ABSTRACT
Introduction and objectives: Invasive diagnosis of vasoreactivity and microvascular function may be useful to optimize the management of patients with signs and/or symptoms of myocardial ischemia in the absence of significant coronary stenosis (INOCA). We analyzed the prevalence of the different endotypes, as well as the concordance between 2 diagnostic methods based on thermodilution assessment.
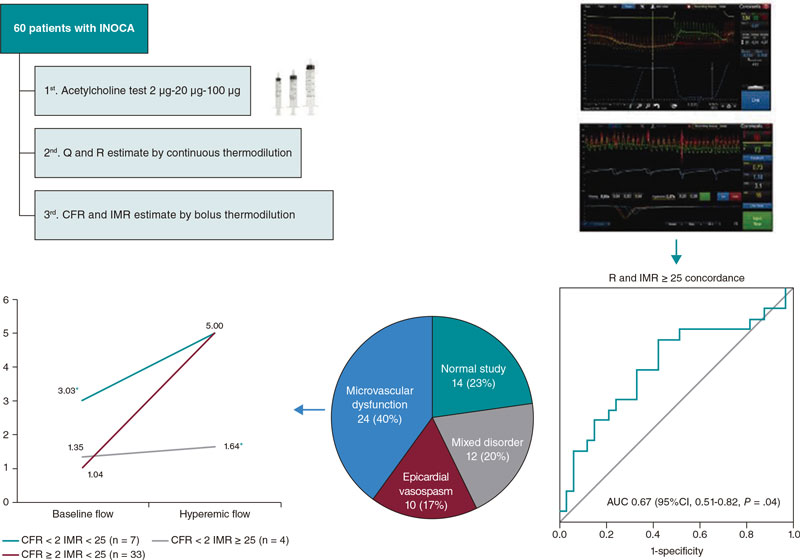
Methods: We prospectively included 60 patients with INOCA who underwent a vasoreactivity test with intracoronary acetylcholine, and measurement of absolute coronary blood flow (Q) and minimum microvascular resistance (R) using continuous thermodilution assessment. Finally, calculations of the coronary flow reserve (CFR) and index of microcirculatory resistance index (IMR) were made using the bolus thermodilution method considering CFR < 2 and MRI ≥ 25 as established pathological cut-off values.
Results: The invasive functional diagnostic procedure allowed patients to be categorized into 4 subgroups: microvascular dysfunction (40%), epicardial vasospasm (17%), mixed disorder (20%), and normal study (23%). No correlation was seen between the Q and the CFR. Using ROC curves, an R > 435 UW was estimated as the optimal cut-off value to identify patients with IMR ≥ 25 with an area under the curve of 0.67 (95%CI, 0.51-0.82; P = .04).
Conclusions: The invasive study of vasoreactivity and microcirculation was feasible and safe. Prevalence of vasospasm and microvascular dysfunction in patients with INOCA was high. The CFR/MRI/Q combined study allowed us to unmask a subtype of microvascular dysfunction characterized by an abnormally high coronary flow at baseline. The concordance seen between the microvascular resistance obtained by continuous thermodilution measurements and the reference method was low so future studies are justified to determine the usefulness of this technique.
Keywords: Microvascular dysfunction. Vasospasm. Acetylcholine. Continuous thermodilution measurements. Microvascular resistance. INOCA.
RESUMEN
Introducción y objetivos: El diagnóstico invasivo de la vasorreactividad y la función microvascular puede resultar de utilidad para optimizar el manejo de los pacientes con signos o síntomas de isquemia miocárdica en ausencia de estenosis coronarias significativas (INOCA). Se analizó la prevalencia de los distintos endotipos y la concordancia entre 2 métodos diagnósticos basados en la termodilución.
Métodos: Se incluyeron de forma prospectiva 60 pacientes con INOCA a quienes se realizó un test de vasorreactividad con acetilcolina intracoronaria, medida del flujo absoluto (Q) y la resistencia microvascular mínima (R) por termodilución continua y, por último, se calcularon la reserva de flujo coronario (RFC) y el índice de resistencia microvascular (IRM) por termodilución con bolos. Se consideraron como patológicos los puntos de corte establecidos de RFC < 2 e IRM ≥ 25.
Resultados: El procedimiento diagnóstico funcional invasivo permitió clasificar a los pacientes en 4 subgrupos: disfunción microvascular (40%), vasoespasmo epicárdico (17%), trastorno mixto (20%) y estudio normal (23%). No se observó correlación entre Q y RFC. Mediante curvas ROC se estimó una R > 435 UW como el punto de corte óptimo para identificar pacientes con IRM ≥ 25, con un área bajo la curva de 0,67 (IC95%, 0,51-0,82; p = 0,04).
Conclusiones: El estudio invasivo de la vasorreactividad y la microcirculación fue factible y seguro. La prevalencia de vasoespasmo y de disfunción microvascular en pacientes con INOCA fue elevada. El análisis conjunto de RFC, IRM y Q permitió desenmascarar un subtipo de disfunción microvascular caracterizado por un flujo coronario basal anormalmente elevado. La concordancia entre la resistencia microvascular obtenida por termodilución continua respecto al método de referencia fue baja, por lo que se requieren futuros estudios para determinar la utilidad de esta técnica.
Palabras clave: Disfunción microvascular. Vasoespasmo. Acetilcolina. Termodilución continua. Resistencia microvascular. INOCA.
Abbreviations
CFR: coronary flow reserve; INOCA: ischemia with nonobstructive coronary artery disease; IMR: index of microcirculatory resistance; Q: absolute coronary blood flow; R: coronary microvascular resistance.
INTRODUCTION
Over the past few years, the term INOCA (ischemia with nonobstructive coronary arteries) has established to define patients with signs or symptoms of ischemic heart disease without angiographically significant obstructive coronary artery disease.1 In these patients, coronary microvascular or epicardial vessel dysfunction could be the pathophysiological mechanism triggering the symptoms and ischemic impairment.2
Currently, the invasive study of microvascular function in patients with INOCA is a recommendation IIa according to the clinical practice guidelines of the European Society of Cardiology.3 What it does is measure the parameters that show its functional or structural status like coronary flow reserve (CFR) or index of microcirculatory resistance (IMR).4
Recently, the possibility of measuring absolute coronary blood flow (Q) and microvascular resistance (R) by continuous thermodilution with the infusion of a physiological saline solution through a specific coronary microcatheter has been described. This technique has potential advantages like its independence from the operator or not needing pharmacologically induced hyperemia.5
The objective of this study is to estimate the prevalence of the different endotypes of patients with INOCA and analyze the correlation between the measurements obtained by continuous thermodilution and the traditional method of intracoronary boluses of physiological saline solutions.
METHODS
This was a prospective and consecutive study of 60 referred patients due to symptoms or signs of myocardial ischemia without angiographically significant coronary artery stenosis on the visual estimate (< 50%) or after functional assessment (resting full-cycle ratio [RFR] > 0.89 or fractional flow reserve [FFR] > 0.80). Severe valvular heart disease, acute coronary syndrome, decompensated heart failure, and any clinical or anatomical condition where the study of microcirculation and vasoreactivity would be considered unnecessary were excluded.
All microcirculation and vasoreactivity studies were scheduled and second-staged. Nitrates and calcium antagonists were withdrawn prior to conducting the tests.
The coronary angiography was performed based on the routine clinical practice via radial access. A spasmolytic cocktail of 200 µg of nitroglycerin was administered. The target artery was the left main coronary artery.
The study was approved by the center ethics research committee and the patients’ written informed consent was obtained.
Vasoreactivity test
First, the vasoreactivity test was performed. Patient monitoring included precordial leads, and baseline angiograms were performed using 2 different projections. The sequential administration of acetylcholine was followed by increasing doses of 2 µg, 20 µg, and 100 µg in intracoronary bolus for 2 min. In the presence of significant bradycardia, the injection was interrupted, and if considered appropriate, it was re-administered at a slower rate. A follow-up angiogram was performed after every dose. In the presence of severe symptoms, changes to the echocardiogram or epicardial spasm 200 µg of intracoronary nitroglycerin were administered.
The test was considered positive based on the criteria established by the COVADIS (Coronary vasomotor disorders international study) group: epicardial spasm in the presence of chest pain, changes to the echocardiogram, and constriction ≥ 90%, and microvascular spasm in the presence of chest pain, and changes to the echocardiogram without epicardial spasm ≥ 90%.6
Indices obtained with continuous thermodilution
After the administration of unfractionated heparin (70 IU/kg), a pressure-temperature sensor guidewire Pressure Wire X (Abbott, United States) was inserted and pressures at the catheter distal border were equalized. The guidewire was advanced until it reached the left anterior descending coronary artery distal segment.
Resting full-cycle ratio was registered to confirm the lack of hemodynamically significant epicardial stenoses (RFR > 0.89).
Afterwards, a specific Rayflow (Hexacath, France) microcatheter for intracoronary infusion was placed in the left anterior descending coronary artery proximal segment. After confirmation that the guidewire sensor was, at least, 3 cm distal to the tip of the microcatheter, the intracoronary infusion of a physiological saline solution at room temperature and at a dose of 20 mL/min was started using an injector pump to induce hyperemia.
Pressure-temperatures curves were registered using Coroventis software (Abbott, United States). When the distal temperature drop was stabilized, the sensor was withdrawn up to the tip of the microcatheter to determine the infusion temperature.
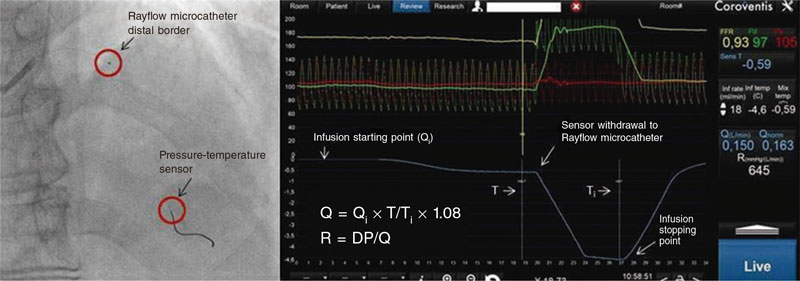
Afterwards, the injection of the physiological saline solution stopped, and Q (L/min) and R (Wood units) values were obtained automatically (figure 1).
Figure 1. Measurements obtained by continuous thermodilution: DP, distal pressure; Q, absolute coronary blood flow; Qi, infusion flow (mL/min); R, microvascular resistance; T, distal temperature; Ti, infusion temperature.
Indices obtained with bolus thermodilution of a physiological saline solution
After completion of the continuous thermodilution study, and once the Rayflow microcatheter was removed, the pressure-temperature guidewire was repositioned in its previous location, and thermodilution curves were registered using the Coroventis software after the vigorous manual injection of 3 intracoronary boluses of 3 mL of a physiological saline solution. Measurements were taken at rest and after inducing hyperemia with a peripheral intravenous bolus of regadenoson (400 µg) resulting in the calculation of CFR and IMR.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation or median [interquartile range]. The categorical ones were expressed as absolute value or percentage. ROC (Receiver operating characteristic) curves were used to estimate the optimal cut-off values for the continuous variables Q and R. The cut-off values established as pathological for CFR < 2 and IMR ≥ 25 were used as the reference framework. Once dichotomized, the variables Q and R were compared to the CFR and IMR values using chi-square tests. One-way ANOVA was used to compare the different quantitative variables. The statistical analysis was performed using the SPSS v 20 statistical software package (IBM, United States).P values < .05 were considered statistically significant.
RESULTS
Study patients
Table 1 shows the baseline characteristics of the 60 patients included in the study. Women (55%) were predominant. Also, there was a high prevalence of cardiovascular risk factors. Most showed typical angina-like clinical signs (76%) and had tested positive to an ischemia test performed before the coronary angiography (60%).
Table 1. Clinical and angiographic characteristics (N = 60)
| Age (years) | 63 ± 10 |
| Women | 33 (55%) |
| Hypertension | 39 (65%) |
| Diabetes | 21 (35%) |
| Dyslipidemia | 35 (58%) |
| Smoking (current or past) | 28 (47%) |
| Previous percutaneous revascularization | 4 (7%) |
| Previous myocardial infarction | 3 (5%) |
| Left ventricular systolic dysfunction | 4 (7%) |
| Ejection fraction (%) | 63 ± 8 |
| Clinical presentation | |
| Exertional angina | 19 (32%) |
| Resting angina | 13 (22%) |
| Mixed angina | 14 (23%) |
| Other | 14 (24%) |
| Ischemia test | |
| Ergometry | 19 (32%) |
| Isotopic scintigraphy | 18 (30%) |
| Dobutamine stress echocardiography | 3 (5%) |
| None | 20 (33%) |
| Coronary angiography | |
| Atheromatous disease | 22 (37%) |
| Slow flow | 13 (22%) |
|
Data are expressed as no. (%) or mean ± standard deviation. |
|
The baseline coronary angiography confirmed that 37% of the patients showed parietal irregularities consistent with atheromatous disease, and 22% had slow coronary flow. The FFR and RFR values were normal in all the cases studied.
Coronary vasoreactivity
As shown on table 2, 60% of the cases (36/60) had a positive response to acetylcholine in the vasoreactivity test. A total of 32% of the cases (19/60) showed severe epicardial vasoconstriction, and 23% (14/60) met the criteria for microvascular spasm. In 3 patients (5%), microvascular spasm was observed concomitantly with the medium dose (20 µg), and epicardial spasm with the high dose (100 µg), which added to the impaired indices of microvascular function was consistent with a mixed endotype.
| Pathological vasoreactivity testing | 36 (60%) |
| Epicardial vasospasm | 19 (32%) |
| Microvascular vasospasm | 14 (23%) |
| Combined vasospasm | 3 (5%) |
| Structural microvascular dysfunction (IMR ≥ 25) | 20 (33%) |
| Isolated | 5 (8%) |
| Associated with epicardial spasm | 8 (13%) |
| Associated with microvascular spasm | 4 (7%) |
| Associated with combined spasm | 3 (5%) |
| CFR < 2 | 11 (18%) |
| CFR < 2.5 | 17 (28%) |
| RFR | 0.93 [0.91-0.94] |
| FFR | 0.90 [0.87-0.93] |
| Q (mL/min) | 170 ([138-219] |
| R (WU) | 496 [381-654] |
| CFR | 3.0 [2.3-4.2] |
| IMR | 20 [12-28] |
|
Data are expressed as no. (%) or median [interquartile range]. |
|
Indices of microvascular function
Both studies—bolus thermodilution and continuous infusion thermodilution—were performed uneventfully in all of the patients. Table 2 shows the values of the measurements of microvascular function obtained with both techniques.
In the continuous infusion study, a median of absolute flow in the left anterior descending coronary artery of 170 mL/min [138-219 mL/min] was described while the median of microvascular resistance was 496 WU [381-654 WU].
A total of 18% of the patients (11/60) had a reduced CFR (CFR < 2) while 33% (20/60) showed elevated resistances (IMR ≥ 25).
The group of patients with microvascular dysfunction due to low CFR with normal IMR (7/60, 12%) with respect to cases with microvascular dysfunction due to high IMR with normal CFR (16/60, 27%) had a clinical profile with a lower mean age (61 ± 11 vs 66 ± 8), and a higher predominance of women (86% vs 58%) although this tendency was not statistically significant.
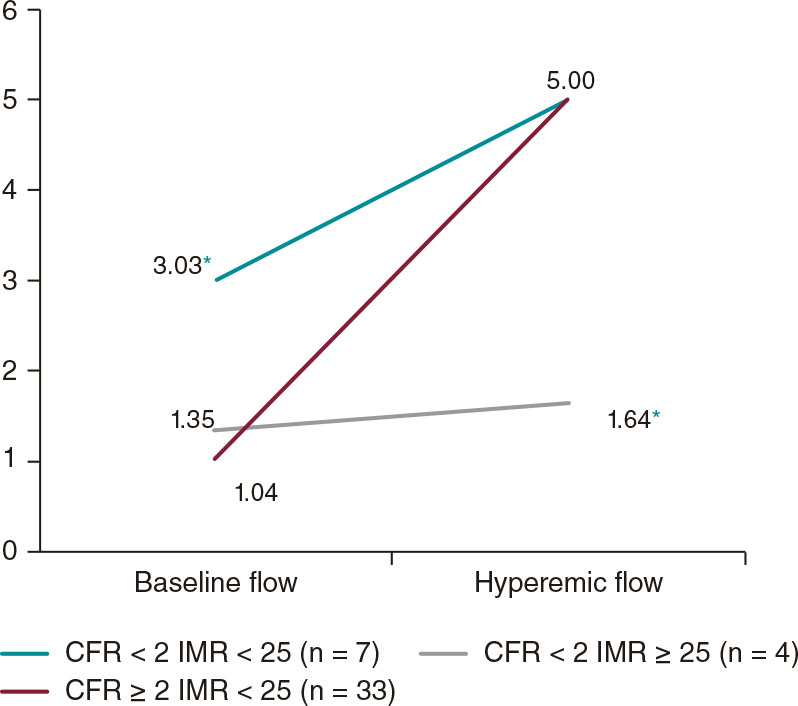
Table 3 shows the mean transit times (MTT) of bolus thermodilution tests. The cases with low CFR showed significantly shorter baseline MTT (0.48 ± 0.45 vs 1.13 ± 0.70), especially the subgroup of patients with low CFR and high Q (0.31 ± 0.15 vs 0.77 ± 0.68).
Table 3. Mean transit times obtained by bolus thermodilution
| Overall (N = 60) |
CFR < 2 (N = 11) |
CFR < 2 Q > 170 (N = 7) |
CFR < 2 Q < 170 (N = 4) |
|
|---|---|---|---|---|
| Baseline MTT | 1.13 ± 0.70 | 0.48 ± 0.45* | 0.31 ± 0.15* | 0.77 ± 0.68 |
| Hyperemic MTT | 0.36 ± 0.25 | 0.35 ± 0.28 | 0.25 ± 0.14 | 0.51 ± 0.41 |
|
Values (in seconds) are expressed as mean ± standard deviation. |
||||
Figure 2 shows data of coronary flow estimated by MTT measurement divided into 3 groups based on CFR and IMR results. We should mention that patients with low CFR without elevated resistances had significantly high resting flows and hyperemic flows without significant differences compared to the rest while in patients with low CFR and elevated resistances, the opposite phenomenon was described.
Figure 2. Baseline and hyperemic mean flow estimated based on the MTT (1/MTT) and grouped based on the CFR and IMR results. Values are expressed as s–1. CFR, coronary flow reserve; IMR, index of microvascular resistance; MTT, mean transit time.
* P < .05.
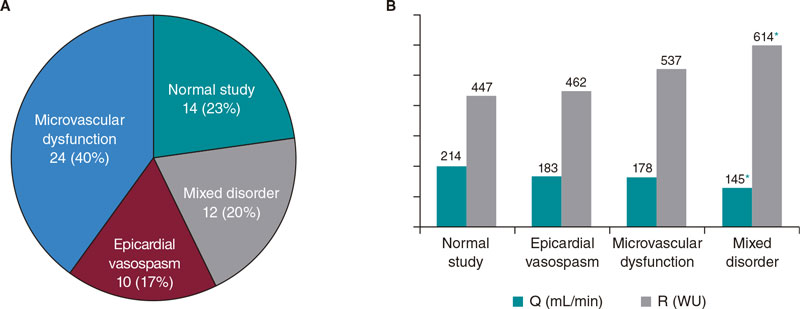
Endotypes
Figure 3A shows the percentages of endotypes based on the result of the acetylcholine test and the measurements of CFR and IMR. The most common pattern was microvascular dysfunction (24/60, 40%) followed by the normal study (14/60, 23%). In 20% of the patients (12/60), microvascular dysfunction overlapped with epicardial vasospasm while in 17% of the patients (10/60) isolated epicardial vasospasms were seen.
Figure 3. A: endotype-based classification. Values are expressed as absolute number and percentage.B: mean values of absolute flow and microvascular resistance grouped by endotypes. Q, absolute coronary blood flow; R, microvascular resistance.
* P < .05 with respect to normal study.
Table 4 shows how the mechanisms of vasomotor and microvascular dysfunction overlap in many cases.
Table 4.Results of the acetylcholine test and bolus thermodilution study (N = 60)
| Epicardial spasm | Microvascular spasm | IMR ≥ 25 | CFR < 2 | Endotype | Cases |
|---|---|---|---|---|---|
| − | − | − | − | Normal | 14 (23.3%) |
| + | − | − | − | Epicardial vasospasm | 10 (16.7%) |
| − | + | − | − | Microvascular dysfunction | 9 (15.0%) |
| − | − | + | − | Microvascular dysfunction | 5 (8.3%) |
| − | − | − | + | Microvascular dysfunction | 5 (8.3%) |
| − | + | + | − | Microvascular dysfunction | 3 (5.0%) |
| − | + | − | + | Microvascular dysfunction | 1 (1.6%) |
| − | + | + | + | Microvascular dysfunction | 1 (1.6%) |
| + | − | + | − | Mixed disorder | 6 (10.0%) |
| + | + | + | − | Mixed disorder | 2 (3.3%) |
| + | − | + | + | Mixed disorder | 2 (3.3%) |
| + | − | − | + | Mixed disorder | 1 (1.6%) |
| + | + | + | + | Mixed disorder | 1 (1.6%) |
|
Data are expressed as no. (%) |
|||||
The association between epicardial vasospasm and structural microvascular dysfunction (IMR ≥ 25) was the most prevalent combination in cases of mixed disorder (11/12). In turn, this endotype, in continuous thermodilution measurements, showed significant differences compared to the normal pattern, with reduced absolute flow values and elevated resistances (figure 3B) indicative of more serious structural and functional damage.
Concordance among the different indices of microvascular function
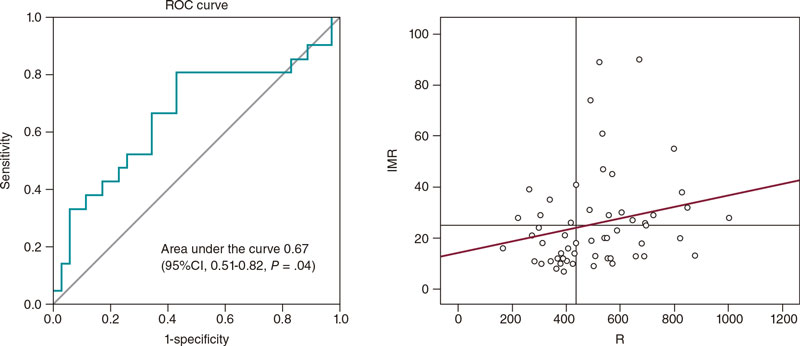
The ROC curve analysis of absolute coronary blood flow (Q) with respect to CFR < 2 determined an optimal cut-off value of 170 mL/min (a 64% sensitivity, and a 52% specificity) with an area underthe curve of 0.50 (95% confidence interval [95%CI], 0.33-0.66;P = .97), therefore showing no diagnostic utility.
Given the recent proposal to consider the cut-off value of CFR < 2.57,7 the analysis was performed using this threshold as the reference. In addition, no significant concordance was seen (area under the curve of 0.45 [95%CI, 0.30-0.61;P = .56]).
Regarding R with respect to IMR, an area under the curve of 0.67 (95%CI, 0.51-0.82;P = .04) was obtained, which was indicative of a weak yet significant diagnostic concordance (figure 4). The estimated optimal cut-off value was 435 WU, which was consistent with an 81% sensitivity and a 57% specificity. A total of 66% of cases with IMR ≥ 25 were categorized correctly using this index.
Figure 4. Analysis of the R cut-off value > 435 WU to predict IMR ≥ 25, and scatter plot showing the correlation between IMR and R. IMR, index of microvascular resistance; R, microvascular resistance.
The absence of an association between Q and CFR was confirmed in correlation tests (Spearman’s rho correlation coefficient= -0.02; 95%CI, -0.24-0.25;P = .99). However, a weak yet significant correlation was seen between Q and hyperemic MTT (Spearman’s rho= -0.28; 95%CI, -0.01-0.51;P = .04), and between R and IMR (Spearman’s rho= 0.28; 95%CI, 0.04-0.51;P = .03).
Complications
While the vasoreactivity test was being performed, 3 cases of transient bradycardia (5%) without clinical repercussions and 2 episodes of atrial fibrillation (4%) were reported, 1 of them self-limited while the other required sedation and electrical cardioversion. After the administration of regadenoson, most patients experienced some degree of discomfort, which was well-tolerated and reversed with the administration of 100 mg of intravenous theophylline. No other complications or adverse effects were reported.
DISCUSSION
This study confirms that a high percentage of patients with symptoms or signs of INOCA show microvascular dysfunction or vasospasm in invasive functional testing, and that it is feasible and safe to perform (figure 5).
Figure 5. Study design, endotype-based classification, and analysis using the ROC curve. AUC, area under the curve; CFR, coronary flow reserve; IMR, index of microvascular resistance; INOCA, ischemia with nonobstructive coronary artery disease; Q, absolute coronary blood flow; R, microvascular resistance.
* P < .05.
The percentage of patients with microcirculation or vasomotility alterations found in our study (77%) is consistent with former studies of patients with angina without obstructive coronary artery disease (64% to 89%8-11).
Vasoreactivity test
Some groups systematically use a dose of 200 µg of intracoronary acetylcholine to perform the vasoreactivity test; in our study, the high dose was established at 100 µg according to the COVADIS group, the CorMicA protocol, and the technical document of the Spanish Society of Cardiology Working Group on Cardiac Catheterization and Interventional Cardiology, which highlights its high sensitivity and specificity rates (90% and 99%, respectively).12 As a matter of fact, the high prevalence of positive results seen in our study in the acetylcholine test (60%) is similar to that reported in other series (57% to 71%13-15). In a recent study of 110 patients, Feenstra et al.11 revealed that 62% of the patients had a pathological acetylcholine test that confirmed the presence of epicardial vasospasm and microvascular spasm (36% and 26%, respectively).
In our study, the complications associated with the vasoreactivity test in our study are not very many: 2 cases of atrial fibrillation (4%), which is consistent with the incidence rate reported by the CorMIcA trial (5%).9
Prevalence of endotypes
The most common endotype in our patients was isolated microvascular dysfunction (40%), but not as much as in the CorMicA trial (52%). These differences could be explained by the discrepancy seen in the percentage of completely normal angiographies (22% in the CorMicA vs 63% in our study) due to the possible association between non-obstructive atheromatous disease and microvascular dysfunction.16,17
The prevalence of the remaining endotypes is similar to that reported in the CorMicA trial: isolated epicardial vasospasm (17% vs 17%), and mixed disorder (20% vs 21%). A recent meta-analysis that included 14 427 patients with INOCA also shows similar percentages.18
Indices of microvascular function obtained through bolus thermodilution
The analysis of the MTT obtained with this technique (figure 2), a parameter that correlates inversely with the direct measurement of coronary flow,19 reveals an interesting finding that is consistent with the data published by Nardone et al.20: patients with low CFR have 2 differentiated phenotypes based on the IMR. On the one hand, cases with reduced CFR and elevated resistances have normal baseline flow and low hyperemic flow, which would be indicative of an insufficient vasodilation response. However, in patients with normal resistances, a reduced CFR would be indicative of an abnormally elevated resting flow with hyperemic flow in the normal range. This phenomenon can also be observed in the analysis of patients with high Q (table 3) in whom a reduced CFR can be attributed to elevated baseline flow instead of an insufficient hyperemic response.
Therefore, this subgroup probably shows inefficient or dysregulated baseline myocardial flows. This characteristic, of indeterminate cause, could have important therapeutic implications like a lack of response to vasodilator drugs.
Indices of microvascular function obtained by continuous thermodilution
The continuous thermodilution technique has evolved to the point of quantifying Q and R with a microcatheter and specific software in a simple and precise fashion. The main advantages of this method are its independence from an operator, reproducibility, and induction of hyperemia with a physiological saline solution without the need for pharmacological agents.21-24 However, its main limitation is the lack of normal reference values.
In our study, the lack of a correlation between Q and CFR could be justified by the variations described of baseline myocardial flow. Estimating the CFR requires estimating the baseline coronary flow while Q is a measurement that is representative of hyperemic flow.
The weak concordance seen in this study between Q and hyperemic MTT and between R and IMR shows how difficult it is to establish valid cut-off values for patient comparison with these indices.
With an optimal cut-off value of R in our study of 435 WU (an 81% sensitivity, and a 57% specificity), a total of 66% of cases with IMR ≥ 25 were properly categorized with this index. This value is somewhat lower compared to the one shown by Rivero et al.,25 who analyzed 120 patients and found that an R > 500 WU properly categorized 80% of the cases with IMR ≥ 25.Konst et al.26 studied 84 patients with INOCA using both thermodilution techniques only to find no correlation between the Q-R combo and IMR.
The differences seen may be explained by the fact that the quantitative variability of Q and R values among individuals mostly depends on myocardial mass. However, in positron emission tomography studies, considerable ranges were seen even after adjusting for flow and resistance values for myocardial mass. Therefore, it has been speculated that the most plausible hypothesis is the natural variation of hyperemic myocardial perfusion among individuals.27
Therefore, indices like CFR estimated by continuous thermodilution and microvascular resistance reserve are currently in the pipeline. They correlate the absolute values of flow and resistance seen during hyperemia with those obtained at rest. Nonetheless,these new parameters will still need validation in futurestudies.28,29
Limitations
The data presented here should be interpreted while understanding that this is an observational, single-center study with a small sample size. Therefore, results may be biased by confounding factors associated with a study of this nature.
The left anterior anterior descending coronary artery was considered as the pre-specified target vessel. However, in the routine clinical practice, it may be appropriate to assess other arteries in the presence of negative tests and high clinical suspicion.1
The optimal sequence in invasive functional studies has not been established yet.1 In our case, we chose to perform the acetylcholine test first to minimize the instrumentation of the artery and avoid further guidewire-induced vasoreactivity. However, the spasm and symptoms seen during the provocation test, although transient, could interfere with subsequent measurements of microvascular function. The possibility of determining CFR by continuous thermodilution was established at the beginning of our study, and it was assumed that a comparison of the CFRs obtained with both techniques would have been more appropriate.
In most bolus thermodilution studies, intravenous adenosine is used to induce hyperemia. However, we chose regadenoson because it is easy to use, following our previous experience, and because evidence says it is equivalent to adenosine.30,31
Finally, we should not overlook that this is an invasive study so potential risks associated with the examination should be weighed in. To this date, however, conducting this study has not impacted prognosis.
CONCLUSIONS
The invasive study of coronary vasoreactivity and microcirculation is feasible and safe. These studies allow us to easily recognize different endotypes of patients with INOCA and help us optimize their treatment.
The analysis of CFR, IMR, and Q combined can unmask a subtype of microvascular dysfunction characterized by an abnormally high baseline coronary flow.
The new indices obtained by continuous thermodilution show low concordance with respect to the reference indices. Therefore, future studies will be required to determine the utility of this technique.
FUNDING
None whatsoever.
AUTHORS’ CONTRIBUTIONS
All the authors contributed substantially to the study idea, design, and data mining process. In addition, all approved the manuscript final version for publication.
CONFLICTS OF INTEREST
None reported.
WHAT IS KNOWN ABOUT THE TOPIC?
- The invasive diagnosis of microvascular dysfunction and coronary vasospasm have proven useful to improve the quality of life of patients without obstructive coronary artery disease on the coronary angiography.
- Indices of microvascular dysfunction obtained by continuous thermodilution offer potential advantages since are they are independent from the operator, reproducible, and do not require pharmacologically induced hyperemia.
WHAT DOES THIS STUDY ADD?
- Invasive coronary functional diagnosis is feasible and safe and highlights the high prevalence of microcirculation and vasomotility alterations in patients without obstructive coronary artery disease.
- The combined analysis of the different indices may be useful to characterize cases with decreased CFR.
- Future studies are needed to establish the utility of microvascular function measurements obtained by continuous thermodilution.
REFERENCES
1. Kunadian V, Chieffo A, Camici PG, et al. An EAPCI Expert Consensus Document on Ischaemia with Non-Obstructive Coronary Arteries in Collaboration with European Society of Cardiology Working Group on Coronary Pathophysiology & Microcirculation Endorsed by Coronary Vasomotor Disorders International Study Group. Eur Heart J. 2020;41:3504-3520.
2. Camici PG, Crea F. Coronary microvascular dysfunction. N Engl J Med. 2007;356:830-840.
3. Knuuti J, Wijns W, Saraste A, et al. ESC Scientific Document Group. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41:407-477.
4. Ford TJ, Ong P, Sechtem U, et al. COVADIS Study Group. Assessment of Vascular Dysfunction in Patients Without Obstructive Coronary Artery Disease: Why, How, and When. JACC Cardiovasc Interv. 2020;13:1847-1864.
5. Xaplanteris P, Fournier S, Keulards DCJ, et al. Catheter-Based Measurements of Absolute Coronary Blood Flow and Microvascular Resistance: Feasibility, Safety, and Reproducibility in Humans. Circ Cardiovasc Interv. 2018;11:e006194.
6. Beltrame JF, Crea F, Kaski JC, et al., On Behalf of the Coronary Vasomotion Disorders International Study Group (COVADIS). International standardization of diagnostic criteria for vasospastic angina. Eur Heart J. 2015;38:
2565-2568.
7. Demir OM, Boerhout CKM, de Waard GA, et al. Comparison of Doppler Flow Velocity and Thermodilution Derived Indexes of Coronary Physiology. JACC Cardiovasc Interv. 2022;15:1060-1070.
8. Suda A, Takahashi J, Hao K, et al. Coronary functional abnormalities in patients with angina and nonobstructive coronary artery disease. J Am Coll Cardiol. 2019;74:2350-2360.
9. Ford TJ, Stanley B, Good R, et al. Stratified medical therapy using invasive coronary function testing in angina: the CorMicAtrial. J Am Coll Cardiol. 2018;72:2841-2855.
10. Sara JD, Widmer RJ, Matsuzawa Y, Lennon RJ, Lerman LO, Lerman A. Prevalence of Coronary Microvascular Dysfunction Among Patients With Chest Pain and Nonobstructive Coronary Artery Disease. JACC Cardiovasc Interv. 2015;8:1445-1453.
11. Feenstra RGT, Boerhout CKM, Woudstra J, et al. Presence of Coronary Endothelial Dysfunction, Coronary Vasospasm, and Adenosine-Mediated Vasodilatory Disorders in Patients With Ischemia and Non obstructive Coronary Arteries. Circ Cardiovasc Interv. 2022;15:e012017.
12. Gutiérrez E, Gómez-Lara J, Escaned J, et al. Valoración de la función endotelial y provocación de vasoespasmo coronario mediante infusión intracoronaria de acetilcolina. Documento técnico de la ACI-SEC. REC Interv Cardiol. 2021;3:286-296.
13. Aziz A, Hansen HS, Sechtem U, Prescott E, Ong P. Sex-Related Differences in Vasomotor Function in Patients With Angina and Unobstructed Coronary Arteries. J Am Coll Cardiol. 2017;70:2349-2358.
14. Seitz A, Gardezy J, Pirozzolo G, et al. Long-Term Follow-Up in Patients With Stable Angina and Unobstructed Coronary Arteries Undergoing Intracoronary Acetylcholine Testing. J Am Coll Cardiol Interv. 2020;13:1865-1876.
15. Ong P, Athanasiadis A, Borgulya G, et al. Clinical usefulness, angiographic characteristics, and safety evaluation of intracoronary acetylcholine provocation testing among 921 consecutive white patients with unobstructed coronary arteries. Circulation. 2014;129:1723-1730.
16. Melikian N, Vercauteren S, Fearon WF, et al. Quantitative assessment of coronary microvascular function in patients with and without epicardial atherosclerosis. EuroIntervention. 2010;5:939-945.
17. Sharaf B, Wood T, Shaw L, et al. Adverse outcomes among women presenting with signs and symptoms of ischemia and no obstructive coronary artery disease: findings from the National Heart, Lung, and Blood Institute-sponsored Women’s Ischemia Syndrome Evaluation (WISE) angiographic corelaboratory. Am Heart J. 2013;166:134-141.
18. Mileva N, Nagumo S, Mizukami T, et al. Prevalence of Coronary Microvascular Disease and Coronary Vasospasm in Patients With Nonobstructive Coronary Artery Disease: Systematic Review and Meta-Analysis. J Am Heart Assoc. 2022;11:e023207.
19. De Bruyne B, Pijls NH, Smith L, et al. Coronary thermodilution to assess flow reserve: experimental validation. Circulation. 2001;104:2003-2006.
20. Nardone M, McCarthy M, Ardern CI, et al. Concurrently Low Coronary Flow Reserve and Low Index of Microvascular Resistance Are Associated With Elevated Resting Coronary Flow in Patients With Chest Pain and Nonobstructive Coronary Arteries. Circ Cardiovasc Interv. 2022;15:e011323.
21. Van’t Veer M, Adjedj J, Wijnbergen I, et al. Novel monorail infusion catheter for volumetric coronary blood flow measurement in humans: invitro validation. EuroIntervention. 2016;12:701-707.
22. Rivero F, Bastante T, Cuesta J, García-Guimaraes M, Maruri-Sánchez R, Alfonso F. Volumetric Quantification of Coronary Flow by Using a Monorail Infusion Catheter: Initial Experience. Rev Esp Cardiol. 2018;71:1082-1084.
23. Everaars H, de Waard GA, Schumacher SP, et al. Continuous thermodilution to assess absolute flow and microvascular resistance: validation in humans using [15O] H2O positron emission tomography. Eur Heart J. 2019;40:2350-2359.
24. Keulards DCJ, Van’t Veer M, Zelis JM, et al. Safety of absolute coronary flow and microvascular resistance measurements by thermodilution. EuroIntervention. 2021;17:229-232.
25. Rivero F, Gutiérrez-Barrios A, Gomez-Lara J, et al. Coronary microvascular dysfunction assessed by continuous intracoronary thermodilution: A comparative study with index of microvascular resistance. Int J Cardiol. 2021;333:1-7.
26. Konst RE, Elias-Smale SE, Pellegrini D, et al. Absolute Coronary Blood Flow Measured by Continuous Thermodilution in Patients With Ischemia and Nonobstructive Disease. J Am Coll Cardiol. 2021;77:728-741.
27. Fournier S, Keulards DCJ, van’t Veer M, et al. Normal values of thermodilution-derived absolute coronary blood flow and microvascular resistance in humans. EuroIntervention. 2021;17:e309-e316.
28. Gutiérrez-Barrios A, Izaga-Torralba E, Rivero Crespo F, et al. Continuous Thermodilution Method to Assess Coronary Flow Reserve. Am J Cardiol. 2021;141:31-37.
29. De Bruyne B, Pijls NHJ, Gallinoro E, et al. Microvascular Resistance Reserve for Assessment of Coronary Microvascular Function: JACC Technology Corner. J Am Coll Cardiol. 2021;78:1541-1549.
30. Federico P, Martínez L, Castelló T, Pomar F, Peris E. Regadenoson intravenoso frente a adenosina intracoronaria para la medida de la reserva fraccional de flujo. REC Interv Cardiol. 2019;1:77-82.
31. Gill GS, Gadre A, Kanmanthareddy A. Comparative efficacy and safety of adenosine and regadenoson for assessment of fractional flow reserve: A systematic review and meta-analysis. World J Cardiol. 2022;14:
319-328.