To the Editor,
Revascularization of a coronary chronic total occlusion (CTO) is indicated in patients with refractory angina, after treatment of non-CTO lesion.1 Observational studies have suggested that when intermediate stenosis is present in an artery providing collaterals to a CTO (“donor artery”), its fractional flow reserve (FFR) value increases after percutaneous coronary intervention (PCI) of the CTO.2 Quantitative flow ratio (QFR) has demonstrated excellent correlation with FFR in several settings.3,4 The purpose of this study was to determine the ability of QFR to predict the severity of intermediate lesions in donor arteries as compared to its value after CTO-PCI and, also, as compared to FFR.
A retrospective analysis of a prospective registry was performed. Patients who underwent successful CTO-PCI and had a concomitant intermediate stenosis (between 30% to 70% on visual estimation) in the donor artery were included. FFR measurements, obtained according to standard protocol before starting and after completing CTO-PCI, were available for all participants, and the index of microcirculatory resistance (IMR) was available in 72.7% of the patients. Intracoronary adenosine was used to induce hyperemia. QFR was calculated retrospectively based on angiographic acquisitions before and after CTO-PCI and was feasible in all cases. To ensure reproducible results, QFR measures were performed starting within the sensor of the pressure wire. QFR computation was performed by a blinded technician using the QAngio XA 3D/QFR (Medis Medical Imaging Systems, the Netherlands). FFR and QFR < 0.80 were considered positive. Patients whose intermediate lesions in donor artery were ostial or presented any contraindication for adenosine administration were excluded from the study. One-month and one-year clinical follow-up were available for all patients. Categorical variables were presented as counts and percentages, while continuous variables were expressed as mean ± standard deviation. The agreement and correlation between QFR and FFR were evaluated using the Bland-Altman plot, Lin’s concordance correlation coefficient (CCC) and Pearson’s test. The Shapiro-Wilk was used to ensure the normal distribution of data. All analyses were conducted using the statistical software R, version 4.2.0 (R Project for statistical computing).
A total of 33 patients were analyzed. Baseline patient and procedural characteristics are presented in table 1. The most common CTO location was the right coronary artery (RCA), 60.6%, followed by the left anterior descending coronary artery (LAD), 30.3%, and the circumflex (Cx) 9.1%. Conversely, LAD was the most common donor artery (69.7%), followed by RCA (30.3%). The mean donor vessel’s pre-procedural FFR was 0.773 ± 0.059 with 75.8% of the patients showing a positive FFR, and the baseline QFR was 0.813±0.446 (36.4% positive). Post-CTO-PCI, FFR increased to 0.844 ± 0.049 (12.1% positive) and QFR to 0.825 ± 0.044 (27.3% positive). The mean change of post-PCI FFR was + 0.067 (LAD occlusion), + 0.073 (Cx) and + 0.08 (RCA). Figure 1 summarizes the main results of the study. Moderate agreement was observed between pre-CTO-PCI FFR and QFR measurements (CCC: 0.65; 95% confidence interval [95%CI], 0.48-0.77). A stronger agreement emerged between pre-CTO-PCI QFR and post-CTO-PCI FFR (CCC: 0.76; 95%CI, 0.62-0.85), as well as between QFR values measured before and after PCI (CCC: 0.93; 95%CI, 0.87-0.96). However, the correlation between pre- and post-PCI FFR values was comparatively weaker (CCC: 0.44; 95%CI, 0.275-0.58). IMR demonstrated a significant improvement (from 43.1 ± 5.6 to 31.5 ± 8.2 mmHg/s, P < .001) as estimated immediately post CTO-PCI.
Table 1. Main characteristics of the atients included in the study
| Variable | N = 33 |
|---|---|
| Baseline characteristics | |
| Age, years | 69.3 ± 11.7 |
| Gender, male | 21 (63.6) |
| Hypertension | 26 (78.8) |
| Diabetes mellitus | 19 (57.6) |
| Dyslipidemia | 27 (81.8) |
| Smoking | 16 (48.5) |
| Prior myocardial infarction | 6 (18.2) |
| Prior percutaneous coronary intervention | 4 (12.1) |
| Prior coronary bypass grafting | 3 (9.1) |
| Left main disease | 0 (0) |
| Left anterior descending disease | 14 (42.4) |
| Circumflex disease | 11 (33.3) |
| Right coronary artery disease | 26 (78.8) |
| Location of chronic total occlusion | |
| Circumflex artery | 3 (9.1) |
| Left anterior descending artery | 10 (30.3) |
| Right coronary artery | 20 (60.6) |
| Location of donor artery | |
| Left anterior descending artery | 23 (69.7) |
| Right coronary artery | 10 (30.3) |
| Procedural characteristics | |
| Successful recanalization technique | |
| Antegrade dissection - reentry | 7 (21.2) |
| Antegrade wire escalation | 17 (51.5) |
| Retrograde wire escalation | 9 (27.3) |
| Fluoroscopy time (min) | 42.6 ± 16.7 |
| Contras dose (cc) | 322.9 ± 134.1 |
| Radiation dose (Gy) | 2.8 ± 1.1 |
| Successful recanalization of the chronic total occlusion | 33 (100) |
|
Data are expressed as mean ± standard deviation or absolut number (number and percentage). |
|
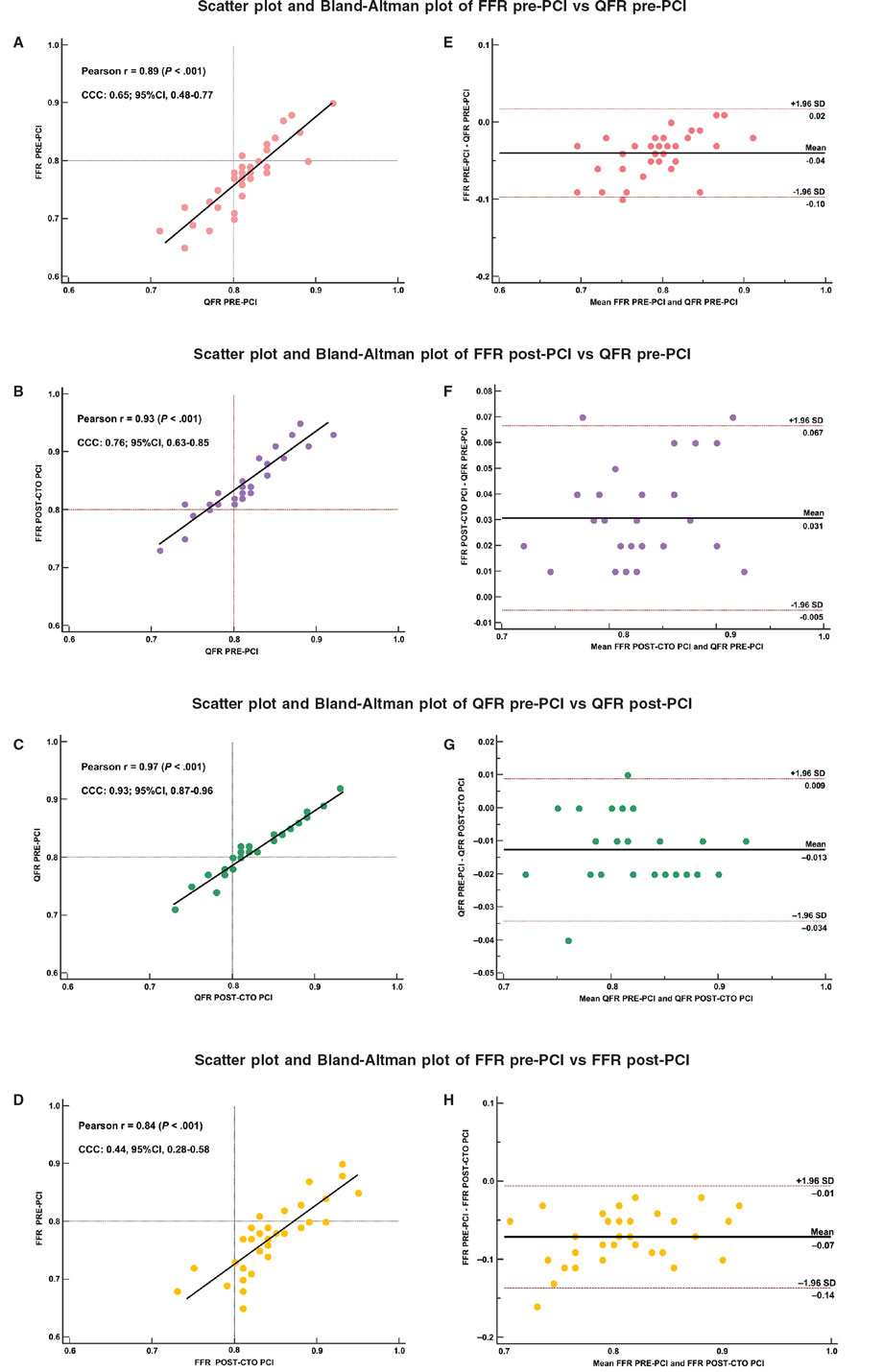
Figure 1. Correlation between QFR and FFR values in the donor artery of a CTO before and after a percutaneous coronary intervention of the CTO. Scatter (A,B,C,D) and Bland-Altman (E,F,G,H) plots showing the strong correlation between QFR estimated before CTO-PCI and FFR estimated after CTO-PCI demonstrating the potential of QFR as a predictive tool due to its independence from the revascularization. 95%CI, 95% confidence interval; CCC, concordance correlation coefficient; CTO, chronic total occlusion; FFR, fractional flow reserve; QFR, quantitative flow ratio; PCI, percutaneous coronary intervention; SD, standard deviation.
This post-angioplasty microvascular resistance assessed values are consistent with those previously described in the literature during the acute phase following revascularization, where slight variations are found.5
Our findings align with previous observations showing an increase in FFR within the donor artery. This might result from the donor artery’s decreased absolute total perfused coronary territory flow and microvascular resistance after normal flow is restored.2 The minimal variation in QFR values pre- and post-PCI could be attributed to the software’s processing of angiography images and coronary territories, which may not fully consider the physiology of microvasculature and the actual total territory perfused by the donor artery. These limitations may diminish the role of QFR in assessing donor arteries intermediate lesions as compared to FFR and therefore require further validation.
Despite the limitations of the study due to its retrospective nature and the small sample, the hypothesis-generating findings suggest lower impact of microvascular index on QFR than on FFR assessment of donor arteries in patients with CTOs. Further prospective studies are required to confirm these findings.
FUNDING
None.
ETHICAL CONSIDERATIONS
The protocol was approved by the ethics committee and informed consent was obtained from the patients. SAGER recommendations were followed.
STATEMENT ON THE USE OF ARTIFICIAL INGELLIGENCE
Artifical intelligence was not used during this investigation.
AUTHORS’ CONTRIBUTIONS
I.J. Amat-Santos and L. Scorpiglione designed the manuscript. I.J. Amat-Santos, C. Cortés-Villar, A. Gutiérrez and A. Fernández Cisnal collected the data. L. Scorpiglione and J. Ruiz Ruiz analyzed the data and drafted the manuscript. All authors have read and approved the sending of this manuscript.
CONFLICTS OF INTEREST
None to declare.
REFERENCES
1. Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization. J Am Coll Cardiol. 2022;79:21–129.
2. Ladwiniec A, Cunnington MS, Rossington J, et al. Collateral Donor Artery Physiology and the Influence of a Chronic Total Occlusion on Fractional Flow Reserve. Circ Cardiovasc Interv. 2015;8:002219.
3. Cortés C, Carrasco-Moraleja M, Aparisi A, et al. Quantitative flow ratio-Meta-analysis and systematic review. Catheter Cardiovasc Interv. 2021;97:807-14.
4. Amat-Santos IJ, Marengo G, Sánchez-Luna JP, et al. Validation of Quantitative Flow Ratio-Derived Virtual Angioplasty with Post-Angioplasty Fractional Flow Reserve-The QIMERA-I Study. J Cardiovasc Dev Dis. 2023;11:14.
5. Keulards DCJ, Vlaar PJ, Wijnbergen I, Pijls NH, Teeuwen K. Coronary physiology before and after chronic total occlusion treatment:what does it | us?Neth Heart J. 2020;29:22-29.










