle, which is not necessarily suggestive of epicardial endothelial dysfunction.
Positive test for epicardial spasm. The diagnosis of epicardial vasospasm requires the 3 following simultaneous findings:
Reproduction of symptoms after the infusion of acetylcholine.
Changes on the ECG suggestive of ischemia, usually in the ST-segment (whether depression or elevation > 0.1 mV). The appearance of negative U-waves has been described too.
Spasm with a "65; 90% diameter stenosis with respect to the same segment after the infusion of nitroglycerin that can be flow-limiting, focal, multisegmental or diffuse.
Positive test for microvascular spasm. Microvascular spasm has been defined as the reproduction of common angina symptoms plus the finding of changes on the ECG indicative of ischemia (basically, ST-segment depression or elevation > 0.1 mV) in the absence of coronary spasm with a "65; 90% diameter stenosis (with respect to nitroglycerin).
LEGAL ASPECTS PERTAINING TO THE USE OF INTRACORONARY ACETYLCHOLINE
The use of drugs in off-label indications different from those approved in their instructions for use and outside the clinical trial setting like intracoronary acetylcholine for diagnostic purposes requires the approval of local pharmaceutical committees. Because the Spanish Agency of Medicines and Medical Devices accepts the use of these drugs under very particular circumstances no general consensus has been achieved and local approvals are still required.
Also, in observance of Royal Decree 1015/2009 of 19 June,41 the use of a drug through a route of administration different from the one described in the drug labeling requires the provision of information as well as the patient’s written informed consent prior to its administration. For that reason, some centers also require the signing of a specific informed consent to be able to use intracoronary acetylcholine. These documents are available on the center intranet or the hospital pharmacy.
CONCLUSIONS
Figure 5 summarizes the key takeaways of this document. In conclusion, vasoreactivity testing with acetylcholine is an essential part of the assessment of patients with non-obstructive coronary artery disease and symptoms or ischemia. The result of this assessment allows us to target specific therapies and has proven effective in the routine clinical practice. Cath labs should be prepared to perform this kind of tests, and computers should be ready to use and interpret them.
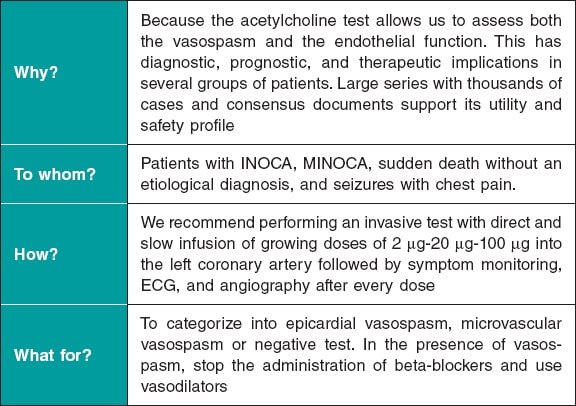
Figure 5. Key takeaways of this document. ECG, electrocardiogram; INOCA, ischemia with non-obstructive coronary arteries; MINOCA, myocardial infarction with non-obstructive coronary arteries.
FUNDING
This document had no funding whatsoever.
AUTHORS’ CONTRIBUTIONS
E. Gutiérrez and J. Gómez-Lara equally contributed to the manuscript first draft, and to the figures, and tables. The remaining authors performed a thorough revision of the paper and made comments and changes to its content and form.
CONFLICTS OF INTEREST
None reported.
REFERENCES
1. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation:The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119-177.
2. Knuuti J, Wijns W, Saraste A, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41:407-477.
3. Collet JP, Thiele H, Barbato E, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021;42:1289-1367.
4. Aziz A, Hansen HS, Sechtem U, Prescott E, Ong P. Sex-Related Differences in Vasomotor Function in Patients With Angina and Unobstructed Coronary Arteries. J Am Coll Cardiol. 2017;70:2349-2358.
5. Beltrame JF, Crea F, Kaski JC, et al.;Coronary Vasomotion Disorders International Study Group (COVADIS). International standardization of diagnostic criteria for vasospastic angina. Eur Heart J. 2017;38:2565-2568.
6. Ford TJ, Stanley B, Good R, et al. Stratified Medical Therapy Using Invasive Coronary Function Testing in Angina:The CorMicA Trial. J Am Coll Cardiol. 2018;72:2841-2855.
7. Kunadian V, Chieffo A, Camici PG, et al. An EAPCI Expert Consensus Document on Ischaemia with Non-Obstructive Coronary Arteries in Collaboration with European Society of Cardiology Working Group on Coronary Pathophysiology &Microcirculation Endorsed by Coronary Vasomotor Disorders International Study Group. Eur Heart J. 2020;41:3504-3520.
8. Duncker DJ, Bache RJ. Regulation of coronary blood flow during exercise. Physiol Rev. 2008;88:1009-1086.
9. Lerman A, Burnett JC, Jr., Higano ST, McKinley LJ, Holmes DR, Jr. Longterm L-arginine supplementation improves small-vessel coronary endothelial function in humans. Circulation. 1998;97:2123-2128.
10. JCS Joint Working Group. Guidelines for diagnosis and treatment of patients with vasospastic angina (Coronary Spastic Angina) (JCS 2013). Circ J. 2014;78:2779-2801.
11. Sueda S, Miyoshi T, Sasaki Y, Sakaue T, Habara H, Kohno H. Safety and optimal protocol of provocation test for diagnosis of multivessel coronary spasm. Heart Vessels. 2016;31:137-142.
12. Sueda S, Kohno H, Fukuda H, et al. Induction of coronary artery spasm by two pharmacological agents:comparison between intracoronary injection of acetylcholine and ergonovine. Coron Artery Dis. 2003;14:451-457.
13. Saternos HC, Almarghalani DA, Gibson HM, et al. Distribution and function of the muscarinic receptor subtypes in the cardiovascular system. Physiol Genomics. 2018;50:1-9.
14. Lamping KG, Wess J, Cui Y, Nuno DW, Faraci FM. Muscarinic (M) receptors in coronary circulation:gene-targeted mice define the role of M2 and M3 receptors in response to acetylcholine. Arterioscler Thromb Vasc Biol. 2004;24:1253-1258.
15. Gutierrez E, Flammer AJ, Lerman LO, Elizaga J, Lerman A, Fernandez-Aviles F. Endothelial dysfunction over the course of coronary artery disease. Eur Heart J. 2013;34:3175-3181.
16. Zeiher AM, Krause T, Schachinger V, Minners J, Moser E. Impaired endothelium-dependent vasodilation of coronary resistance vessels is associated with exercise-induced myocardial ischemia. Circulation. 1995;91:2345-2352.
17. Lavi S, Bae JH, Rihal CS, et al. Segmental coronary endothelial dysfunction in patients with minimal atherosclerosis is associated with necrotic core plaques. Heart. 2009;95:1525-1530.
18. Schachinger V, Britten MB, Zeiher AM. Prognostic impact of coronary vasodilator dysfunction on adverse long-term outcome of coronary heart disease. Circulation. 2000;101:1899-1906.
19. Pargaonkar VS, Lee JH, Chow EKH, et al. Dose-Response Relationship Between Intracoronary Acetylcholine and Minimal Lumen Diameter in Coronary Endothelial Function Testing of Women and Men With Angina and No Obstructive Coronary Artery Disease. Circ Cardiovasc Interv. 2020;13:e008587.
20. Ong P, Athanasiadis A, Borgulya G, Mahrholdt H, Kaski JC, Sechtem U. High prevalence of a pathological response to acetylcholine testing in patients with stable angina pectoris and unobstructed coronary arteries. The ACOVA Study (Abnormal COronary Vasomotion in patients with stable angina and unobstructed coronary arteries). J Am Coll Cardiol. 2012;59:655-662.
21. Hasdai D, Gibbons RJ, Holmes DR, Jr., Higano ST, Lerman A. Coronary endothelial dysfunction in humans is associated with myocardial perfusion defects. Circulation. 1997;96:3390-3395.
22. Hoshino M, Yonetsu T, Mizukami A, et al. Moderate vasomotor response to acetylcholine provocation test as an indicator of long-term prognosis. Heart Vessels. 2016;31:1943-1949.
23. Davis SF, Yeung AC, Meredith IT, et al. Early endothelial dysfunction predicts the development of transplant coronary artery disease at 1 year posttransplant. Circulation. 1996;93:457-462.
24. Gomez-Lara J, Oyarzabal L, Brugaletta S, et al. Coronary endothelial and microvascular function distal to polymer-free and endothelial cell-capturing drug-eluting stents. The randomized FUNCOMBO trial. Rev Esp Cardiol. 2021. https://doi.org/10.1016/j.rec.2021.01.007.
25. Prinzmetal M, Kennamer R, Merliss R, Wada T, Bor N. Angina pectoris. A variant form of angina pectoris;preliminary report. Am J Med. 1959;27:375-388.
26. Okumura K, Yasue H, Matsuyama K, et al. Sensitivity and specificity of intracoronary injection of acetylcholine for the induction of coronary artery spasm. J Am Coll Cardiol. 1988;12:883-888.
27. Ong P, Athanasiadis A, Borgulya G, et al. Clinical usefulness, angiographic characteristics, and safety evaluation of intracoronary acetylcholine provocation testing among 921 consecutive white patients with unobstructed coronary arteries. Circulation. 2014;129:1723-1730.
28. Ong P, Camici PG, Beltrame JF, et al. International standardization of diagnostic criteria for microvascular angina. Int J Cardiol. 2018;250:16-20.
29. Ford TJ, Ong P, Sechtem U, et al. Assessment of Vascular Dysfunction in Patients Without Obstructive Coronary Artery Disease:Why, How, and When. JACC Cardiovasc Interv. 2020;13:1847-1864.
30. Ludmer PL, Selwyn AP, Shook TL, et al. Paradoxical vasoconstriction induced by acetylcholine in atherosclerotic coronary arteries. N Engl J Med. 1986;315:1046-1051.
31. Takagi Y, Yasuda S, Takahashi J, et al. Clinical implications of provocation tests for coronary artery spasm:safety, arrhythmic complications, and prognostic impact:multicentre registry study of the Japanese Coronary Spasm Association. Eur Heart J. 2013;34:258-267.
32. Widmer RJ, Samuels B, Samady H, et al. The functional assessment of patients with non-obstructive coronary artery disease:expert review from an international microcirculation working group. EuroIntervention. 2019;14:1694-1702.
33. Kim JW, Park CG, Suh SY, et al. Comparison of frequency of coronary spasm in Korean patients with versus without myocardial bridging. Am J Cardiol. 2007;100:1083-1086.
34. Ong P, Athanasiadis A, Sechtem U. Intracoronary Acetylcholine Provocation Testing for Assessment of Coronary Vasomotor Disorders. J Vis Exp. 2016;114:54295.
35. Hasdai D, Cannan CR, Mathew V, Holmes DR, Jr., Lerman A. Evaluation of patients with minimally obstructive coronary artery disease and angina. Int J Cardiol. 1996;53:203-208.
36. ENCORE Investigators. Effect of nifedipine and cerivastatin on coronary endothelial function in patients with coronary artery disease:the ENCORE I Study (Evaluation of Nifedipine and Cerivastatin On Recovery of coronary Endothelial function). Circulation. 2003;107:422-428.
37. Luscher TF, Pieper M, Tendera M, et al. A randomized placebo-controlled study on the effect of nifedipine on coronary endothelial function and plaque formation in patients with coronary artery disease:the ENCORE II study. Eur Heart J. 2009;30:1590-1597.
38. Melikian N, Kearney MT, Thomas MR, De Bruyne B, Shah AM, MacCarthy PA. A simple thermodilution technique to assess coronary endothelium-dependent microvascular function in humans:validation and comparison with coronary flow reserve. Eur Heart J. 2007;28:2188-2194.
39. Diez-Delhoyo F, Gutierrez-Ibanes E, Sanz-Ruiz R, et al. Prevalence of Microvascular and Endothelial Dysfunction in the Nonculprit Territory in Patients With Acute Myocardial Infarction. Circ Cardiovasc Interv. 2019;12:e007257.
40. Ciliberti G, Seshasai SRK, Ambrosio G, Kaski JC. Safety of intracoronary provocative testing for the diagnosis of coronary artery spasm. Int J Cardiol. 2017;244:77-83.
41. Real Decreto 1015/2009, de 19 de junio, por el que se regula la disponibilidad de medicamentos en situaciones especiales. BOE núm. 174, de 20/07/2009. Available online: https://www.boe.es/eli/es/rd/2009/06/19/1015. Accessed 25 Apr 2021.
* Corresponding author: Departamento de Cardiología Intervencionista, Hospital Universitari de Bellvitge, Feixa Llarga s/n, 08907 L’Hospitalet de Llobregat, Barcelona, Spain.
E-mail address: gomezjosep@hotmail.com (J. Gómez-Lara).












