To the Editor,
Myocardial infarction is the leading cause of morbidity and mortality in our setting. Percutaneous coronary intervention has improved the prognosis of patients with ST-segment elevation myocardial infarction (STEMI).1 However, there is a subgroup of patients who suffer from suboptimal myocardial reperfusion with appearance of myocardial fibrosis, ventricular dysfunction, and development of heart failure.2
Recently, several pharmaceutical and procedural strategies have been developed to improve these results.3 The PiCSO system (Pressure-controlled intermittent coronary sinus occlusion) developed by Miracor Medical SA, Belgium consists of a balloon catheter to occlude the coronary sinus periodically:
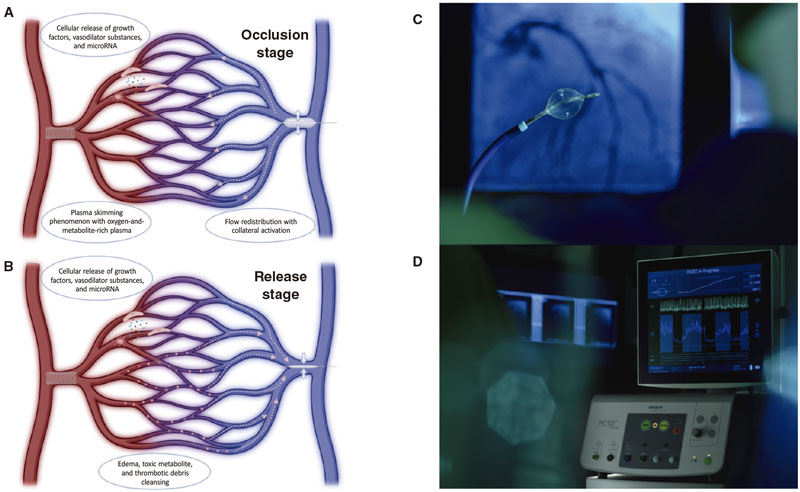
- 1) During the occlusion stage (5 to 15 s), venous flow is redistributed from well perfused areas towards ischemic regions through the formation of collateral circulation. Also, through an increased venous systolic pressure, the plasma skimming phenomenon allows better perfusion of venules with oxygen-and-metabolite-rich plasma.
- 2) During the release stage (3 to 4 s) the dramatic drop of venous pressure creates a gradient that ends up clearing all thrombotic debris, toxic metabolites, and myocardial edema.
- 3) These pressure variations can induce mechanotransduction by activating vascular cells and releasing growth factors, vasodilator substances, and microRNA into microcirculation (figure 1).
Figure 1. Representation of the mechanism of action of the PiCSO system in the occlusion (A) and release stages (B). The PiCSO system includes a balloon catheter (C) connected to a console (D) to automatically occlude the coronary sinus intermittently.
The PiCSO system has proven capable of improving microvascular function and reducing the infarction size in non-randomized clinical trials of patients with high-risk anterior STEMI.4 As a matter of fact, it was granted the CE marking in 2020 with a clinical indication for the management of anterior STEMI with < 12-hour evolution and early TIMI grade 0-1 flow (Thrombolysis in Myocardial Infarction) and culprit lesion in the proximal or middle segments of the left anterior descending coronary artery. We wish to use this scientific letter to share our experience with this novel device in 2 case reports. The patients’ informed consent was obtained, and the study was approved by the ethics committee according to the principles set forth in the Declaration of Helsinki.
The first case is a 83-year-old man without a past medical history of interest with thoracic pain and anterior ST-segment elevation of 3 mm in V1-V4 on the electrocardiogram. The coronary angiography revealed the presence of an acute thrombotic occlusion in the proximal segment of the left anterior descending coronary artery with early TIMI grade-0 flow (figure 2A). Thrombus aspiration and drug-eluting stent implantation led to TIMI grade-3 flow after 115 min of total ischemia (figure 2B). Since this was a large anterior STEMI with early TIMI grade-0 flow, right femoral venous access, cannulation (figure 2C), and PiCSO balloon catheter implantation in the coronary sinus were used (figure 2D) with a 21 min therapy time, and PiCSO doses of 824 mmHg (values > 800 mmHg are advised since they are associated with a reduced infarction size in former studies)4 (figure 2E). The first electrocardiogram revealed a left ventricular ejection fraction (LVEF) of 30% with peak troponin levels of 197 419 ng/L. The patient was discharged without any signs of angina or heart failure and a LVEF of 35% to 40% at 7 days.
Figure 2. Coronary angiography showing an acute thrombotic occlusion in the proximal left anterior descending coronary artery (A). Coronary flow recovery after thrombus aspiration and stenting (B). Afterwards, via right femoral vein (12-Fr), a 8.5-Fr Destino Reach introducer sheath (Oscor, United States) was used for cannulation (C) and the PiCSO balloon catheter was implanted in the coronary sinus (D). The console (E) shows charts with information on coronary sinus pressures and an algorithm to estimate the dose of PiCSO in mmHg—which is a reference of the performance of PiCSO—based on inflation time, the coronary sinus maximum pressure in systole and diastole, and the mean pressure during the release stage.
The second case was a 67-year-old man, active smoker, who had sustained a cardiac arrest due to ventricular fibrillation with recovered circulation 25 min after starting cardiopulmonary resuscitation. The electrocardiogram confirmed the presence of anterior ST-segment elevation of 20 mm in V1-V4, and the coronary angiography the presence of acute thrombotic occlusion in the middle segment of the left anterior descending coronary artery (TIMI grade-0 flow). Thrombus aspiration and drug-eluting stent implantation led to TIMI grade-3 flow (total ischemia time, 120 min). Since this was also a high-risk anterior STEMI, it was decided to implant the PiCSO system in the coronary sinus via right femoral vein with a 20 min therapy time and a PiCSO dose of 830 mmHg. The first electrocardiogram showed a LVEF of 35% and peak troponin levels of 63 141 ng/L. The patient neurological and cardiologic progression was good. The patient’s LVEF was 55% 10 days after the infarction.
The PiCSO system is a safe and easy to implement tool in the management of STEMI. However, PiCSO will have to demonstrate its efficacy in ongoing randomized trials.
FUNDING
None whatsoever.
AUTHORS’ CONTRIBUTIONS
S. Brugaletta, and P. Vidal-Calés participated in the manuscript idea, design, and data analysis. O Abdul-Jawad Altisent, F. Spione, V. Arévalos, and M.Sabaté reviewed and edited the manuscript.
CONFLICTS OF INTEREST
None reported.
ACKNOWLEDGEMENTS
Dr. Pablo Vidal Calés received a research grant at the end of his residency at Hospital Clínic de Barcelona.
REFERENCES
1. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119-177.
2. Stone GW, Selker HP, Thiele H, et al. Relationship Between Infarct Size and Outcomes Following Primary PCI: Patient-Level Analysis From 10 Randomized Trials. J Am Coll Cardiol. 2016;67:1674-1683.
3. Vidal-Calés P, Cepas-Guillén PL, Brugaletta S, Sabaté M. New Interventional Therapies beyond stenting to Treat ST-Segment Elevation Acute Myocardial Infarction. J Cardiovascular Dev Dis. 2021;8:100.
4. De Maria GL, Alkhalil M, Borlotti A, et al. Index of microcirculatory resistance-guided therapy with pressure-controlled intermittent coronary sinus occlusion improves coronary microvascular function and reduces infarct size in patients with ST-elevation myocardial infarction: the Oxford Acute Myocardial Infarction - Pressure-controlled Intermittent Coronary Sinus Occlusion study (OxAMI-PICSO study). EuroIntervention. 2018;14:e352-e359.