To the Editor,
In left atrial appendage closure (LAAC), venous access is often predictable. These are 2 cases of venous disease found during LAAC and the alternatives proposed for its resolution. Both patients gave their informed consent for publication purposes.
In case #1, an 88-year-old man who was a pacemaker carrier, with permanent atrial fibrillation, ventricular dysfunction, and non-surgical sacral fracture was referred for LAAC due to recurrent hemorrhages.
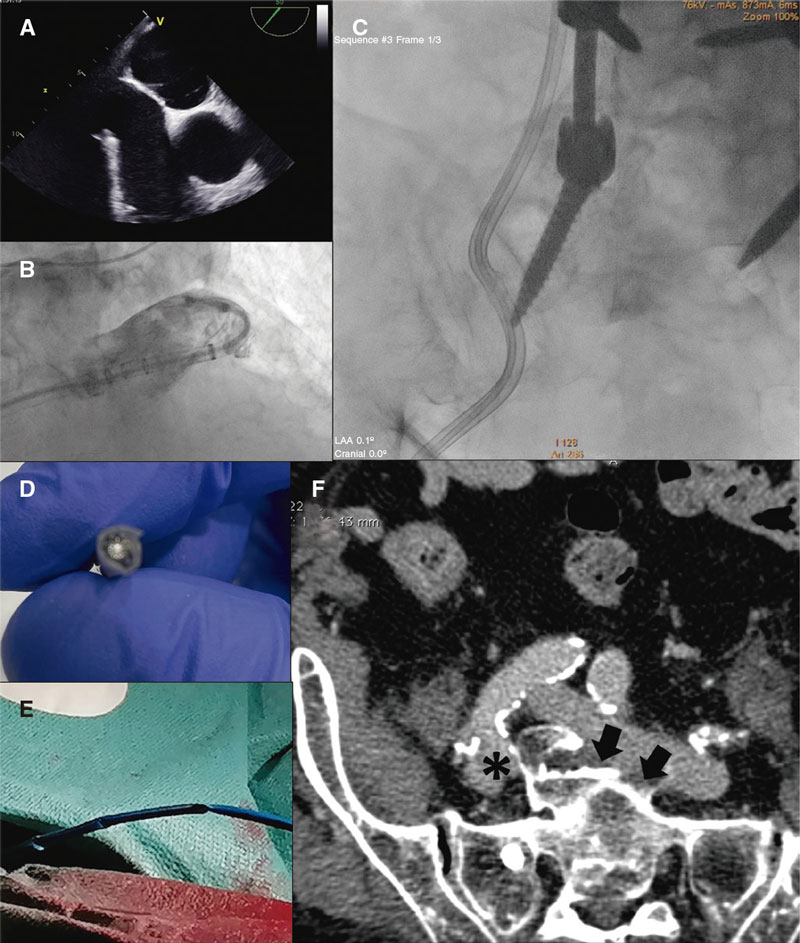
Through previous ultrasound-guided venous puncture a transseptal system was advanced that experienced significant resistance in the iliac curvature, difficult torsion at the right atrium, and loss of driving force in the fossa ovalis (figure 1, videos 1-4 of the supplementary data). Transseptal puncture was achieved through the rigid section of a 0.014 in angioplasty guidewire by exchanging the flexible section and advancing the sheath towards the pulmonary vein. Afterwards, it was exchanged for a 14-Fr sheath, and the pigtail catheter was mounted over the high-support guidewire. However, significant resistance during retraction and rotation maneuvers was reported. Nevertheless, it was successfully placed in the left atrial appendage and several angiographies were performed. During pigtail catheter withdrawal, resistance was very significant with evidence of severe torsion following the previous lumbosacral surgery. Since it was impossible to advance the device due to damage to the distal border or recanalize the sheath with a 0.035 in guidewire the procedure was stopped. Computed tomography (CT) scan revealed the presence of lateral deviation and elongation of the inferior vena cava bifurcation with endofibrosis at this level and loss of cleavage plane with the sacrum, posterior compression of the right common iliac vein, and horizontalization of the left common iliac vein. Conservative treatment was decided.
Figure 1. Limited contact pressure of transseptal system (A), and difficult maneuverability of the pigtail catheter (B) due to the severe torsion of the delivery catheter (C). Procedure stopped due to the impossibility of advancing a new device or guidewire (D, E). Computed tomography scan (F) of a compressed right iliac vein (asterisk) between the fracture and the homolateral common iliac artery. Presence of endofibrosis (arrows) and lack of cleavage plane between the left common iliac vein and the sacrum.
In case #2, a 74-year-old man with permanent atrial fibrillation, on hemodialysis, prostate cancer, and an old right pelvic fracture was referred for LAAC due to severe hemorrhages in arteriovenous fistula.
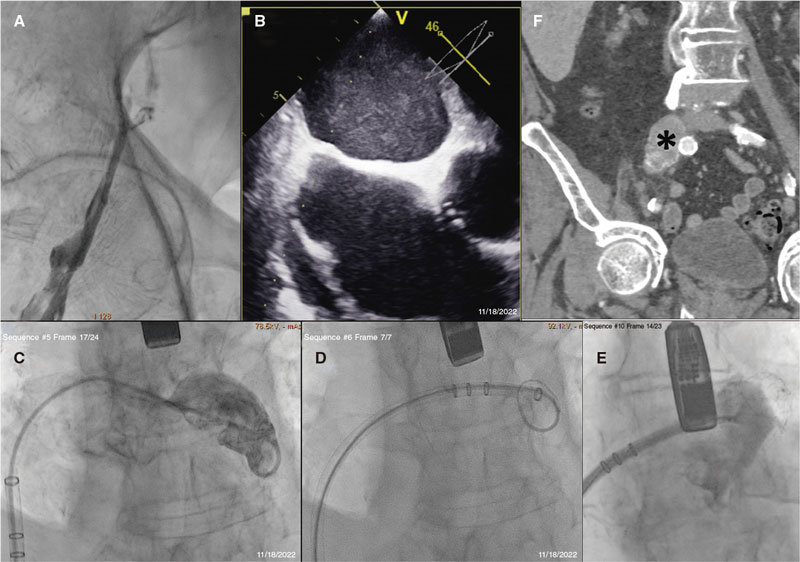
During ultrasound-guided venous puncture, a large caliber common femoral vein with flow inside was reported. Since the Teflon-coated guidewire could not be advanced antegradely, an angiography documented the presence of iliofemoral deep venous thrombosis (figure 2, videos 5-8 of the supplementary data). Procedure went on via left access using a BRK-1 XS needle (Abbott Vascular, United States) by pre-shaping a secondary curve of additional 15° to 20° while the guidewire was being manipulated and elevated to prevent needle deformation. Given the limited contact with the septum, the rigid section of an angioplasty guidewire was required to perform the puncture. A pigtail catheter, and a high-support guidewire were used to bring the 14-Fr sheath closer to the left atrial appendage. A 31 mm Watchman FLX device (Boston Scientific, United States) was successfully implanted The CT scan confirmed the presence of chronic deep venous thrombosis at right common iliac vein level.
Figure 2. Venography reveals the presence of a complete obstruction that triggered change to left access route (A). Note the unusual position and limited support of both the transseptal puncture needle (B) and the delivery catheter (C). The increased support provided by the rigid guidewire to the 6-Fr pigtail catheter facilitated sheath placement and device release (D, E). The CT scan (F) revealed the presence of an oversized right common iliac vein with hyperdensities inside.
Venous damage is one of the most dreaded complications of lumbosacral surgery. May-Turner syndrome of posterior location (iliac vein compression due to incorrect alignment following spinal instrumentation) has been described by analogy with the anterior location one due to right common iliac artery crossing.1 In addition, lower limb fractures can become complicated with deep venous thrombosis and eventually trigger chronification in a third of the cases.2 The growing prevalence of this plethora of clinical signs and symptoms requires knowing different alternatives to complete structural heart procedures (table 1).
Table 1. Technical resources to perform left atrial appendage closure in the presence of elongation, calcification, tortuosity or venous obstruction
| Stage of the procedure | Maneuver proposed |
|---|---|
| Suspected venous disease | Past medical history of trauma/vertebral or pelvic surgery or venous thromboembolic disease |
| Ultrasound-guided access (hypoplasia, increased caliber due to venous hypertension, collateral circulation) | |
| Computed tomography scan (venous stage) and specialized assessment | |
| Correction of tortuosity, and increased passive support | Work on a larger caliber introducer sheath like the ones used for transcatheter valve implantation (anticipate risk of venous lesion and possibilities of transcatheter repair) |
| Transseptal puncture | Pre-shaping of the needle additional curve |
| Needle with additional sharpening (XS series) | |
| Sequential use of the rigid and flexible parts of the angioplasty guidewire | |
| SafeSept system | |
| Radiofrequency or electrocautery needle | |
| System crossing through the septum | Greater support guidewires |
| Septal dilatation with balloon or dilators like the ones used for transcatheter mitral valvuloplasty | |
| Navigation through left atrium and placement into the left atrial appendage | Use of flexible, deflectable or pre-shapable sheaths |
| Additional support with a catheter of a larger caliber (≥ 6-Fr), and a high-support guidewire inside | |
| Impossibility of lower access route | Upper limb access with deflectable sheath |
| Epicardial closure (eg, stapling or clips) | |
| Anticoagulation at lower doses compared to the standard ones |
In case #1, the CT scan revealed the presence of an inelastic right axis, high risk of venous fracture, and extreme elongation and horizontalization of the left axis to an extent that all lower limb procedures were ill-advised. Although procedures have been performed via upper3 or transhepatic access,4 experience on this regard is very limited. Case #2 illustrates the possibility of left access in patients without extreme elongation or iliofemoral axis horizontalization. As a last resort, epicardial approaches can be used. However, operators should be aware of the need for an associated transseptal access (hybrid procedures) or thoracotomy.
FUNDING
None whatsoever.
AUTHORS’ CONTRIBUTIONS
All the authors participated in the management of the patients, collection of clinical information, drafting, and critical review of the manuscript.
CONFLICTS OF INTEREST
D. Martí Sánchez received consultancy and training fees from Boston Scientific Ibérica. The remaining authors declared no conflicts of interest whatsoever.
SUPPLEMENTARY DATA
Vídeo 1. Martí Sánchez D. DOI: 10.24875/RECICE.M23000364
Vídeo 2. Martí Sánchez D. DOI: 10.24875/RECICE.M23000364
Vídeo 3. Martí Sánchez D. DOI: 10.24875/RECICE.M23000364
Vídeo 4. Martí Sánchez D. DOI: 10.24875/RECICE.M23000364
Vídeo 5. Martí Sánchez D. DOI: 10.24875/RECICE.M23000364
Vídeo 6. Martí Sánchez D. DOI: 10.24875/RECICE.M23000364
Vídeo 7. Martí Sánchez D. DOI: 10.24875/RECICE.M23000364
Vídeo 8. Martí Sánchez D. DOI: 10.24875/RECICE.M23000364
BIBLIOGRAFÍA
1. Woo EJ, Ogilvie RA, Krueger VS, Lundin M, Williams DM. Iliac vein compression syndrome from anterior perforation of a pedicle screw. J Surg Case Rep. 2016;2016:rjw003.
2. Cannon KA, Badiee J, Wallace JD, et al. The prevalence of chronic deep venous thrombosis in trauma: Implications for hospitals and patients. J Trauma Acute Care Surg. 2018;84:170-174.
3. Galea R, Roten L, Siontis GCM, Brugger N, Windecker S, Räber L. Percutaneous left atrial appendage closure with superior vascular access. EuroIntervention. 2022;18:e695-e696.
4. Zare P, Rechani L, Smithson S. Left atrial appendage closure device implantation via transhepatic vascular access: a case report. Eur Heart J Case Rep. 2020;4:1-5.