To the Editor,
The use of new technologies applied to cardiology has proven effective for the patients’ clinical improvement,1 especially in certain situations like arrhythmias, heart failure or secondary prevention.2,3
In particular, the use of smartphones applied to the healthcare networks of patients with ST-segment elevation acute myocardial infarction (STEMI) is effective to share electrocardiographic tracing and improve the coordination of the different healthcare workers involved in the management of the patients. The result is shorter primary angioplasty times.4,5
This scientific letter discusses the results of a pilot test on the working of an application for both tablets and smartphones (ODISEA APP [Myocardial Infarction Safety Transfer]) built to improve the healthcare networks of patients with STEMI (figure 1).
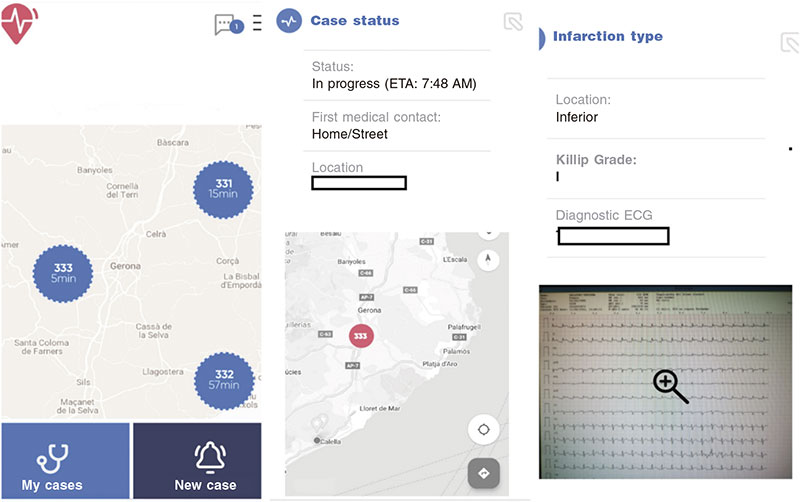
Figure 1. Screenshots from the ODISEA APP. Geolocation, data on transfer and the infarction including images from the electrocardiogram.
The primary goal of this app is to improve the coordination of the healthcare personnel involved in the management of patients with STEMI who require transfer to a PCI-capable center. This improvement should shorten primary angioplasty times and avoid unnecessary transfers. Other goals are to increase patient safety (by registering the medication administered, giving recommendations to the primary care physician, discussing doubts, etc…), improve coordination at the cath lab with elective cases, prepare, in advance, the material needed, and improve the patient’s location after the primary angioplasty.
This is how the app works: when a patient with STEMI is first helped by a primary care physician, a non-PCI-capable emergency doctor or the doctor from the emergency medical team (EMT) in the house or on the street, the app is opened with a smartphone/table using the healthcare worker’s identification and working station. Afterwards, a short questionnaire is rapidly filled out with data from the patient and the infarction. The electrocardiogram tracing is added using the camera on the smartphone or the table.
The app sends a warning message with this information to the devices the EMT physicians carry, both to coordination and to the mobile units close to the patient and the PCI-capable reference hospital cardiology personnel (interventional cardiologist, cardiologist on call, interventional cardiology nurse, and nursing team at the cardiac surgery intensive care unit).
Based on the data entered the app:
- – Creates an estimate time of diagnostic electrocardiogram-guidewire passage.6
- – Makes suggestions on the most adequate medical management and treatment for the patient (antiplatelet, anticoagulation therapy).
- – Opens a chat so the primary care physician can clear up doubts and agree on the best possible treatment with EMT physicians, the cardiologist on call, and the interventional cardiologists involved. All of them have access, in real time, to the information registered: data on the patient and the infarction sustained, electrocardiogram records, treatment administered, serious complications, etc.
If transfer for primary angioplasty is activated, the geolocation of the patient is started on the device of the EMT physician doing the transfer. From that moment onwards, the entire healthcare personnel involved can follow, in real time, the transfer of the patient to the PCI-capable hospital. The interventional cardiology unit can coordinate more precisely the elective activity of each cath lab available with up-to-the-minute information on the patient’s exact location. Also, by activating a warning message on the estimated time of arrival.
The medication administered, and serious complications reported moments before the patient gets to the cath lab are recorded.
The patient gets to the reference hospital cath lab on a treatment agreed by the entire healthcare personnel after solving all possible doubts, with all the relevant information previously known, and in perfect coordination with the entire team.
Finally, the interventional cardiologist performing the primary angioplasty adds information confirming, or not, the «Infarction Code», the angiographic result, the patient’s clinical status, the primary angioplasty times, the complications reported during the procedure, and information on the unit the patient is being transferred to. Afterwards, the case is eventually closed.
A final report is, then, created with a summary including all the data entered throughout the process that is sent to all the healthcare workers involved (primary care physician, EMT, cardiologist on call, and interventional cardiologist), which improves positive feedback.
This app has been designed in observance of all data confidentiality rules and regulations, with an obligation to authenticate, and with safe servers for data collection in full compliance with the General Data Protection Regulation (GDPR).
A pilot test was run with this app between September 2021 and January 2022. A total of 227 STEMIs transferred for primary angioplasty were included (in 98 cases the ODISEA APP was used as opposed to 129 where it wasn’t). A summary of results is shown on table 1. No significant differences were reported between both groups regarding the patient’s past medical history, the infarction location, the Killip grade or the place where the first medical contact occurred. Statistically speaking, patients treated with the ODISEA APP were further away from the PCI-capable center. A non-significant tendency was seen towards shorter primary angioplasty times (diagnostic electrocardiogram-guidewire passage) in the ODISEA compared to the NON ODISEA group (112 min vs 122 min; P = .3), a non-significant reduction of cases with times > 120 min (26.2% vs 35.7%, respectively; P = .1), and a tendency towards fewer cases eventually diagnosed as non-acute coronary syndrome (7.1% vs 13.2%; P = .1).
Table 1. Comparative summary of patients from the ODISEA APP pilot test
| ODISEA (98 patients) | NON ODISEA (129 patients) | P | |
|---|---|---|---|
| Age (mean, SD) | 61 (13.9) | 63 (13.1) | .1 |
| Women, n (%) | 21 (21.4%) | 32 (24.8%) | .5 |
| Smoking, n (%) | 44 (44.9%) | 50 (38.8%) | .3 |
| Arterial hypertension, n (%) | 48 (49%) | 59 (45.7%) | .6 |
| Dyslipidemia, n (%) | 34 (34.7%) | 54 (41.9%) | .2 |
| Diabetes mellitus, n (%) | 18 (18.4%) | 31(24%) | .3 |
| Previous AMI, n (%) | 16 (16.3%) | 16 (12.4%) | .4 |
| Previous heart surgery, n (%) | 3 (2.1%) | 2 (1.6%) | .4 |
| Anterior location, n (%) | 39 (39.8%) | 43 (33.3%) | .3 |
| Killip grade > 2, n (%) | 5 (5.1%) | 8 (6.2%) | .7 |
| Location of the first medical contact | .5 | ||
| EMT, n (%) | 35 (35.7%) | 39 (30.2%) | |
| Outpatient, n (%) | 28 (28.6%) | 36 (27.9%) | |
| Non-PCI-capable hospital, n (%) | 35 (35.7%) | 54 (41.9%) | |
| Distance in km, mean (SD) | 42 (19.3) | 36 (21.7) | .02 |
| Sudden death, n (%) | 1 (1%) | 1(0.8%) | .8 |
| Diagnostic ECG-guidewire passage time in min, mean (SD) | 112 (28) | 122 (24) | .3 |
| Patients with diagnostic ECG-guidewire passage time > 120 min, % | 26.2% | 35.7% | .1 |
| Diagnostic ECG-start of transfer time in min, mean (SD) | 32 (8) | 36 (10) | .5 |
| Transfer time until arrival at the cath lab in min, mean (SD) | 67 (21) | 70 (19) | .6 |
| Cath lab-guidewire passage time in min, mean (SD) | 17 (7) | 19 (6) | .5 |
| AMI CODE not properly indicated, n (%) | 7 (7.1%) | 17 (13.2%) | .1 |
AMI, acute myocardial infarction; ECG, electrocardiogram; EMT, emergency medical team; SD, standard deviation. | |||
Finally, we should mention that this app has been created by a working group including EMT physicians, primary care practitioners, doctors from non-PCI-capable hospitals, interventional cardiologists, and cardiologists from cardiac surgery intensive care units.
FUNDING
Grants from the following organizations were received: Catalan Society of Cardiology: Research Projects 2022, and Spanish Society of Cardiology: Research training of the ischemic heart diseases and cardiology critical care section.
AUTHORS’ CONTRIBUTIONS
All the authors contributed to the development of this application and drafted the manuscript.
CONFLICTS OF INTEREST
None whatsoever.
REFERENCES
1. Nguyen HH, Silva JNA. Use of smartphone technology in cardiology. Trends Cardiovasc Med. 2016;26:376–386.
2. Hamilton SJ, Mills B, Birch EM, Thompson SC. Smartphones in the secondary prevention of cardiovascular disease: a systematic review. BMC Cardiovasc Disord. 2018;18:25.
3. Kotecha D, Chua WWL, Fabr/itz L, et al; European Society of Cardiology (ESC) Atrial Fibr/illation Guidelines Taskforce, the CATCH ME consortium and the European Heart Rhythm Association (EHRA). European Society of Cardiology smartphone and tablet applications for patients with atrial fibr/illation and their health care providers. Europace. 2018;20:225–233.
4. Chao C-C, Chen Y-C, Shih C-M, et al. Smartphone transmission of electrocardiography images to reduce time of cardiac catheterization laboratory activation. J Chin Med Assoc JCMA. 2018;81:505–510.
5. Park JJ, Yoon C-H, Suh J-W, et al. Reduction of Ischemic Time for Transferred STEMI Patients Using a Smartphone Social Network System. J Am Coll Cardiol. 2016;68:1490–1492.
6. Aboal J. Creación y validación de un modelo de predicción para el cálculo del tiempo de angioplastia primaria en pacientes con infarto agudo de miocardio que son trasladados a un hospital con disponibilidad de hemodinámica. Tesis doctoral inédita. Universidad de Girona. Departamento de ciencias médicas. 2020. Available online: http://hdl.handle.net/10803/669976. Acceso 15 Jul 2022.












