To the Editor,
Coronary computed tomography angiography (CCTA) is one of the main imaging modalities used to discard coronary artery disease in patients with stable symptoms; thanks to its excellent negative predictive value, it can characterize atheromatous plaques and the degree of stenosis they cause.1 In some imaging facilities, the CCTA is used after measuring the coronary calcium score often through the Agatston score that does not require initially the injection of contrast. Studies suggest that patients with stable symptoms and lack of coronary calcium (CCS = 0 or Agatston = 0) don’t usually have significant coronary stenoses but a have better prognosis. This is indicative that a CCTA with the corresponding injection of contrast would not provide relevant information in most of the cases.2-4 Therefore, our objectives were to describe the prevalence and characteristic of patients with CCS = 0; also, to assess the findings obtained in the subsequent contrast study and invasive coronary angiography if any; finally, we studied the events occurring at the long-term follow-up in this group of patients.
Therefore, we conducted an observational cohort study that included all procedures (CCS and subsequent CCTA) performed in a tertiary center between 2008 and 2016. The authors declare that they acted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all patients. All patients were referred with chest pain and a past medical history of ischemic heart disease. The Philips CT Brillance 64-multislice detector computed tomography scanner and Heartbeat-CS software (Philips Medical Systems, United States) were used. The CCS was assessed using the Agatston score. Stenoses that were > 70% quantitatively were considered significant coronary lesions.
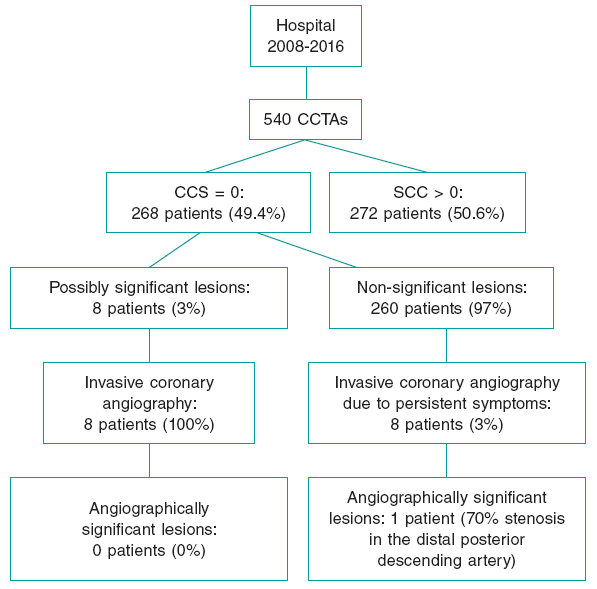
Five hundred and forty studies were conducted of which 268 showed Agatston scores = 0 (49.4%) (figure 1). Patients were mostly women (62.7% vs 50.4%), younger (55.1 years vs 64.9 years), and with a lower prevalence of cardiovascular risk factors (table 1). No differences were seen in the intraprocedural characteristics.
Figure 1. Flowchart of patients included in the study. CCTA, coronary computed tomography angiography; CCS: coronary calcium score.
Table 1. Clinical, intraprocedural, and follow-up characteristics
| Total | Agatston = 0 | Agatston > 0 | P | |
|---|---|---|---|---|
| (N = 540) | (N = 268) | (N = 272) | ||
| Clinical characteristics | ||||
| Women | 305 (56.5) | 168 (62.7) | 137 (50.4) | .004 |
| Age (years) | 59.98 ± 11.16 | 55.07 ± 11.28 | 64.86 ± 8.67 | < .001 |
| Arterial hypertension | 248 (46.1) | 90 (33.7) | 158 (58.3) | < .001 |
| Type 2 diabetes mellitus | 91 (16.9) | 25 (9.3) | 66 (24.3) | < .001 |
| Dyslipidemia | 143 (26.5) | 60 (22.4) | 83 (30.5) | .032 |
| Smoking | 78 (14.4) | 41 (15.3) | 37 (13.6) | .136 |
| Previous treatment | ||||
| Hypolipemiant drugs | 85 (15.8) | 31 (11.7) | 54 (19.9) | .009 |
| Antihypertensive drugs | 114 (21.1) | 42 (15.7) | 72 (26.5) | .002 |
| Antiplatelet therapy | 124 (23) | 54 (20.1) | 70 (25.7) | .123 |
| Analytical values | ||||
| Creatinine (mg/dL) | 0.87 ± 0.3 | 0.83 ± 0.31 | 0.9 ± 0.29 | .009 |
| Glycemia (mg/dL) | 104.49 ± 33.76 | 98.01 ± 31.57 | 110.36 ± 34.81 | < .001 |
| Total cholesterol levels (mg/dL) | 197.44 ± 44.24 | 202.41 ± 39.48 | 192.93 ± 47.95 | .020 |
| LDL-C (mg/dL) | 118.16 ± 37.26 | 122.69 ± 32.61 | 114.27 ± 40.72 | .014 |
| HDL-C (mg/dL) | 51.64 ± 14.7 | 53.14 ± 14.06 | 50.32 ± 15.11 | .039 |
| Triglycerides (mg/dL) | 146.08 ± 80.57 | 142.03 ± 84.91 | 148.73 ± 75.79 | .373 |
| Intraprocedural characteristics | ||||
| Step and shoot | 419 (77.6) | 213 (79.5) | 206 (75.7) | .297 |
| Atrial fibrillation | 9 (1.7) | 3 (1.1) | 6 (2.2) | .324 |
| Heart rate (bpm) | 60.59 ± 8.39 | 60.79 ± 7.97 | 60.49 ± 8.77 | .689 |
| Systolic arterial pressure (mmHg) | 126.52 ± 19.41 | 124.63 ± 18.88 | 128.49 ± 19.86 | .051 |
| Diastolic arterial pressure (mmHg) | 68.86 ± 11.73 | 69.38 ± 1.5 | 68.39 ± 12.04 | .410 |
| Allergic reaction | 5 (0.9) | 3 (1.1) | 2 (0.7) | .644 |
| Clinical follow-up | ||||
| N (%) | 510 (94.7) | 252 (94.03) | 258 (94.9) | |
| Follow-up period (months) | 34.79 ± 24.39 | 32.72 ± 25.08 | 36.72 ± 23.52 | .062 |
| Mortality | ||||
| Cardiovascular causes | 0 (0) | 0 (0) | 0 (0) | NS |
| Non-cardiac causes | 1 (0.2) | 1 (0.4) | 0 (0) | NS |
| Cardiovascular events | ||||
| Acute myocardial infarction | 2 (0.4) | 0 (0) | 2 (0.8) | .161 |
| Heart failure | 2 (0.4) | 0 (0) | 2 (0.8) | .161 |
| Ischemic stroke | 7 (1.4) | 3 (1.2) | 4 (1.6) | .914 |
| Total | 11 (2.2) | 3 (1.2) | 8 (3.1) | .138 |
|
bpm, beats per minute; HDL-C, high-density lipoprotein bound cholesterol; LDL-C, low-density lipoprotein bound cholesterol; NS, non-significant. Data are expressed as no. (%) or mean ± standard deviation. |
||||
Among the patients with zero CCS, only 8 patients showed images suggestive of significant lesions (3%) on the subsequent study with contrast (CCTA). Afterwards, the invasive coronary angiography performed in these cases confirmed the lack of significant lesions in all of the patients. Another 8 patients without significant lesions on the CCTA underwent an invasive coronary angiography because of their persistent symptoms, yet only 1 patient had significant stenosis: a male patient with a coronary anomaly consisting of a left anterior descending coronary artery originated at the right coronary artery with a 70% stenosis in the distal posterior interventricular branch that could not be revascularized. At the median 35-month follow-up [12 months to 56 months], no significant differences were seen regarding the events occurred between patients with CCS = 0 and those with CCS ≥ 1.
Therefore, patients with CCS = 0, almost half of those referred, had no significant lesions on the CCTA or the invasive coronary angiography. This is consistent with former studies like the one conducted by Hulten et al.,2 that reported a prevalence of potentially obstructive lesions of 1.5% in patients with CCS = 0 or Mittal et al.’s study,3 where 52.2% of the 2730 patients studied had zero CCS and significant lesions were only seen on the CCTA and the subsequent invasive coronary angiography in 4 (0.3%). Regarding prognosis, this study also showed a higher survival rate in the group with zero CCS (99% vs 94.5%).3
Similarly, the CONFIRM study confirmed an event-free survival rate of 99% within the first 2 years.4 Such a good survival rate was confirmed in our study, although without statistically significant differences regarding patients with calcium. This was probably due to the lower number of patients and the low percentage of events of both groups, maybe due to the inclusion of patients at lower risk.
The direct implication of these findings is that patients with zero CCS > may not have to undergo CCTA with the corresponding cost and time savings while avoiding venous puncture, the injection of iodinated contrast, the administration of bradycardia inducing drugs, and the use of more ionizing radiation. However, the main limitation for this is the possibility that the cause for the symptoms is a ruptured plaque where the presence of calcium is not indispensable.5 However, cumulative experience on this regard confirms that its finding in stable patients with low pre-test probabilities is highly unlikely.
Therefore, in our own opinion, the techniques should be adapted to the characteristics of each particular study patient. On the one hand, in patients at higher risk, the CCTA could be suggested right from the start given the currently relatively low doses of radiation; on the other hand, in low-risk patients (low pre-test probabilities with stable symptoms) a CCS with an Agatston score = 0 may spare the CCTA, thus reducing radiation and avoiding the injection of contrast.
FUNDING
There was no funding for this research project.
AUTHORS' CONTRIBUTIONS
V. M. Becerra-Muñoz, data collection, statistical analysis and manuscript drafting;;M. Millán-Gómez and G. Berteli-García, data collection and manuscript drafting; J. Algarra-García and N. Alegre-Bayo, reading of computerized tomography studies and revision of the final draft; M, Jiménez-Navarro, data collection, reading of computerized tomography studies and revision of the final draft.
CONFLICTS OF INTEREST
The authors declare that there are no conflicts of interest with respect to this study.
REFERENCES
1. Montalescot G, Sechtem U, Achenbach S, et al. 2013 ESC guidelines on the management of stable coronary artery disease. Eur Heart J. 2013;34:2949-3003.
2. Hulten E, Bittencourt MS, Ghoshhajra B, et al. Incremental prognostic value of coronary artery calcium score versus CT angiography among symptomatic patients without known coronary artery disease. Atherosclerosis. 2014;233:190-195.
3. Mittal TK, Pottle A, Nicol E, et al. Prevalence of obstructive coronary artery disease and prognosis in patients with stable symptoms and a zero-coronary calcium score. EHJ Cardiovasc Imaging. 2017;18:922-929.
4. Villines T, Hulten E, Shaw L, et al. Prevalence and severity of coronary artery disease and adverse events among symptomatic patients with coronary artery calcification scores of zero undergoing coronary computed tomography angiography:results from the CONFIRM registry. J Am Coll Cardiol. 2011;58:2533-2540.
5. Gottlieb I, Miller J, Arbab-Zadeh A, et al. The absence of coronary calcification does not exclude obstructive coronary artery disease or the need for revascularization in patients referred for conventional coronary angiography. J Am Coll Cardiol. 2010;55:627-634.