This is the case of a 62-year-old man who presented to the emergency department with signs of an acute neurological syndrome. He remained under regular monitorization due to spastic paraparesis. The patient’s past medical history also included dyslipidemia, active smoking, former alcohol abuse, and psoriasis. His routine medication included daily aspirin 150 mg, and simvastatin 20 mg. Due to severe worsening of his neurological status, he was admitted for further evaluation. After careful clinical evaluation, diagnosis of cerebellar and pyramidal syndrome in the neurosyphilis setting was achieved. Penicillin was started. During hospitalization, cerebral magnetic resonance imaging revealed the presence of a massive hernia at C4-C5 causing significant spinal cord compression. Decompressive surgery was advised. During hospitalization, he complained of chest pain. The ECG showed signs of sinus rhythm with sustained diffuse ST-segment depression and ST-segment elevation in aVR and V1. The transthoracic echocardiography showed a severely impaired left ventricular ejection fraction with severe hypokinesia of the apex, anterior, posterior, and lateral walls. The aortic root was mildly enlarged, but no flaps were seen. Due to refractory chest pain and progressively worsening hypotension, the patient was given unfractionated heparin (5000 IU) and underwent an emergency coronary angiography that revealed the presence of critical left main coronary artery ostial stenosis (videos 1 and 2 of the supplementary data). No further lesions were identified. Due to the complexity of the lesion, percutaneous angioplasty under left ventricular assist device was advised. It was necessary to make a multidisciplinary decision due to the patient’s condition.
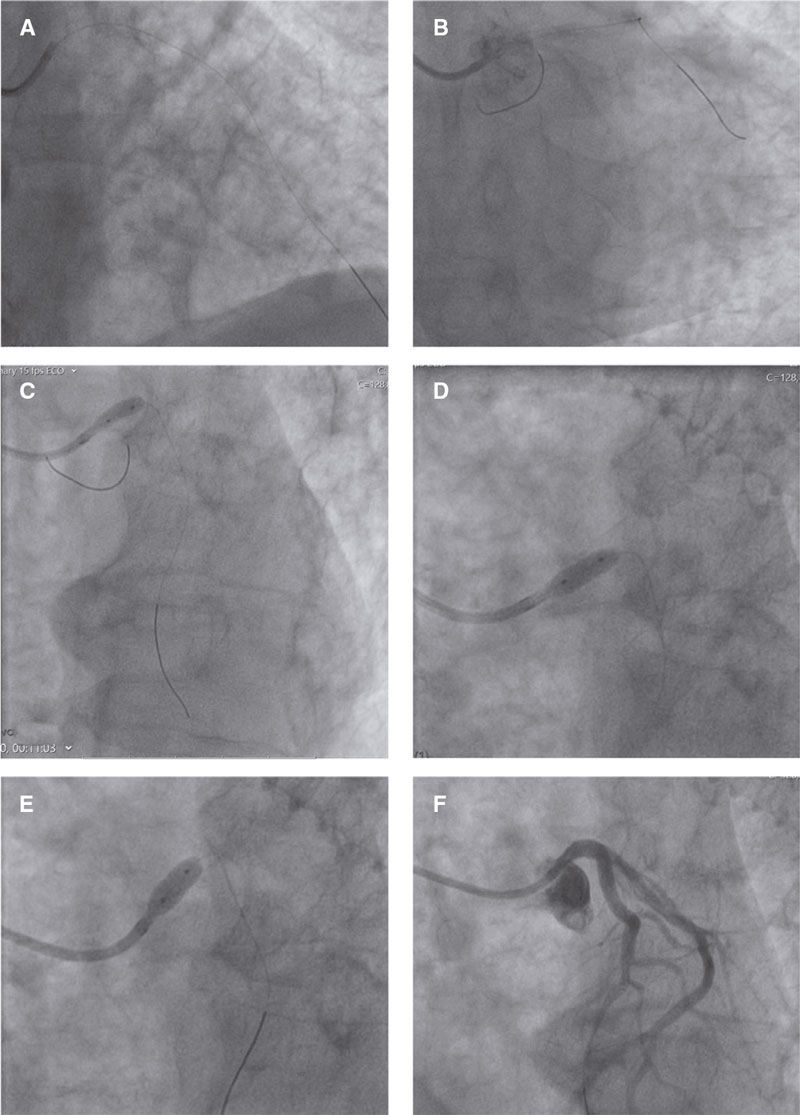
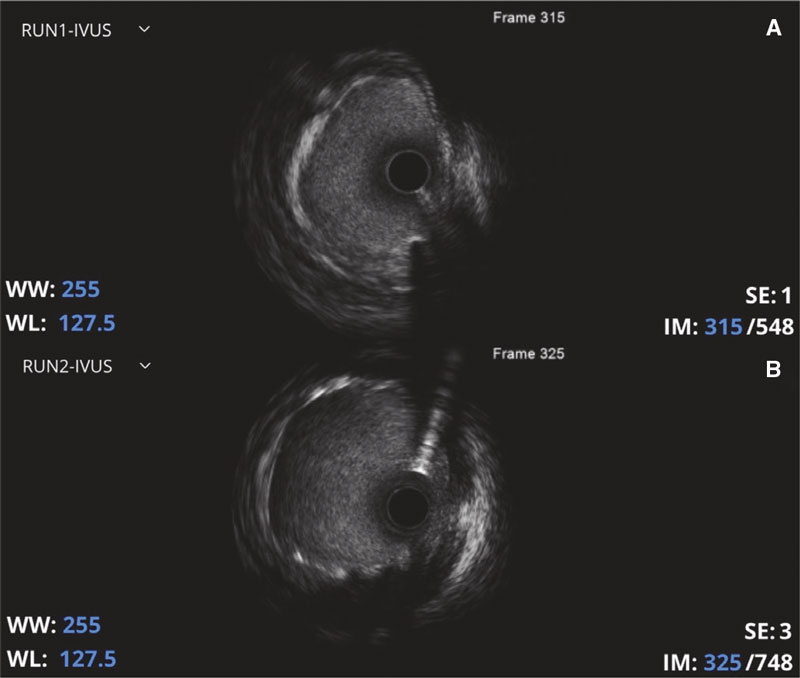
Due to the patient’s unstable and worsening hemodynamic condition, a coronary angioplasty using a drug-eluting stent was decided and successfully performed (figure 1, and figure 2). Before the angioplasty was performed, the patient was given a loading dose of ticagrelor 180 mg. The procedure was backed by intracoronary ultrasound (IVUS), which showed good stent positioning and expansion at the end of the procedure (minimum in-stent area of 16 mm2) (videos 3 and 4 of the supplementary data). No signs of coronary artery dissection were reported. After the procedure, the patient was pain-free, and blood pressure levels came back to normal.
Figure 1. Coronary angiography images. A: protection guidewire placed in the left anterior descending coronary artery. B: protection guidewire placed in the left circumflex artery. C: left main coronary artery predilatation with a noncompliant balloon (Emerge PTCA, Boston Scientific, United States; 3.5 mm × 8 mm; 16 atm); D: implantation of an everolimus-coated stent (XIENCE Sierra, Abbott, United States; 4.0 mm × 8 mm; 22 atm) in the left main coronary artery ostium. E: overdilatation of the previously implanted stent using another noncompliant balloon (Emerge PTCA, Boston Scientific, United States; 5.0 mm x 8 mm; 24 atm); F: good final angiographic results.
Figure 2. Intravascular ultrasound (IVUS). A: IVUS performed after predilatation showing a heterogeneous lesion at left main coronary artery ostium level possibly due to aortitis phenomena. B: the IVUS performed after stent implantation revealed proper stent expansion.
The transthoracic echocardiography was repeated, and confirmed a mildly dilated aortic root (40 mm to 41 mm) with apparent posterior wall thickening. The left ventricle was not dilated. The left ventricular ejection fraction was 30%-35% with an apical akinetic area, and anterior, lateral, and posterior walls. The right ventricular function was normal. No significant valvular disease, pericardial effusion or intracardiac masses were reported.
A thoracic computerized tomography scan showed multiple atheromatous aortic calcifications and significant wall thickening, which correlated to aortitis phenomena of syphilitic etiology. The patient remained on dual antiplatelet therapy and completed his antibiotic cycle with penicillin. The patient had favorable cardiovascular progression with gradual improvement of the left ventricular function and was discharged to the neurosurgery unit after 7 days. At 1 month, ticagrelor was withdrawn, and the patient underwent neurosurgery. His neurological recovery was uneventful and after 6 months, left ventricular function was normal.
Although cardiovascular signs have been previously described in the medical literature as well-known complications of syphilis, this case illustrates a particularly rare cardiac complication in the modern era.1-3 A possible sign of syphilitic aortitis is ostial coronary narrowing that can lead to an acute myocardial infarction, most cases being identified post-mortem.1 The underlying mechanism can be associated with atherosclerotic plaques, inflammatory phenomena, and/or calcium protrusion to the coronary arteries.1-3 High level of suspicion and the proper clinical setting were essential to achieve diagnosis and further treatment.1 Other differential diagnoses can be questioned like ankylosing spondylitis, temporal arteritis, and Takayasu’s arteritis since they can cause ascending aortitis.2,3
This case underlines the complexity of treating ostial lesions of left main coronary artery especially in situations where coronary obstruction seems to be conditioned by calcifications at ascending aorta, aortic root or aortitis level. Displacement of calcium in the aorta can lead to critical obstructions that, in the emergency setting, can complicate percutaneous revascularization or make it unfeasible. The absence of left ventricular assist devices and the close availability of cardiac surgery in our hospital made this scenario frightening and difficult to manage in the acute phase. Former studies have reported angioplasties in patients with left main coronary artery ostial stenosis, most requiring left ventricular assist devices to support the angioplasty of left main coronary artery.4-6 Fortunately for the patient, emergence angioplasty was possible with favorable cardiovascular progression. The patient’s written informed consent was obtained.
FUNDING
None whatsoever.
AUTHORS’ CONTRIBUTIONS
R. Flores, F. Mané, C. Braga, and C. Oliveira treated the patient. R. Flores drafted the manuscript, and F. Mané, C. Braga, and C. Oliveira reviewed it.
CONFLICTS OF INTEREST
None reported.
SUPPLEMENTARY DATA
Vídeo 1. Flores R. DOI: 10.24875/RECICE.M23000375
Vídeo 2. Flores R. DOI: 10.24875/RECICE.M23000375
Vídeo 3. Flores R. DOI: 10.24875/RECICE.M23000375
Vídeo 4. Flores R. DOI: 10.24875/RECICE.M23000375
REFERENCES
1. Jadeed R, Paarmann R, Harringer W, El-Essawi A. Syphilitic Aortitis Presenting with Coronary Ostial Stenosis and Aortic Regurgitation. J Heart Valve Dis. 2016;25:18-20.
2. Barbosa-Barros R, Pérez-Riera AR, Koivula K et al. Acute coronary syndrome of very unusual etiology. Ann Noninvasive Electrocardiol. 2018;23:e12531.
3. Nomura R, Yamazaki F, Egawa Y. Syphilitic aortitis: chronic left coronary ostial occlusion and aortic regurgitation with aortitis. Gen Thorac Cardiovasc Surg. 2021;69:736-739.
4. Predescu LM, Zarma L, Platon P, et al. ST Segment Elevation Myocardial Infarction Due to Severe Ostial Left Main Stem Stenosis in a Patient with Syphilitic Aortitis. Rom J Intern Med. 2016;54:74-79.
5. Li X, Wang X, Wang Z et al. Cardiovascular syphilis-associated acute myocardial infarction: A case report. Medicine (Baltimore). 2021;100:e24788.
6. Hosoba S, Suzuki T, Koizumi Y et al. Syphilitic aortitis causing bilateral coronary ostial stenosis. Heart Surg Forum. 2011;14:E59-60.