ABSTRACT
Introduction and objectives: Coronary artery aneurysms are a complex situation. Our main objective is to describe the frequency of use of covered stents (grafts) for their management, as well as to characterize their long-term results compared to drug-eluting stents.
Methods: Ambispective observational study with data from the International Coronary Artery Aneurysm Registry (CAAR) (NCT-02563626). Only patients who received a stent-graft or a drug-eluting stent where the aneurysm occurred were selected.
Results: A total of 17 patients received, at least, 1 stent-graft while 196 received 1 drug-eluting in the aneurysmal vessel. Male predominance, a higher rate of dyslipidemia, a past medical history of coronary artery disease, previously revascularized coronary artery disease, and giant aneurysms were reported in the stent-graft cohort. The independent predictive variables of the composite endpoint of all-cause mortality, heart failure, unstable angina, reinfarction, stroke, systemic embolism, bleeding or any aneurysmal complications at the median follow-up of 38 months were suggestive of the existence of connective tissue diseases (HR, 5.94; 95%CI, 1.82-19.37), left ventricular dysfunction ≤ 55% (HR, 1.84; 95%CI, 1.09-3.1), and an acute indication for heart catheterization (HR, 2.98; 95%CI, 1.39-6.3). The use of stent-grafts was not associated with the occurrence of more composite endpoints (23.5% vs 29.6%; P = .598).
Conclusions: The use of stent-grafts to treat coronary aneurysms is feasible and safe in the long-term. Randomized clinical trials are needed to decide what the best treatment is for these complex lesions.
Keywords: Coronary aneurysm. Registry. Stent. Stent graft. Angioplasty.
RESUMEN
Introducción y objetivos: Los aneurismas coronarios son una situación compleja. Planteamos como objetivo principal describir la frecuencia de utilización de stents recubiertos (grafts) para su tratamiento y caracterizar sus resultados a largo plazo en comparación con stents farmacoactivos.
Métodos: Estudio observacional ambispectivo, con información procedente del Registro Internacional de Aneurismas Coronarios (CAAR) (NCT-02563626). Se seleccionaron los pacientes que recibieron un stent-graft o un stent farmacoactivo en la zona del aneurisma.
Resultados: Un total de 17 pacientes recibieron al menos un stent-graft y 196 un stent farmacoactivo en la zona aneurismática. Se observa un predominio del sexo masculino y una mayor frecuencia de dislipemia, antecedentes de coronariopatía, enfermedad coronaria revascularizada previamente y aneurismas gigantes en la cohorte de stent-graft. Como variables independientes predictoras del desarrollo del evento combinado (muerte por cualquier causa, insuficiencia cardiaca, angina inestable, reinfarto, ictus, embolia sistémica, sangrado o cualquier complicación en el aneurisma), tras una mediana de seguimiento de 38 meses, destacaron la existencia de conectivopatías (hazard ratio [HR] = 5,94; intervalo de confianza del 95% [IC95%], 1,82-19,37), la disfunción del ventrículo izquierdo ≤ 55% (HR = 1,84; IC95%, 1,09-3,1) y la indicación aguda del cateterismo índice (HR = 2,98; IC95%, 1,39-6,3). El uso de stent-grafts comparado con el de stents farmacoactivos no se asoció al desarrollo de más eventos combinados (23,5 frente a 29,6%; p = 0,598).
Conclusiones: El uso de stents recubiertos en aneurismas coronarios es factible y seguro a largo plazo. Se necesitan estudios clínicos aleatorizados para decidir el mejor tratamiento de este tipo de lesiones complejas.
Palabras clave: Aneurismas coronarios. Registro. Resultados. Stent. Stent-graft. Angioplastia.
Abbreviations
LVEF: Left ventricular ejection fraction.
INTRODUCTION
The first descriptions of a coronary aneurysm were reported by Morgagni back in 1761, and the first series of 21 patients were reported in 1929.1-4 Since then, a variable incidence rate—between 0.3% and 12%—has been reported in several series following the implementation of imaging modalities and coronary angiography.5 The overall incidence rate reported in a cohort of over 436 000 contemporary coronary angiographies from an international registry is 0.35%.5 Same as it happens with the clinical presentation and profile, treatment varies significantly.5,6 Still, revascularization is often required here.6 Over the last few years, some of the alternatives available propose the use of stent-grafts for the exclusion of coronary aneurysms.5-14
These devices—initially developed for other indications15 such as coronary perforations—have proven useful and safe in the short-term, and in cases and series previously published.7-10,12
The main goal of this paper is to describe the frequency of use of this type of stents for the management of coronary aneurysms and characterize its long-term results using patients with drug-eluting stents as the control group since they have had good results in this context.5
METHODS
This paper uses data curated from the International Coronary Artery Aneurysm Registry (CAAR) (NCT-02563626).16 Using a methodology already published, this ambispective registry included data from adult patients (≥ 18 years) who underwent a coronary angiography for whatever reason in 32 hospitals from 9 different countries.5 Coronary aneurysm was defined as a focal dilatation (< 1/3 of the vessel) 1.5 times larger compared to the vessel diameter in a healthy adjacent segment; the giant aneurysm was defined as a dilatation 4 times larger compared to the reference diameter.16 Investigators were advised to collect a consecutive case series in specific closed periods of time. Both the clinical and the procedural variables were collected, as well as the events occurred during the index hospital stay considered as that moment when it was first reported that the patient had, at least, 1 coronary aneurysm. Then, after validating which patients were eligible, the clinical follow-up was performed with information from the health records collected via medical consultations or phone calls. As stated in former reports, the protocol was initially approved by the coordinating center ethics committee and then by the centers that required it. Data were collected anonymously, and patients gave their informed consent to all the study procedures. Clinical decisions were always made by the treating physician of every patient without any influence from the study protocol whatsoever. The analysis of this study only included patients who received a stent-grafts or drug-eluting stents in an aneurysmal area.
The study primary endpoint was to describe the real-life use of stent-grafts to treat coronary aneurysms. Secondary endpoints were to determine the occurrence of events at the long-term follow-up. Similarly, another secondary endpoint was to conduct a comparison with patients who received drug-eluting stents in the aneurysmal area. If both types of stents were implanted, the patient from the stent-graft group was considered. Similarly, the analyses were conducted individually in each patient.
Statistical analysis
The statistical package SPSS v24.0 (IBM-SPSS, United States) was used to conduct the statistical analysis. Data are expressed as mean ± standard deviation or as median and interquartile range, when appropriate. Categorical variables were expressed as percentages. Inter-group comparisons were made using the chi-square test with qualitative variables. On the other hand, the Student t test, Mann-Whitney U test or Wilcoxon test were used, when appropriate, with continuous variables. The long-term event-free survival curves for the different analyses and groups were obtained using the Kaplan-Meier method. In them, the inter-group comparisons were performed using the log-rank test.
Based on the principle of parsimony, multivariable models were used in which, to avoid ann excess of variables in the analysis, only those with P values ≤ .10 were included in the univariate study that will be further explained later. Both the hazard ratio (HR) and the confidence intervals were estimated at 95% (95%CI) based on a Cox logistic regression model with backward elimination (Wald). Two-tailed P values < .05 were considered statistically significant.
RESULTS
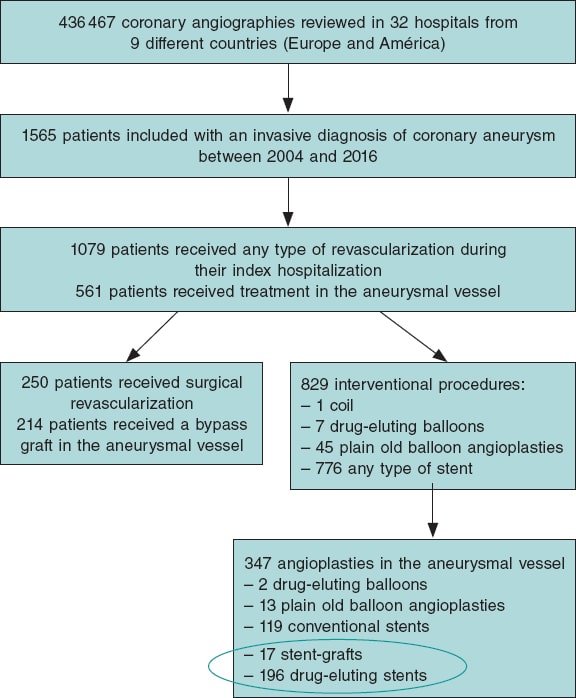
Out of a total of 1565 patients eventually considered in the global registry, 250 were referred for coronary artery surgery and 829 to receive some type of percutaneous revascularization.5 A total of 17 of these patients received, at least, 1 stent-graft to treat their coronary aneurysm. Also, 196 patients received a drug-eluting stent in the aneurysmal area. Therefore, the 17 and 196 patients mentioned before were included in the subsequent analyses of this study. Figure 1 shows the flow of patients.
Figure 1. Flow of the registry patients. The devices encircled in an oval were analyzed in this study. In the stent-graft group it was studied whether patients received a device of this type regardless of other devices.
Approximately, 8% of the patients specifically treated in the aneurysmal area received a stent-graft. Table 1 shows the clinical and angiographic characteristics, and the long-term events of both patients who received stent-grafts and those who received drug-eluting stents. Males were predominant and often showed signs of dyslipidemia, previous coronary arteriopathy, coronary artery disease with previous revascularization, and giant aneurysms in the cohort implanted with stent-grafts. The frequency and type of complications reported at the long-term follow-up with an overall median follow-up of 38 months are shown on table 1. No statistically significant differences were seen at the follow-up regarding the clinical events. A composite event rate of major adverse cardiovascular events (MACE) of 29.6% was reported in patients treated with drug-eluting stents compared to 23.5% in those treated with stent-grafts. Individually, the most common event reported in the group implanted with stent-grafts was unstable angina (11.8%). In the group treated with drug-eluting stents, the most common event was unstable angina (10.2%) and death (10.2%). Every individual event is shown on table 1.
Table 1. Overall characteristics of patients treated with stent-grafts compared to those treated with drug-eluting stents as first-line therapy for the management of coronary aneurysms
| Patients | Stent-graft (N = 17) | Drug-eluting stent (N = 196) | P |
|---|---|---|---|
| Clinical characteristics | |||
| Age, years | 61.47 ± 13.8 | 63.84 ± 12.8 | .467 |
| Sex, male | 16 (94.1) | 146 (74.5) | .069 |
| Arterial hypertension | 11 (64.7) | 142 (72.4) | .496 |
| Dyslipidemia | 15 (88.2) | 119 (60.7) | .024 |
| Diabetes | 3 (17.6) | 58 (29.6) | .296 |
| Smoking habit | .218 | ||
| Active smoker | 10 (58.8) | 82 (41.8) | |
| Former smoker | 3 (17.6) | 25 (12.8) | |
| Family history of coronary arteriopathy | 7 (41.2) | 14 (7.1) | < .001 |
| Kidney disease (CrCl < 30) | 1 (5.9) | 14 (7.1) | .846 |
| Peripheral vasculopathy | 1 (5.9) | 18 (9.2) | .647 |
| Aortopathy – aneurysms | 1 (5.9) | 6 (3.1) | .531 |
| Atrial fibrillation | 1 (5.9) | 7 (3.6) | .631 |
| Connective tissue disease | 0 | 3 (1.5) | .607 |
| LVEF | 56.8 ± 6.1 | 55.6 ± 11.4 | .657 |
| Previous revascularization | 8 (47.0) | 41 (20.9) | .014 |
| Angiographic characteristics | |||
| Right dominance | 14 (82.4) | 166 (84.7) | .641 |
| Serious coronary stenoses | 15 (88.2) | .132 | |
| 1 vessel disease | 4 (23.5) | 62 (31.6) | |
| 2-vessel disease | 6 (35.3) | 68 (34.7) | |
| 3-vessel disease | 5 (29.4) | 62 (31.6) | |
| Location of the aneurysma | |||
| Left main coronary artery | 0 | 3 (1.5) | .607 |
| LAD | 7 (41.2) | 125 (63.8) | .066 |
| LCX | 4 (23.5) | 49 (25) | .893 |
| RCA | 6 (35.3) | 53 (27.0) | .466 |
| Type of aneurysmb | .450 | ||
| Fusiform | 5 (29.4) | 85 (43.8) | |
| Saccular | 12 (70.6) | 107 (55.2) | |
| Giant aneurysm | 3 (17,6) | 5 (2,6) | .02 |
| Number of aneurysms per patient | .940 | ||
| 1 | 15 (88.2) | 155 (79.1.2) | |
| 2 | 2 (6.3) | 30 (15.3) | |
| 3 | 0 | 6 (3.1) | |
| 4 or more | 0 | 5 (2.5) | |
| Indication for catheterization, acute | 11 (64.7) | 144 (73.5) | .436 |
| Indication for catheterization | .179 | ||
| STEACS | 6 (35.3) | 49 (25.0) | |
| NSTEACS | 4 (23.5) | 91 (46.4) | |
| Heart failure | 1 (5.9) | 2 (1) | |
| Stable angina | 6 (35.3) | 32 (16.3) | |
| Other | 0 | 22 (11.2) | |
| Type of stent | – | ||
| Aneugraft | 4 (23.5) | ||
| Jostent-graftmaster | 11 (64.7) | ||
| Papyrus | 1 (5.9) | ||
| Undetermined stent-graft | 1 (5.9) | ||
| ABSORB | 2 (1.0) | ||
| ACTIVE | 28 (14.3) | ||
| BIOFREEDOM | 1 (0.5) | ||
| BIOMATRIX | 4 (2.0) | ||
| COMBO | 2 (1.0) | ||
| COROFLEX | 1 (0.5) | ||
| CRE8 | 8 (4.1) | ||
| CYPHER | 3 (1.5) | ||
| GENOUS | 1 (0.5) | ||
| JANUS | 2 (1.0) | ||
| NO ESPECIF | 8 (4.1) | ||
| ONYX | 1 (0.5) | ||
| ORSIRO | 3 (1.5) | ||
| PROMUS | 20 (10.2) | ||
| RESOLUTE | 23 (11.7) | ||
| STENTYS | 6 (3.1) | ||
| SYNERGY | 12 (6.1) | ||
| XIENCE | 47 (24.0) | ||
| TAXUS | 22 (11.2) | ||
| YUKON | 2 (1.0) | ||
| Size of the stent-graft, medians | |||
| Diameter | 3.5 (3.5-4.0) | 3.5 (3.0-3.75) | .336 |
| Length | 18.0 (16.0-26.0) | 20.0 (15.0-28.0) | .014 |
| Intracoronary imaging modalities | |||
| IVUS | 5 (29.4) | 19 (9.7) | .014 |
| OCT | 1 (5.9) | 7 (3.6) | .631 |
| Any or both | 6 (35.3) | 26 (13.3) | .015 |
| Follow-up | |||
| Median follow-up, months | 29.9 (2.33-51.54) | 46.95 (11.92-76.75) | .093 |
| Dual antiplatelet therapy at discharge | 17 (100) | 193 (99.5) | .767 |
| Duration of dual antiplatelet therapy, median | 12.0 (11.0-12.0) | 12 (12.0-12.0) | .372 |
| Oral anticoagulation/new indication | 2/0 | 9/0 | |
| Adverse events | |||
| Heart failure | 0 | 3 (1.5) | .607 |
| Unstable angina | 2 (11.8) | 20 (10.2) | .839 |
| Reinfarction | 1 (5.9) | 16 (8.2) | .739 |
| Clinically relevant bleeding | 1 (5.9) | 8 (4.1) | .723 |
| Embolism | 0 | 1 (0.5) | .768 |
| Stroke | 0 | 2 (1) | .676 |
| Dead | 0 | 20 (10.2) | .166 |
| All of the above or complicated aneurysm (MACE) | 4 (23.5) | 58 (29.6) | .598 |
| Coronary angiography at the follow-up | 8 (47.0) | 61 (31.1) | .187 |
| Control | 3 (17.6) | 16 (8.2) | |
| Stable angina | 3 (17.6) | 6 (3.1) | |
| NSTEACS | 2 (11.8) | 25 (12.8) | |
| STEACS | 0 | 6 (3.1) | |
| Other | 0 | 8 (4.0) | |
| Aneurysmal complications on the angiographyc | |||
| Growth | 0 | 7 (11.5) | .312 |
| New aneurysms | 0 | 3 (4.9) | .521 |
| Thrombosis | 0 | 6 (9.8) | .353 |
| In-stent restenosis | 1 (12.5) | 0 | .005 |
|
Cr, creatinine; IVUS, intravascular ultrasound; LAD, left anterior descending coronary artery; LCX, left circumflex artery; LVEF, left ventricular ejection fraction; MACE, major adverse cardiovascular events; NSTEACS, non-ST-segment elevation acute coronary syndrome; OCT, optical coherence tomography; RCA, right coronary artery; STEACS, ST-segment elevation acute coronary syndrome. Data are expressed as no. (%) or mean ± standard deviation. a There are more aneurysms than patients because the same patient can have several aneurysms. b Aneurysm was categorized as mixed (fusiform and saccular) in 2 patients. c Statistics is performed on a lower N, only in those with a coronary angiography at the follow-up. |
|||
Coronary angiographies at the follow-up became available for 69 patients (32.4%). Eight of them were performed in the group with stent-grafts and only 1 confirmed failed stent implantation due to in-stent restenosis. In the group treated with drug-eluting stents, the aneurysm grew bigger or new aneurysms appeared in over 15% of the patients with follow-up coronary angiographies available. The rate of thrombosis in this selected group reached 9.8%. Table 2 provides an overall comparison between patients with the composite endpoint of MACE and those without it.
Table 2. Clinical and angiographic characteristics of patients depending on whether they showed, at least, 1 major adverse cardiovascular event at the follow-upa
| Patients | Without events (N = 151) | Some MACE (N = 62) | P |
|---|---|---|---|
| Clinical characteristics | |||
| Age, years | 62.99 ± 12.37 | 65.29 ± 13.93 | .234 |
| Sex, make | 115 (76.2) | 47 (75.8) | .956 |
| Arterial hypertension | 107 (70.9) | 456 (74.2) | .623 |
| Dyslipidemia | 93 (61.6) | 41 (66.1) | .533 |
| Diabetes | 39 (25.8) | 22 (35.5) | .157 |
| Smoking habit | .808 | ||
| Active smoker | 64 (42.4) | 28 (30.4) | |
| Former smoker | 19 (12.6) | 9 (14.5) | |
| Family history of coronary arteriopathy | 17 (11.3) | 4 (6.5) | .285 |
| Kidney disease (CrCl < 30) | 8 (5.3) | 7 (11.3) | .120 |
| Peripheral vasculopathy | 9 (6.0) | 10 (16.1) | .018 |
| Aortopathy – aneurysms | 3 (2.0) | 4 (6.5) | .097 |
| Atrial fibrillation | 5 (3.3) | 3 (4.8) | .594 |
| Connective tissue disease | 0 | 3 (4.8) | .006 |
| LVEF | 56.62 ± 9.74 | 53.67 ± 13.44 | .080 |
| Previous revascularization | 36 (23.8) | 13 (21.0) | .651 |
| Angiographic characteristics | |||
| Right dominance | 127 (84.1) | 53 (85.5) | .237 |
| Serious coronary stenoses | 147 (97.4) | 60 (96.8) | .817 |
| 1 vessel disease | 47 (31.1) | 19 (30.6) | |
| 2-vessel disease | 52 (34.4) | 22 (35.5) | |
| 3-vessel disease | 48 (31.8) | 19 (30.6) | |
| Location of the aneurysmb | .429 | ||
| Left main coronary artery | 3 (2.0) | 0 | |
| LAD | 88 (58.3) | 44 (71) | |
| LCX | 41 (27.2) | 12 (19.4) | |
| RCA | 41 (27.2) | 18 (29.0) | |
| Type of aneurysmc | .676 | ||
| Fusiform | 62 (41.1) | 28 (45.2) | |
| Saccular | 86 (57.0) | 33 (53.2) | |
| Giant aneurysm | 4 (2.6) | 4 (6.5) | .185 |
| Number of aneurysms per patient | |||
| 1 | 122 (80.8) | 48 (77.4) | |
| 2 | 20 (13.2) | 12 (19.4) | |
| 3 | 6 (4.0) | 0 | |
| 4 or more | 3 (2.0) | 2 (3.2) | |
| Indication for catheterization, acute | 101 (66.9) | 54 (87.1) | .002 |
| Indication for catheterization | .053 | ||
| STEACS | 38 (25.1) | 17 (27.4) | |
| NSTEACS | 61 (40.4) | 34 (54.8) | |
| Heart failure | 2 (1.3) | 1 (1.6) | |
| Stable angina | 33 (21.8) | 5 (8.1) | |
| Other | 17 (11.2) | 5 (8.1) | |
| Type of stent | .598 | ||
| Stent-graft | 13 (8.6) | 4 (6.5) | |
| Drug-eluting stent | 138 (91.4) | 58 (93.5) | |
| Size of the stent-graft, medians | |||
| Diameter | 3.38 (3.0-4.0) | 3.28 (3.0-3.5) | .521 |
| Length | 22.00 (15.0-28.0) | 21.74 (15.0-25.0) | .843 |
| Intracoronary imaging modalities | |||
| IVUS | 17 (11.3) | 7 (11.3) | .995 |
| OCT | 8 (5.3) | 0 | .065 |
| Median follow-up, months | 34.0 (12.0-76.0) | 46.93 (18.75-79.75) | .646 |
|
CD: coronaria derecha; CX: circunfleja; Cr: creatinina; DA: descendente anterior; FEVI: fracción de eyección del ventrículo izquierdo; IVUS: ecocardiografía intravascular; MACE: eventos adversos cardiovasculares mayores; OCT: tomografía de coherencia óptica; SCACEST: síndrome coronario agudo con elevación del segmento ST; SCASEST: síndrome coronario agudo sin elevación del segmento ST. Los datos se expresan como n (%) o media ± desviación estándar. a Se consideró como MACE el combinado de muerte de cualquier causa, ingreso por insuficiencia cardiaca, angina inestable, reinfarto, ictus, embolia sistémica, sangrado que precisó atención médica o cualquier complicación del aneurisma (crecimiento, nuevo aneurisma, reestenosis o trombosis). b Hay más aneurismas que pacientes, porque cada enfermo puede presentar varios. c En varios pacientes (3 y 1, respectivamente) el aneurisma fue considerado mixto. |
|||
The multivariate analysis on the occurrence of MACE included in the model the use of stent-grafts. On the other hand, the univariate analysis included variables with P values ≤ .10. All of them are shown on table 2 including the presence or not, of peripheral vasculopathy (on therapy), previous diagnosis of aneurysm (in a territory different from the coronary one), diagnosed connective tissue disease, left ventricular ejection fraction, use of intracoronary imaging modalities (optical coherence tomography or intravascular ultrasound), and acute indication to perform index catheterization.
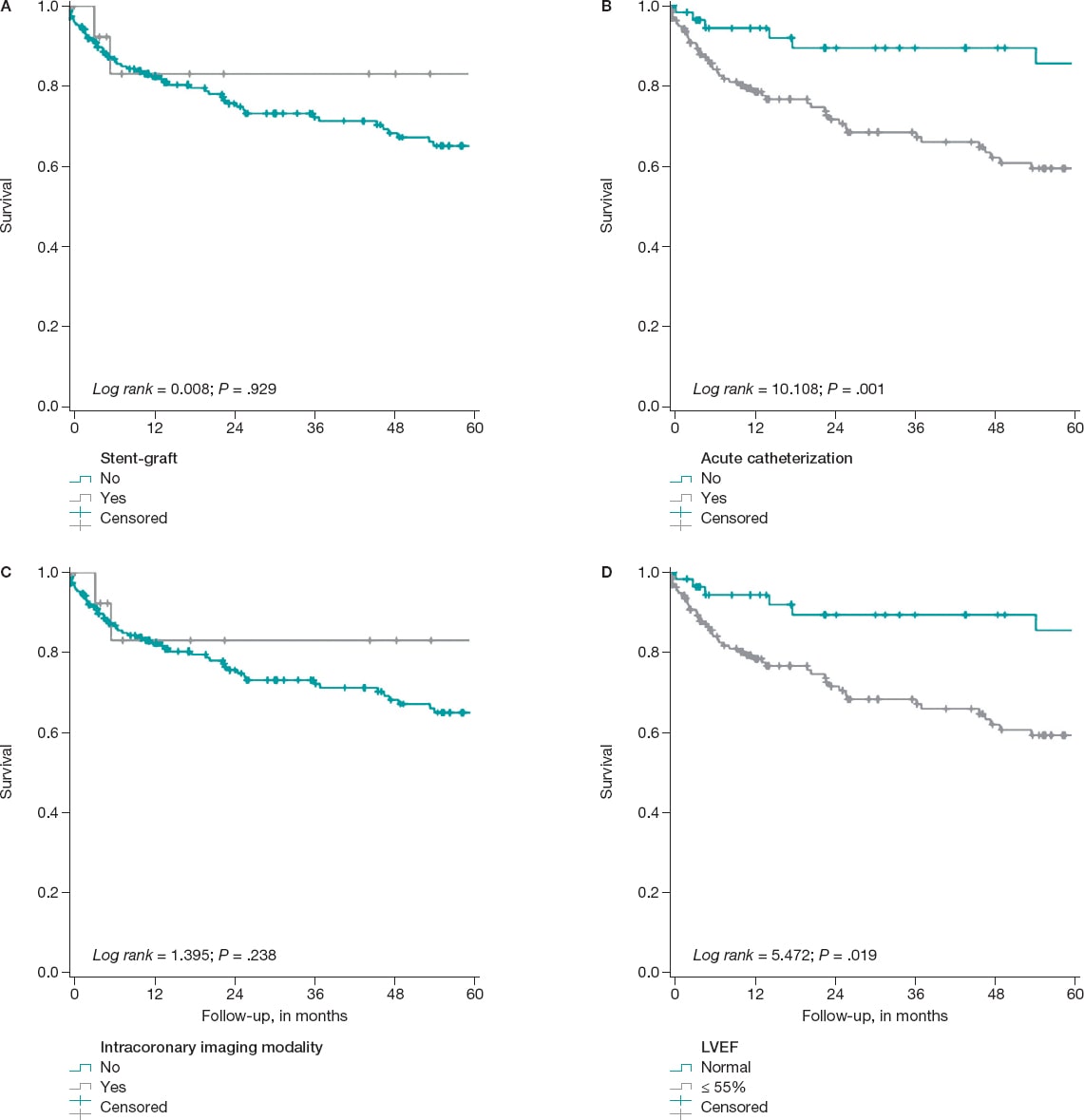
It was confirmed that the following variables remain in the model as independent predictors of the development of the composite endpoint: the existence of connective tissue disease (HR, 5.94; 95%CI, 1.82-19.37), left ventricular dysfunction—below 55%—(HR, 1.84; 95%CI, 1.09-3.1), and the acute indication for index catheterization (HR, 2.98; 95%CI, 1.39-6.3) (figure 2). The use of intracoronary imaging modalities—more common in the cohort implanted with stent-grafts—reached differences that were not statistically significant in the multivariate analysis. It was not a discriminator either regardless of the use of stent-grafts or drug-eluting stents (table 1, table 2, and figure 2).
Figure 2. Kaplan Meier survival curves free of the composite MACE event. A: on the use, or not of the stent-graft for the management of the aneurysm. B: based on whether the indication for index catheterization was acute (acute coronary syndrome, heart failure, etc.). C: regarding the use, during the angioplasty, of any of these intracoronary imaging modalities (intravascular ultrasound, optical coherence tomography or both), D: stratification based on the left ventricular ejection fraction (LVEF) when the angioplasty was performed.
DISCUSSION
This analysis is one of the largest series of coronary aneurysms published including data from real-life patients. It compares 2 of the most widely used therapeutic strategies in this context,5 and its main findings are:
a) The most widely used revascularization method in patients with coronary aneurysms was percutaneous.
b) The exclusion technique, that is, the use of stent-grafts, was used in a relatively lower number of cases (8%).
c) The clinical profile of patients treated with drug-eluting stents was similar compared to patients treated with stent-grafts. However, the presence of giant aneurysms is more common in the latter group. Also, it is probably one of the factors that operators pay most attention to when choosing one stent over the other.
d) An acute indication for the index catheterization and the presence of ventricular dysfunction, at that particular moment, are independent factors of poor prognosis in the study cohort.
e) In the long-term, a similar safety and efficacy profile can be seen in both arms of treatment making stent-grafts a reasonable alternative in selected cases with coronary aneurysms.
The specific treatment of patients with coronary aneurysms has not been well-defined yet to the point that it is not even quoted by the international clinical guidelines on revascularization.5 Over the last few years, several series and registries have been published trying to shed light on this issue.5,6,8,11 Generally speaking, coronary aneurysm is a rare coronary comorbidity. Nonetheless, the average interventional cardiologist sees 1 or several cases each year in his cath lab.7,16 As a matter of fact, in our own experience its estimated that its incidence rate is around 0.35% according to over 430 000 coronary angiographies performed,5 and around 1% according to a recent Chinese series of a little over 11 000 coronary angiographies.17 For this reason, it is important to have clinical data available to guide the management of this entity.7
Also, the coronary aneurysm is a clear marker of anatomic complexity and in adult patients it is suggestive of extensive coronary artery disease, and possibly, poor prognosis compared to milder forms of coronary arteriopathy.7 In previous analyses, the use of drug-eluting stents in patients with coronary aneurysms has been proposed as a therapeutic option clearly superior to conventional stents.5 That is why—as it happens with the rest of patients with ischemic heart disease—this type of platforms is widely recommended for patients with coronary aneurysms. Similarly, the use of an intense and thorough antithrombotic therapy is probably associated with fewer evolutionary complications, which is really reasonable considering the already mentioned high ischemic risk of these patients.11,18
The use of stent-grafts has been proposed as an alternative that can restore the anatomy of the blood vessel. Although the early design of these stents originally served other purposes, the data supporting the feasibility of their use with a high rate of success are extensive.8 In our series, the stent most widely used was the classically designed Jostent Graftmaster coronary stent graft system (Abbott Vascular, United States) (nearly 65%). It is composed of a PTFE layer between 2 stainless-steel stents that may have influenced the results. As a matter of fact, in our setting, Jurado-Román et al.15 conducted a multicenter registry on a certain state-of-the-art stent-graft. They proved that, in several real-life indications, the rate of events is reasonable (MACE, 7.1% at an average 22 months). However, the rate of stent thrombosis was slightly higher (3%) compared to the rate reported by drug-eluting stents in common uses.
The use of intracoronary imaging modalities to perform angioplasties in patients with coronary aneurysms possibly has prognostic implications as it happens in other complex clinical situations (diagnostic doubts, left main coronary artery, bifurcations). In this series, although they were more widely used in the group with stent-grafts implanted, no statistically significant differences were seen on the development of MACE (figure 2). This possibly has to do with the size of the study sample. Also, a tendency was seen towards fewer events in the group of patients with procedures optimized through intracoronary imaging guidance whether intravascular ultrasound or optical coherence tomography.
Limitations
This study has limitation associated with the particular design of the study. Also, a relatively small number of participants was included, which may have complicated the detection of differences in the analyses due to the lack of statistical power. The decision to implant stent-grafts or drug-eluting stents was entirely left to each patient’s medical team, which may have been associated with a certain degree of heterogeneity in the protocols that could have also been more dynamic in time. At the very complete follow-up from the clinical standpoint, control angiographies became available for a limited number of patients only (32%) who met the criterion set by the treating physicians. This may have underestimated the rate of complications, especially the subclinical ones, or be associated with selection biases in both groups.
However, this study is an approach to real-life clinical practice for a relatively rare heart disease on which there is little information available. It also includes a long-term clinical follow-up.
CONCLUSIONS
Stents-grafts can be used to treat coronary aneurysms and are safe in the long-term. Randomized clinical trials are needed to decide what the best treatment is for this type of complex coronary lesions.
FUNDING
None.
AUTHORS’ CONTRIBUTIONS
I. J. Núñez-Gil, CAAR coordinator: study design, data analysis, and draft writing. E. Cerrato, M. Bollati, L. Nombela-Franco, and A. Fernández-Ortiz: study design. E. Cerrato, M. Bollati, B. Terol, E. Alfonso-Rodríguez, S. J. Camacho-Freire, P. A. Villablanca, I. J. Amat-Santos, J.M. de la Torre-Hernández, I. Pascual, C. Liebetrau, B. Camacho, M. Pavani, R. A. Latini, F.Varbella, V. A. Jiménez Díaz, D. Piraino, MM, F. Alfonso, J. Antonio Linares, J. M. Jiménez-Mazuecos, J. Palazuelos- Molinero, and I. Lozano: data mining and recruitment. E. Cerrato, M. Bollati, B. Terol, L. Nombela-Franco, E. Alfonso-Rodríguez, S. J. Camacho-Freire, P. A. Villablanca, I. J. Amat-Santos J.M. de la Torre-Hernández, I. Pascual, C. Liebetrau, B. Camacho, M. Pavani, R. A. Latini, F.Varbella, V. A. Jiménez Díaz, Davide Piraino, M. Mancone, F. Alfonso, J. A. Linares, J. M. Jiménez-Mazuecos, J. Palazuelos- Molinero, IÍ. Lozano, and A. Fernández-Ortiz: reading and critical review of the manuscript.
CONFLICTS OF INTEREST
J. M. de la Torre Hernández is the editor-in-chief of REC: Interventional Cardiology, and F. Alfonso is an associate editor of this journal. The journal’s editorial procedure to ensure impartial handling of the manuscript has been followed. No other conflicts of interest have been declared whatsoever.
WHAT IS KNOWN ABOUT THE TOPIC?
- Coronary aneurysms are a complex entity whose incidence rate is between 0.3 and 12% in the different series already published.
- Treatment, like the presentation and the clinical profile, is varied. However, revascularization is often required.
- In this sense, over the last few years, some of the alternatives available propose the use of stent-grafts for the exclusion of coronary aneurysms.
WHAT DOES THIS STUDY ADD?
- The main goal of this paper was to describe the frequency of use of this type of stents to treat coronary aneurysms and then characterize its long-term results.
- From a total of 829 patients with coronary aneurysms treated with some type of percutaneous revascularization, data on the use of stent-grafts and drug-eluting stents was collected in 17 and 196 patients, respectively.
- It seems obvious that patients treated with stent-grafts for the management of coronary aneurysms have a high ischemic load, often complex anatomies, and even more often giant aneurysms.
- The use of stent-grafts for the management of coronary aneurysms is feasible and safe in the long-term. However, randomized clinical trials are still needed to decide what the best therapy is for this type of complex coronary lesions.
REFERENCES
1. Bourgon A. Biblioth Med. 1812;37:183. Citado por Scott DH. Aneurysm of the coronary arteries. Am Heart J. 1948;36:403-421.
2. Packard M, Wechsler H. Aneurysms of coronary arteries. Arch Intern Med. 1929;43:1-14.
3. Swaye PS, Fisher LD, Litwin P, et al. Aneurysmal coronary artery disease. Circulation. 1983;67:134-138.
4. Cohen P, O'Gara PT. Coronary artery aneurysms:a review of the natural history, pathophysiology, and management. Cardiol Rev. 2008;16:301-304.
5. Núñez-Gil IJ, Cerrato E, Bollati M, et al. Coronary artery aneurysms, insights from the international coronary artery aneurysm registry (CAAR). Int J Cardiol. 2020;299:49-55.
6. Núñez-Gil IJ, Terol B, Feltes G, et al. Coronary aneurysms in the acute patient:Incidence, characterization and long-term management results. Cardiovasc Revasc Med. 2018;19(5 Pt B):589-596.
7. Kawsara A, Núñez Gil IJ, Alqahtani F, Moreland J, Rihal CS, Alkhouli M. Management of Coronary Artery Aneurysms. JACC Cardiovasc Interv. 2018;11:1211-1223.
8. Will M, Kwok CS, Nagaraja V, et al. Outcomes of patients who undergo elective covered stent treatment for coronary artery aneurysms. Cardiovasc Revasc Med. 2021:S1553-8389(21)00264-5.
9. Núñez-Gil IJ, Alberca PM, Gonzalo N, Nombela-Franco L, Salinas P, Fernández-Ortiz A. Giant coronary aneurysm culprit of an acute coronary syndrome. Rev Port Cardiol (Engl Ed). 2018;37:203.e1-203.e5.
10. Cha JJ, Kook H, Hong SJ, et al. Successful Long-term Patency of a Complicated Coronary Aneurysm at a Prior Coronary Branch Stent Treated with a Stent-graft and Dedicated Bifurcation Stent. Korean Circ J. 2021;51:551-553.
11. Khubber S, Chana R, Meenakshisundaram C, et al. Coronary artery aneurysms:outcomes following medical, percutaneous interventional and surgical management. Open Heart. 2021;8:e001440.
12. Arbas-Redondo E, Jurado-Román A, Jiménez-Valero S, Galeote-García G, Gonzálvez-García A, Moreno-Gómez R. Acquired coronary aneurysm after stent implantation at a bifurcation excluded with a Papyrus covered stent subsequently fenestrated. Cardiovasc Interv Ther. 2022;37:215-216.
13. Della Rosa F, Molina-Martin de Nicolas J, Bonfils L, Fajadet J. Symptomatic giant coronary artery aneurysm treated with covered stents. Coron Artery Dis. 2020;31:658-659.
14. Tehrani S, Faircloth M, Chua TP, Rathore S. Percutaneous coronary intervention in coronary artery aneurysms;technical aspects. Report of case series and literature review. Cardiovasc Revasc Med. 2021;28S:243-248.
15. Jurado-Román A, Rodríguez O, Amat I, et al. Clinical outcomes after implantation of polyurethane-covered cobalt-chromium stents. Insights from the Papyrus-Spain registry. Cardiovasc Revasc Med. 2021;29:22-28.
16. Núñez-Gil IJ, Nombela-Franco L, Bagur R, et al. Rationale and design of a multicenter, international and collaborative Coronary Artery Aneurysm Registry (CAAR). Clin Cardiol. 2017;40:580-585.
17. Jiang X, Zhou P, Wen C, et al. Coronary Anomalies in 11,267 Southwest Chinese Patients Determined by Angiography. Biomed Res Int. 2021;2021:6693784.
18. D'Ascenzo F, Saglietto A, Ramakrishna H, et al. Usefulness of oral anticoagulation in patients with coronary aneurysms:Insights from the CAAR registry. Catheter Cardiovasc Interv. 2021;98(5):864-871.