To the Editor,
The presence of a thrombus in the left atrial appendage is a formal contraindication for its percutaneous closure and poses a serious dilemma during the therapeutic management of the patient. The option of intensifying anticoagulation to achieve the dissolution of the thrombus whether through better monitoring of the international normalized ratio (INR) parameters or through the introduction of direct anticoagulants is not often possible in most patients eligible for the percutaneous closure of the left atrial appendage. Therefore, the possibility of closing the left atrial appendage in certain cases of thrombosis (mural thrombus away from the landing zone) by using a modified technique to deploy the Amplatzer Amulet device (Abbott, United States) has been described.1
In a non-closure setting, a percutaneous method for thrombus aspiration in the left atrial appendage with a large caliber device (22-Fr) and extracorporeal circulation has been reported.2
This is the case of an 86-year-old male patient (former smoker) with hypertension and non-valvular atrial fibrillation for which he was being anticoagulated with vitamin K antagonists. The previous month, the patient had suffered a cardioembolic ischemic stroke despite anticoagulation. During that admission, the cerebral magnetic resonance performed showed cerebral amyloid angiopathy with evidence of multiple microhemorrhages and superficial siderosis. Anticoagulation was withdrawn and the patient remained on acetylsalicylic acid only. During the current admission, the patient presented with serious heart failure. In this patient with persistent stroke,3 without anticoagulation, and a high ischemic and hemorrhagic risk (CHA2DS2-VASc and HAS-BLED values of 5 and 4, respectively), doctors suggested the percutaneous closure of the left atrial appendage. The patient was informed about the characteristics and purposes of the procedure, and his informed consent was obtained for both the procedure and the processing of his data for scientific purposes.
Due to the patient’s frailty, the procedure was fluoroscopy guided only. The value of the image fusion technique has been suggested as coadjuvant to transesophageal ultrasound to guide the procedure.4 Our group, that has no intracardiac ultrasound machines available, has gained experience closing the left atrial appendage with fluoroscopy guidance only using the image fusion technique (i-Pilot, Siemens, Germany).
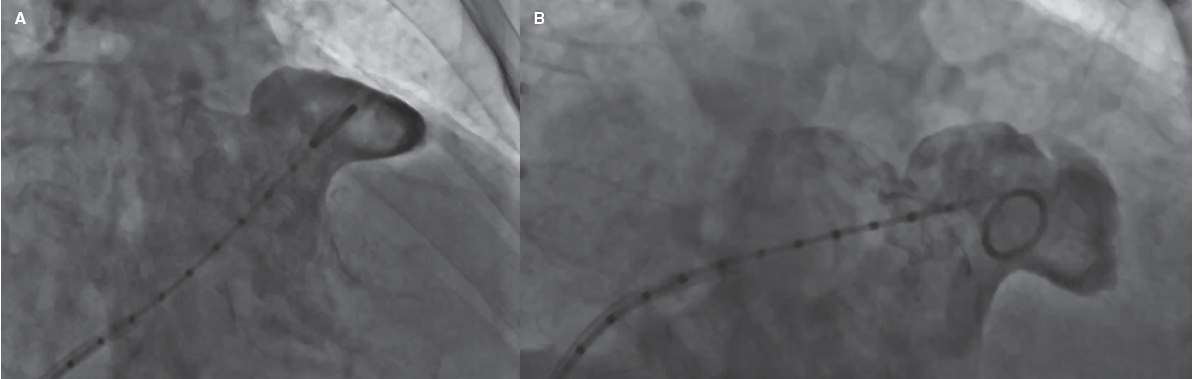
Rotational angiography revealed a left atrial appendage with windsock morphology and a larger diameter in the landing zone of 31 mm. However, it was surprising to see the presence of a mobile filling defect at the left atrial appendage main lobe of circular appearance and an approximate diameter of 1 cm (figure 1 and video 1 of the supplementary data).
Figure 1. Angiographic image in the oblique anterior right cranial (A) and caudal (B) projections. A round radiolucent image immediately distal to the pigtail catheter of approximately 10 mm in diameter can be seen.
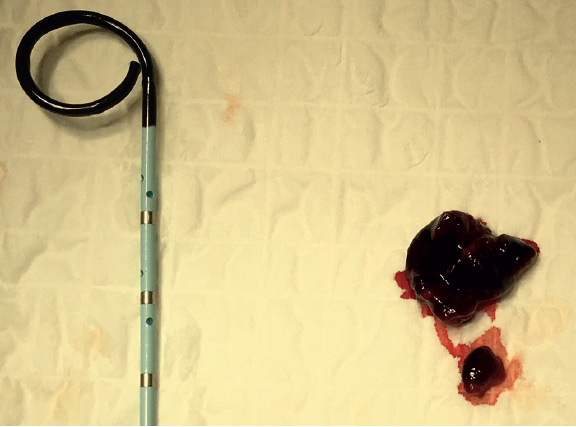
It was decided to continue the procedure with an Amplatzer Amulet device. Exchange was conducted with a 14-Fr 45° × 45° Amplatzer TorqVue delivery sheath (Abbott, United States) with a 4.8-mm internal lumen by bringing its tip towards the left atrial appendage ostium as seen using the image fusion technique. A mandatory step to avoid gas embolization in a low-pressure cavity like the left atrial appendage is to place the sheath proximal border below cardiac level, thus generating a negative pressure gradient that facilitates the outflow of blood. After a mild hemorrhagic retrograde flow, it stopped. On suspected sheath occlusion due to thrombus, a 50 mL Luer-Lock syringe was connected. Aspiration was performed with extraction of very organized thrombotic material of spherical appearance like the one seen during the angiography (figure 2).
Figure 2. Organized thrombus originated at the left atrial appendage after its aspiration through a 34-Fr sheath.
With the guidance provided by the image fusion technique an no additional angiography, the 34 mm Amplatzer Amulet device was deployed in the first attempt with good results (video 2 of the supplementary data).
The patient did not have any complications during the procedure, and he was discharged on single antiplatelet therapy with acetylsalicylic acid. At the 1-year follow-up, no new events have been reported.
In conclusion, this was the first case ever reported by the medical literature of a successful thrombus aspiration of thrombotic material in the left atrial appendage during its percutaneous closure. The maneuver was successful thanks to 3 factors: the characteristics of the thrombus (organized and mobile); the negative pressure through a catheter of large internal lumen initially exerted by the pressure gradient and then by the aspiration with the syringe; and finally, the value of the image fusion technique to guide the procedure without any additional angiographies. However, the success achieved with this particular case should not be mixed up with its recommendation: the lack of control over the thrombus behavior makes the use of cerebral embolic protection measures essential during the closure of the left atrial appendage.
FUNDING
No funding related to this work.
AUTHORS' CONTRIBUTION
R.J Ruiz-Salmerón: author of the manuscript; S. Rodríguez de Leiras, R. García de la Borbolla, C. Carrascosa-Rosillo, M. Vizcaíno-Arellano, and Carlos Robles-Pérez: critical review.
CONFLICTS OF INTEREST
R.J. Ruiz-Salmerón is proctor for Abbott for left atrial appendage clossure with Amulet.
SUPPLEMENTARY DATA
Video 1. Ruiz-Salmerón R.J. DOI: 10.24875/RECICE.M20000152
Video 2. Ruiz-Salmerón R.J. DOI: 10.24875/RECICE.M20000152
REFERENCES
1. Bordignon S, Bologna F, Chen S, et al. Percutaneous left atrial appendage closure in the presence of thrombus:A feasibility report. J Cardiovasc Electrophysiol. 2019;30:2858-2863.
2. So CY, Wang DD, Kang G, Villablanca PA, Frisoli T, O'Neill WW. Vacuuming the LAA:Left Atrial Appendage Thrombectomy Using AngioVac to Facilitate Percutaneous Mitral Balloon Valvuloplasty. Structural Heart. 2020;4:243-244.
3. Cruz-González I, González-Ferreiro R, Freixa X, et al. Cierre de la orejuela izquierda por ictus pese a la anticoagulación oral (ictus resistente):resultados del registro Amplatzer Cardiac Plug. Rev Esp Cardiol. 2020;73:28-34.
4. Cruz-González I, Trejo-Velasco B, González-Ferreiro R. Utilidad del dynamic road-mapping en el cierre de la orejuela izquierda. Rev Esp Cardiol. 2020;73:255.