To the Editor,
The outbreak of the COVID-19 pandemic had enormous repercussions for the management of ST-segment elevation myocardial infarction (STEMI) worldwide.1,2 Overall, the number of patients treated with primary angioplasty in Spain dropped while ischemia time increased from symptom onset until reperfusion.3 The early phase of the pandemic gave rise to a period of consecutive outbreaks during which the management of STEMI seems to have improved thanks to a less saturated healthcare system and the implementation of proper healthcare protocols.4 However, data on the possible side effects associated with the functioning of the healthcare systems in the STEMI Care Network after the first phase of the pandemic are scarce. In the Madrid area, our hospital is one of the highest-volume centers regarding primary angioplasty as it takes over nearly 20% of all activations in the region.5 We present our experience with the STEMI Care Network in the months that followed the de-escalation of June 2020 when the early phase of the COVID-19 pandemic ended in Spain.
Our center STEMI Care Network activation times were analyzed during the first phase of the pandemic (March 14 through June 21, 2020), as well as in the previous and following 12 months. Also, consistent with the data published to this date,3 during the early phase of the pandemic, ischemia time increased in patients from our series. It fluctuated during the following months, with median ischemia times during the second and third waves similar to those reached during the first wave (figure 1). During 2021, equivalent to 2020 when the early phase of the pandemic occurred, the fourth wave of the pandemic broke out. The intensity of this wave was lower compared to the previous ones, and although the median ischemia time was closer to the one described before the pandemic, the number of patients with prolonged ischemia time remained higher than usual (figure 2).
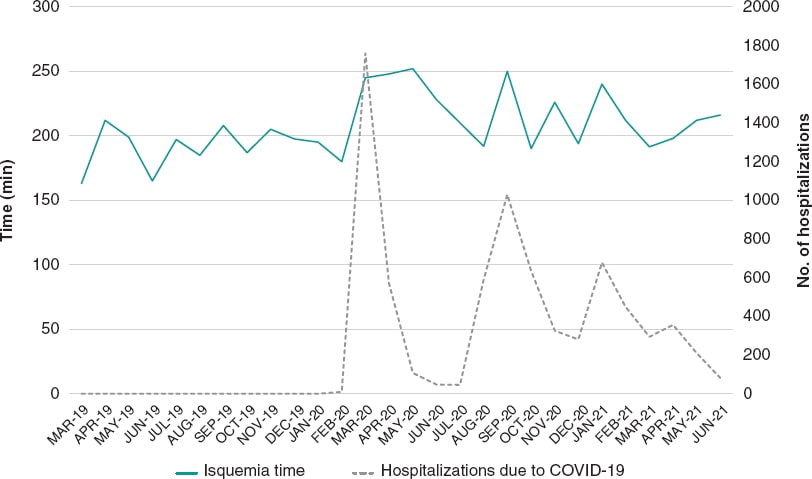
Figure 1. Median ischemia time of patients referred for primary angioplasty, and number of patients hospitalized in our center with COVID-19.
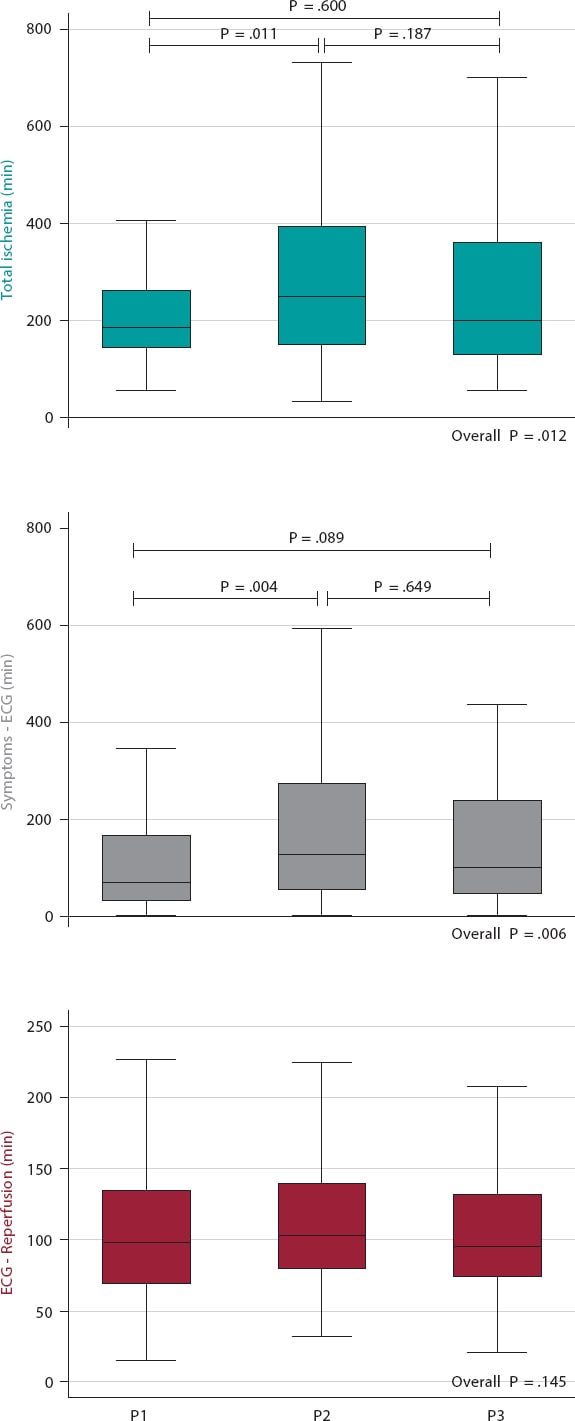
Figure 2. Times during the early phase of the pandemic and within the same period of 2019 and 2021. P1, March/14/2019 through June/21/2019; P2, March/14/2020 through June/21/2020; P3, March/14/2021 through June/21/2021; number of STEMI Care Network activations in each period: 111, 144, and 140 respectively. Bonferroni correction for multiple comparisons. ECG, electrocardiogram.
Table 1 shows a comparison of the STEMI Care Network activation times during the 12 previous and following months compared to the first phase of the pandemic. The percentage of patients with late onsets (ischemia time >12 hours) was significantly higher during the months that followed the first phase and almost double compared to the time before the pandemic (9.2% vs 4.3%; P = .004). When times were analyzed based on the patients’ clinical presentation it was found that, during the period that followed the pandemic early phase, ischemia time was higher than usual in the group of patients who went directly to the health center (including PCI- and non-PCI-capable centers, and primary care centers). In these patients the median ischemia time after the first wave was 36 minutes longer compared to pre-pandemic time (252 [165-412] vs 216 [150-336] minutes; P = .011) basically at the expense of prolonged time from symptom onset until diagnosis. However, it is surprising to see that ischemia time did no go up in patients assisted by the medical emergency services. On the other hand, after the start of the pandemic we saw a change in the pattern of clinical presentation with fewer patients going directly to the health center. This lower percentage of patients who went directly to the health center and the persistently prolonged ischemia time reported in this group of patients due to late diagnosis can be indicative that, at least, part of the population is still afraid that they will get coronavirus at the hospital.
Table 1. Times and clinical presentation of patients from the STEMI Care Network during the previous and following 12 months with respect to the first phase of the pandemic
| Previous period (03/14/2019 through 03/13/2020) | Later period (06/22/2020 through 06/21/2021) | P | |
|---|---|---|---|
| N | 438 | 434 | |
| Age, years | 64.1 ± 14.2 | 63.9 ± 13.9 | .982 |
| Sex (male) | 317 (72.4) | 319 (73.5) | .708 |
| Clinical presentation | |||
| Healthcare lefts | 296 (67.6) | 251 (57.8) | .003 |
| Emergency medical services | 142 (32.4) | 183 (42.2) | |
| Overall times | |||
| Total ischemia, min | 191 [135-280] | 207 [135-353] | .048 |
| Symptoms – ECG, min | 80 [37-163] | 100 [50-244] | .001 |
| ECG – reperfusion, min | 96 [71-134] | 92 [72-127] | .402 |
| Infarctions with ischemia times > 12 hours | 19 (4.3) | 40 (9.2) | .004 |
| Times based on the clinical presentation | |||
| Health lefts | 296 | 251 | |
| Total ischemia, min | 216 [150-336] | 252 [165-412] | .011 |
| Symptoms – ECG, min | 95 [42-185] | 124 [63-290] | < .001 |
| ECG – reperfusion, min | 106 [80-155] | 106 [79-154] | .840 |
| Emergency medical services | 142 | 183 | |
| Total ischemia, min | 154 [121-205] | 155 [120-240] | .230 |
| Symptoms – ECG, min | 65 [31-11] | 70 [45-157] | .024 |
| ECG – reperfusion, min | 75 [64-100] | 79 [65-97] | .926 |
ECG, electrocardiogram. Data are expressed as no. (%) or mean ± standard deviation or median [interquartile range]. | |||
Our analysis suggests that, once the early phase of the pandemic was over, the percentage of patients with an evolving STEMI referred for primary angioplasty remained high. Also, that the STEMI Care Network activation times never went back to normal in patients who went directly to the health center. Therefore, it seems essential to raise awareness among the population of the importance of seeking medical attention at the first sign of chest pain, check the action protocols available in the ERs of health centers, and try to prioritize the care of these patients to return to similar ischemia times to the pre-COVID-19 era.
FUNDING
None whatsoever.
AUTHORS’ CONTRIBUTIONS
All authors participated in the design, draft, and process of critical revision of the final manuscript.
CONFLICT OF INTERESTS
None reported.
REFERENCES
1. Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-Segment Elevation Cardiac Catheterization Laboratory Activations in the United States During COVID-19 Pandemic. J Am Coll Cardiol. 2020;75:2871-2872.
2. Zhang L, Fan Y, Lu Z. Experiences and lesson strategies for cardiology from the COVID-19 outbreak in Wuhan, China, by 'on the scene'cardiologists. Eur Heart J. 2020;41:1788-1790.
3. Rodríguez-Leor O, Cid-Álvarez B, Pérez de Prado A, et al. Impact of COVID-19 on ST-segment elevation myocardial infarction care. The Spanish experience. Rev Esp Cardiol. 2020;73:994-1002.
4. Romaguera R, Cruz-Gonzalez I, Ojeda S, et al. Consensus document of the Interventional Cardiology and Heart Rhythm Associations of the Spanish Society of Cardiology on the management of invasive cardiac procedure rooms during the COVID-19 coronavirus outbreak. REC Interv Cardiol.2020;2:112-117.
5. Código Infarto. Consejería de Sanidad Madrid. 2017. Available online:https://www.comunidad.madrid/servicios/salud/codigo-infarto. Accessed 10 Jan 2021.
* Corresponding author: Servicio de Cardiología, Hospital Universitario 12 de Octubre, Av. de Córdoba, s/n, 28041 Madrid, Spain
E-mail address: igomezblazquez@gmail.com (I. Gómez-Blázquez).












